Role of Quzhou Fructus Aurantii Extract in Preventing and Treating
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thesis of Potentially Sweet Dihydrochalcone Glycosides
University of Bath PHD The synthesis of potentially sweet dihydrochalcone glycosides. Noble, Christopher Michael Award date: 1974 Awarding institution: University of Bath Link to publication Alternative formats If you require this document in an alternative format, please contact: [email protected] General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal ? Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 05. Oct. 2021 THE SYNTHESIS OF POTBTTIALLY SWEET DIHYDROCHALCOITB GLYCOSIDES submitted by CHRISTOPHER MICHAEL NOBLE for the degree of Doctor of Philosophy of the University of Bath. 1974 COPYRIGHT Attention is drawn to the fact that copyright of this thesis rests with its author.This copy of the the sis has been supplied on condition that anyone who con sults it is understood to recognise that its copyright rests with its author and that no quotation from the thesis and no information derived from it may be pub lished without the prior written consent of the author. -

Treatment Protocol Copyright © 2018 Kostoff Et Al
Prevention and reversal of Alzheimer's disease: treatment protocol Copyright © 2018 Kostoff et al PREVENTION AND REVERSAL OF ALZHEIMER'S DISEASE: TREATMENT PROTOCOL by Ronald N. Kostoffa, Alan L. Porterb, Henry. A. Buchtelc (a) Research Affiliate, School of Public Policy, Georgia Institute of Technology, USA (b) Professor Emeritus, School of Public Policy, Georgia Institute of Technology, USA (c) Associate Professor, Department of Psychiatry, University of Michigan, USA KEYWORDS Alzheimer's Disease; Dementia; Text Mining; Literature-Based Discovery; Information Technology; Treatments Prevention and reversal of Alzheimer's disease: treatment protocol Copyright © 2018 Kostoff et al CITATION TO MONOGRAPH Kostoff RN, Porter AL, Buchtel HA. Prevention and reversal of Alzheimer's disease: treatment protocol. Georgia Institute of Technology. 2018. PDF. https://smartech.gatech.edu/handle/1853/59311 COPYRIGHT AND CREATIVE COMMONS LICENSE COPYRIGHT Copyright © 2018 by Ronald N. Kostoff, Alan L. Porter, Henry A. Buchtel Printed in the United States of America; First Printing, 2018 CREATIVE COMMONS LICENSE This work can be copied and redistributed in any medium or format provided that credit is given to the original author. For more details on the CC BY license, see: http://creativecommons.org/licenses/by/4.0/ This work is licensed under a Creative Commons Attribution 4.0 International License<http://creativecommons.org/licenses/by/4.0/>. DISