THEME: Community Orientation in Primary Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Match Report
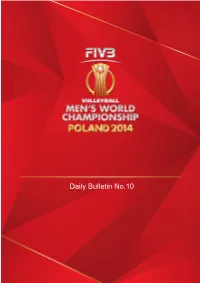
Daily Bulletin No.10 VOLLEYBALL • Match result FIVB Men's Volleyball World Championship 2014 Pool E Match: 61 Date: 10.09.2014 Spectators: 10'600 Teams Sets 1 2 3 4 5 Total City: LODZ POL 1 27 22 27 23 99 Hall: ATLAS ARENA USA 3 29 25 25 25 104 Match duration: Start: 20:25 End: 22:51 Total: 2:26 Set duration 0:37 0:28 0:35 0:30 2:10 Referees: ALI Jafaar (BRN) & BOUDAYA Taoufik (TUN) POL • Poland 12345 Pts USA • USA 12345 Pts 1 Nowakowski Piotr 5 1 Anderson Matthew 21 2 Winiarski Michal 14 3 Sander Taylor 23 3 Konarski Dawid 4 Lee David 11 5 Zagumny Pawel 1 6 Lotman Paul 4 7 Klos Karol 10 7 Shoji Kawika 10 Wlazly Mariusz 17 10 Ciarelli Antonio 11 Drzyzga Fabian 11 Christenson Micah 5 13 Kubiak Michal 12 15 Clark Carson 17L Zatorski Pawel LLLL 17 Holt Maxwell 15 18 Mozdzonek Marcin 4 19L Reft Alfredo 20 Mika Mateusz 20 Smith David 21 Buszek Rafal 22L Shoji Erik LLLL Coach: ANTIGA Stephane (FRA) Coach: Speraw, John (USA) Assistant: BLAIN Philippe (FRA) Assistant: Fuerbringer, Matthew (USA) TEAMS AND PLAYERS PERFORMANCES Won Total Scoring Won Total No Name No Name Pts Atts Skills Pts Atts 50 106 Total Team 61 128 Total Team 16 29 10 Wlazly Mariusz 20 45 1 Anderson Matthew Spike 11 29 2 Winiarski Michal 19 34 3 Sander Taylor 10 22 13 Kubiak Michal 10 17 17 Holt Maxwell 11 98 Total Team 14 85 Total Team 3 19 7 Klos Karol 3 13 11 Christenson Micah Block 2 16 2 Winiarski Michal 3 8 3 Sander Taylor 2 14 18 Mozdzonek Marcin 3 20 4 Lee David 2 100 Total Team 4 103 Total Team 1 18 2 Winiarski Michal 2 18 17 Holt Maxwell Serve 1 14 13 Kubiak Michal 1 18 3 Sander Taylor 1 17 11 Christenson Micah 36 Total Team Opp. -

November 2008
November 2008 S port is life Cor de Maria – Maria Reina AAArrrtttiiicccllleeesss page 3 Interviews page 13 News page 29 Report page 36 Fun Section page 36 First issue game solutions page 49 Basketball and health benefits asketball is one of the ª Build endurance most popular sports in ª Develop concentration Some general tips the world and one of ª Build up muscle. B the most widely viewed. It is a team sport that involves two Other benefits ª Adults should check with teams of five active players their doctor before taking each trying to score points up basketball. As well as being a great way against one another by ª Be aware that basketball is throwing a ball through a to stay fit, basketball can also: a fast-action game with lots 300cm (10 foot) high hoop of running, jumping, (the ‘basket’) under organised ª Help you to make new pivoting and twisting, so rules. friends and see them regularly injuries and accidents can ª Teach you about being a happen easily. good team player Basketball involves a lot of ª Basketball puts a lot of variety including shooting, ª Be played by people of all stress on the legs, especially dribbling, passing, rebounding, ages and all abilities the knees and ankles, and defence and much more. ª Be played all year round puts pressure on tight because it’s usually an indoor shoulders. sport Health benefits ª Protect yourself by ª Be a fun game that kids of becoming strong and Basketball involves a lot of all levels and ages can enjoy. -

Православните Патриарси Orthodox Patriarchs 8
WELCOME NOTE Dear Passengers, Welcome aboard Bulgaria Air! Goethe called architecture “frozen music”. To Constantin Brancusi it was “inhabited sculpture". Even the imperturbable Sir Winston Churchill conceded its importance: "We shape our buildings; thereafter they shape us." Янко Георгиев, Изпълнителен директор Initially starting as a means to protect Yanko Georgiev, Executive Director against the elements, even millennia ago architecture became something much more than that: a factor which determines not only our Уважаеми пътници, way of life, but our mentality as well. And is now Добре дошли на борда на България Ер! about to climb the next step. The architecture of the future won’t consist only in the creation of efficient and comfortable Гьоте наричаше архитектурата "замръзнала музика". За buildings – it will become a much broader Константин Брънкуш тя е "обитаема скулптура". Дори discipline, closely related to things like energy, невъзмутимият сър Уинстън Чърчил признаваше значимостта й: economics and social sciences. And will shape "Ние оформяме нашите сгради; след това те оформят нас". not only our individual homes, but our whole cities, with well-thought-out and targeted efforts. This is the only way to solve problems such as Започнала някога като средство да се нето и глобалното затопляне. В новия resource shortage, pollution and global warming. предпазим от стихиите, още преди хиля- брой на THE INFLIGHT MAGAZINE ще ви The new issue of THE INFLIGHT MAGAZINE долетия архитектурата се е превърнала в представим петима архитекти, които със presents five architects who are bound to play нещо много повече от това: във фактор, сигурност ще играят водеща роля в тази an important role in this transformation. -

RUSE and VARNA, BULGARIA POOLS B and D
RUSE AND VARNA, BULGARIA POOLS B and D Bulletin 3 10/09/2018 1 FIVB Volleyball Men's World Championship O-2bis Team registration BRA - Brazil Weight Height Highest reach [cm] National selections Shirt no Last name First name Shirt name Pos. Birthdate Club [kg] [cm] Spike Block WC OG Oth. Tot. 1 C Rezende Bruno Mossa Bruno S 02-Jul-1986 76 190 323 302 Lube 7 2 20 29 2 Santos Isac Isac MB 13-Dec-1990 99 208 339 306 Sada Cruzeiro - - 8 8 3 Carbonera Eder Eder MB 19-Oct-1983 107 205 360 330 SESI-SP 3 - 5 8 5 Loh Lucas Eduardo Lucas Loh WS 18-Jan-1991 83 195 336 320 SESI-SP - - - - 7 Arjona William William S 31-Jul-1979 78 186 300 295 SESI-SP - 1 - 1 8 De Souza Wallace Wallace OP 26-Jun-1987 87 198 344 318 SESC-RJ 14 1 37 52 9 Hoss Thales Thales L 26-Apr-1989 74 190 320 303 Funvic Taubaté - - - - 12 Fonteles Luiz Felipe Marques Lipe WS 19-Jun-1984 100 198 351 340 SESI-SP 13 - 37 50 13 Souza Maurício M. Souza MB 29-Sep-1988 93 209 344 323 SESC-RJ - - - - 14 Souza Douglas Douglas WS 20-Aug-1995 75 199 338 317 Funvic Taubaté - - - - 15 Barreto Silva Carlos Eduardo Kadu WS 08-Aug-1994 90 200 348 340 Vibo Valentia 8 - - 8 16 Saatkamp Lucas Lucas MB 06-Mar-1986 101 209 340 321 Funvic Taubaté 16 - 37 53 17 Guerra Evandro M. Evandro OP 27-Dec-1981 106 207 359 332 Sada Cruzeiro 7 - 17 24 22 Reis Nascimento Maique Maique L 16-Jul-1997 76 182 310 255 Minas Tenis Clube - - - - OFFICIALS COLORS STATISTICS Team manager: Fernando Castro Maroni Main: Yellow Data Minimum Average Maximum Head coach: Renan Dal Zotto 2nd: Blue Height: 182 198 209 Assistant coach: -

Political Liberalism in Bulgaria: Achievements and Prospects 1
The definitive ideas of political liberalism – individual rights, constitution- alism, and the market economy – have become universal reference points in democratic politics, and because of that have been largely de-politicised. This situation spells the predicament of the liberal parties: their agenda has become universally accepted, which makes them hardly distinguishable from their main competitors. In Bulgaria, essentially only one party has been successfully institution- alised as ‘liberal’ both in terms of ideology and centrism – NDSV. In terms of positioning, DPS has always been centrist, but in terms of practiced ideology it could hardly be called ‘liberal’. There are obviously conditions under which ‘liberalism’ as a political ideology could be revived and become successful in electoral contests: the rise of populism in the 2000s also provides an opportunity for liberal parties to consolidate and to create a joint front against attempts to un- dermine constitutional values. The dominance of mild populism of a centrist type prevents for now the possibility of the emergence of a strong, centrist liberal party (or the revival of existing ones). The immediate chances for the revival of the liberal centre depend on the radicalisation of Bulgarian populism in nationalistic or other illiberal di- rection. If aggressive populist governments, as the one of Orban in Hungary, appear one might expect a possible consolidation of a liberal alternative. One wonders whether such a development would be a cause for celebration for liberals, however. Maybe it is ultimately better to be a victim of one’s own success and to see your ideas shared – imperfectly or simply strategically as it may be - by a wide spectrum of parties. -

Volleyball in Europe.Pdf
Kristina M. Pantelić Babić Nenad Živanović Petar D. Pavlović Branislav Antala (Editors) HISTORY OF VOLLEYBALL IN EUROPE FIEP Europe – History of Physical Education and Sport University of Priština, Faculty of Section Sport and Physical Education in Association of Pedagogues of Leposavić Physical Education and Sport FIEP, Niš, Serbia Niš - Leposavić, 2018. FIEP book Edition: History of Physical Education and Sport Book 4 Book: HISTORY OF VOLLEYBALL IN EUROPE Editors: Kristina M. Pantelić Babić (BIH, Republic of Srpska) Nenad Živanović (Serbia) Petar D. Pavlović (BIH, Republic of Srpska) Branislav Antala (Slovakia) Publisher: University of Priština, Faculty of Sport and Physical Education in Leposavić For publisher: Veroljub Stanković Reviewers: Branislav Antala (Slovakia) Kristina M. Pantelić Babić (BIH, Republic of Srpska) Nenad Živanović (Serbia) Nicolae Ochiana (Romania) Petar D. Pavlović (BIH, Republic of Srpska) Sergii Ivashchenko (Ukraine) Slađana Mijatović (Serbia) Sobyanin Fedor Ivanovich (Russia) Veroljub Stanković (Serbia) Violeta Šiljak (Serbia) Zoran Milošević (Serbia) Prepress: Kristina M. Pantelić Babić Book-jacket: SIGRAF Kruševac Circulation: 200 Printed by: SIGRAF Kruševac ISBN 978-86-82329-75-6 NOTE: No part of this publication may be reproduced without the prior permission of the authors. Authors: Arūnas Emeljanovas (Lithuania) Barbaros Çelenk (Turkey) Bernat Buscà Safont-Tria (Spain) Bogacheva Elizaveta Alekseevna (Russia) Bruno Telles Matos (Brazil) Daiva Majauskienė (Lithuania) Daniela Dasheva (Bulgaria) Dejan Milenković -

Bulgaria Brightbright Rreturn...Eturn
5th Bulgaria BrightBright return...return... After a four-year absence from the World League Bulgaria returned in 2003 with astonishing power and precision to claim second place in Pool C and march right into the World League Finals. Naturally strong and tall Bulgaria proved that they have the talent and game plan, which will threaten the international Volleyball big boys for years to come, as they knocked over some big names on their way to just missing Coach Milorad Kijac out on a semifinal place on Set Ratio. However, looking at the opening stanza of their campaign, one would not have realised what was in store. Two losses – including an opening round defeat to Cuba – in their first three games and Bulgaria was doing it tough on their return to the premier men’s annual competition. But a re- markable run of seven wins from eight games, including three over Olympic Champions Serbia and Montenegro and Bulgaria sailed through to the top of Pool C and claimed their ticket to Madrid. Their impressive run continued, to an extent. Drawn in the most formidable of pools, Bulgaria went down to both Brazil and Italy before claiming the scalp of old foes Russia, which eliminated the defending champions from the competition. Following that litmus test Bulgaria have laid their cards on the table illustrating that they are a side who will continue to threaten the pace setters, especially with such tall timber as 210 cm-tall Evgeni Ivanov in their ranks. As their star setter and captain Nikolay Ivanov said after the tourna- ment: “We have shown we can play good Volleyball with the best teams in the world.” Bulgarian captain and setter Nikolay Ivanov Bulgaria were formidable on defense Plamen Konstantinov was one of Bul- 62 World League 2003 Final Report garia’s best attacking weapons Host TV Bulgarian block at its best TEAM NUMBERS PLAYERS Birthdate Height Weight Spike Block CAPS Club No. -

Téléchargez Le Dossier De Presse
LE PROGRAMME DES BLEUS PAGE 3 LE GROUPE FRANCE PAGE 4 LE PALMARES DE L’EQUIPE DE FRANCE PAGE 5 PROGRAMME DE PRÉPARATION AU CHAMPIONNAT DU MONDE PAGE 6 LE CHAMPIONNAT DU MONDE PAGE 7 LES RESULTATS DE LA SAISON 2018 PAGE 10 LES BIOS PAGE 14 LES STATISTIQUES DES MATCHS DE LA SAISON PAGE 38 LE VOLLEY-BALL PAGE 58 CONTACTS PAGE 63 DOSSIER DE PRESSE - EQUIPE DE FRANCE MASCULINE 2018 2 LE PROGRAMME DES BLEUS 11 août : FRANCE / PAYS-BAS (Sète) 24-26 août : TOURNOI WAGNER (Pologne) 2 septembre : FRANCE / SERBIE (Paris) 9-30 septembre : CHAMPIONNAT DU MONDE (Bulgarie / Italie) DOSSIER DE PRESSE - EQUIPE DE FRANCE MASCULINE 2018 3 L’ÉQUIPE DE FRANCE N° NOM Prénom Poste Naissance Club 2018/2019 Taille Poids Attaque Block Sélec. au 1/8/18 2 GREBENNIKOV Jénia Libéro 13/08/90 TRENTE (ITA) 188 85 345 300 241 4 PATRY Jean Pointu 27/12/96 MONTPELLIER VUC 207 94 357 334 40 6 TONIUTTI Benjamin Passeur 30/10/89 ZAKSA KEDZIERZYN-KOZLE (POL) 183 72 320 300 268 7 TILLIE Kevin Récep/Attaquant 02/11/90 PÉKIN (CHI) 200 85 345 325 180 8 LYNEEL Julien Récep/Attaquant 15/04/90 JASTRZĘBSKI WĘGIEL (POL) 192 88 345 325 170 9 NGAPETH Earvin Récep/Attaquant 12/02/91 KAZAN (RUS) 194 96 358 327 234 10 LE ROUX Kevin Central 11/05/89 SADA CRUSEIRO VOLEI (BRE) 209 95 365 345 214 11 BRIZARD Antoine Passeur 15/06/94 AP WARSZAWSKA (POL) 196 96 340 310 54 12 BOYER Stephen Pointu 10/04/96 VERONE (ITA) 196 77 355 334 54 14 LE GOFF Nicolas Central 15/02/92 BERLIN RV (ALL) 206 114 365 345 183 15 MOUIEL Jérémie Libéro 04/05/95 AS CANNES 176 57 290 260 15 16 BULTOR Daryl Central 17/11/95 -

Sofia and Varna, Bulgaria
SOFIA AND VARNA, BULGARIA POOLS G and H Bulletin 14 22/09/2018 TRAVEL SCHEDULE FOR THE TEAMS IN POOLS G AND H: SOFIA AND VARNA, QUALIFIED FOR THE 3rd ROUND Team Date Departure: Teams Hotel Destination 1st Pool G, 2nd Pool G* 24.09 16:30 Sofia Airport 1st Pool H 24.09 14:00 Varna Airport 2nd Pool H* 24.09 12:30 Burgas Airport *if qualified All teams, travelling to Italy have a connecting flight from Sofia, set for takeoff at 19:05 on 24.09.2018. If they do so wish, the qualified teams can use the time before departure for training in the training halls and gyms. FIVB Control Committee Local Organizing Committee Bulgaria 2 FIVB Volleyball Men's World Championship P-4 Collated results & ranking Results as of 22 September 2018 MATCHES RESULTS Pool G Result per set (points) Total No Date Teams Set Duration Spectators 1 2 3 4 5 Points 61 21-Sep-2018 USA - CAN 3-1 25-17 25-14 21-25 25-17 96-73 1:48 650 65 21-Sep-2018 BUL - IRI 3-0 25-19 28-26 26-24 79-69 1:39 7250 69 22-Sep-2018 IRI - CAN 2-3 20-25 25-20 15-25 25-23 12-15 97-108 2:19 600 73 22-Sep-2018 BUL - USA 0-3 20-25 20-25 18-25 58-75 1:33 8400 TEAM RANKING Pool G Matches Results details Sets Points Rk Code Team Pts W L T 3-0 3-1 3-2 2-3 1-3 0-3 W L Ratio W L Ratio 1 USA USA 7 0 7 19 3 2 2 0 0 0 21 6 3.500 627 514 1.219 2 BUL Bulgaria 4 3 7 12 4 0 0 0 2 1 14 9 1.555 532 512 1.039 3 IRI Iran 4 3 7 12 1 2 1 1 0 2 14 13 1.076 603 587 1.027 4 CAN Canada 4 3 7 11 2 1 1 0 3 0 15 12 1.250 607 601 1.009 3 FIVB Volleyball Men's World Championship P-2 Match result Pool G Match: 69 Date: 22/09/2018 Spectators: 600 Teams Sets 1 2 3 4 5 Total City: Sofia IRI 2 20 25 15 25 12 97 Hall: Arena Armeec CAN 3 25 20 25 23 15 108 Match duration: Start: 17:00 End: 19:19 Total: 2:19 Duration: 0:25 0:26 0:25 0:31 0:20 2:07 Referees: Hector Ortiz (PUR) & Nathanon Sowapark (THA) IRI - Iran CAN - Canada Line-up Points by set Line-up Points by set No Name Pos. -

MEDIA GUIDE Men's Tournament 18Th November to 2Nd
www.fivb.org MEDIA GUIDE Men’s Tournament 18th November to 2nd December 2007 www.fivb.org MEDIA GUIDE Men’s Tournament 18th November to 2nd December 2007 Credits Editorial : Fabrizio Rossini - FIVB Press Officer Project Manager : Volleyball Events Department Data : Alberto Rigamonti - FIVB IT Department Layout : Samuel Chesaux Printing : Wakao Printing Co. Ltd., Japan Photos : © FIVB 1 www.fivb.org Table of contents Message from FIVB President 3 General Organisation 5 Qualification Tournaments 6 Competition System 9 FIVB World Ranking 10 Competition Schedules 12 Participants 14 2007 World Cup Host cities 17 Argentina 22 Australia 26 Brazil 30 Bulgaria 34 Egypt 38 Spain 42 Japan 46 Korea, Republic of 50 Puerto Rico 54 Russia 58 Tunisia 62 U.S.A. 66 Men’s World Cup Honours 70 2003 History 71 List of officials 72 OFFICIAL TEAM PRESENTATION AND MEDIA GUIDE 2 MEN FIVB World Cup 2007: the challenge for Beijing 2008 begins One year after the huge success of the FIVB World Championships played in Japan, the Volleyball family was looking forward to coming back here for the FIVB World Cup 2007. Months before the event I had the feeling that something really exciting was going to happen: the FIVB wants a World Cup even more successful than the 2003 edition, which is still a record breaker event. Japan Volleyball Association and Fuji Television Network Inc. are leading the FIVB team to have the best World Cup ever. All the Japanese fans are ready to give their full support to the best players of the planet, gathered in Japan to go for the gold medals and to get a chance to compete at the Olympic Games next year. -
Annual Report on Its Activity
ÿíóàðè 2004 a i n f o o i S Sofia t a AAnnualnnual d MMISSIONISSION n TToo ppromote,romote, u RReporteport hhelpelp o ddevelopevelop F aandnd y ssustainustain t e tthehe i 22003003 vvalues,alues, c aattitudesttitudes o S aandnd IInitiativesnitiatives ppracticesractices n ooff e SSupportedupported tthehe p PProjectsrojects oopenpen O Open Society Foundation ssocietyociety iinn BBulgariaulgaria OOPENPEN SSOCIETYOCIETY FFOUNDATIONOUNDATION SSOFIAOFIA OOPENPEN SSOCIETYOCIETY FFOUNDATIONOUNDATION – SOFIASOFIA 22003003 FFounderounder George Soros BBoardoard ooff TTrusteesrustees Stefan Popov CChairmanhairman Haralan Alexandrov Rumiana Chervenkova Marin Deltchev Yonko Grozev Petia Kabakchieva Georgi Koritarov Vesselin Metodiev Svetlana Vassileva OOmbudsmanmbudsman Prolet Velkova EExecutivexecutive DDirectorirector Rayna Gavrilova FFinancialinancial DDirectorirector Veliko Sherbanov PProgramrogram DDirectorsirectors Ivanka Ivanova Assya Kavrakova Neda Kristanova Cveta Petkova Kalin Tsekov Elena Zlatanova MMISSIONISSION To promote, help develop and sustain the values, attitudes and practices of the open society in Bulgaria SSTRATEGICTRATEGIC GGOALOAL To support Bulgaria’s accession to United Europe by broadening the integration process into the whole public domain TThehe OOpenpen SSocietyociety FFoundationoundation – SSofiaofia iiss rregisteredegistered aass a ppublicublic bbenefitenefit oorganization.rganization. AANNUALNNUAL RREPORTEPORT 22003003 OOPENPEN SSOCIETYOCIETY FFOUNDATIONOUNDATION SSOFIAOFIA Contents 2003: Opportunities and Challenges -
DVV Newsletter Ausgabe 1 Englisch.Indd
#GOlympia Newsletter #3 Key Players in Berlin · Press conference on Monday · Volleyball2016 European Olympic Qualification Key Players (Pool A) All squads in Berlin are filled with major key players that road playing first in Slovenia for ACH Volley and after that can make the difference in important situations. moving to Italy joining MODENA Volley. This summer he moved to Calzedonia VERONA and he has been doing re- Denys Kaliberda, Germany - Outside Spiker ally well so far with the team. Kaliberda is a very important player for Germany. He nee- ded a lot of time to recover from a shoulder injury in 2015 Simon Van de Voorde, Belgium - Middle blocker but is now on the way to getting better and better. His Van de Voorde was the best middle blocker of the Italian smart attack, good service and fast defence reaction ma- League in the last season and changed to Championship kes him the most complete player on the roster of the winner Trentino for the 2015-2016 season. He is one of hosts. the best players on this position and has a very good float service that creates huge problems to the defence of the Mateusz Mika, Poland - Outside Spiker receiving team. The only downside was an open fracture Mika developed to a key player for Poland in the last 12 that he suffered in the last game of the past season but months and is a teammate who can set the pace in all the Belgian giant is on the way back to reaching his top aspects of the game.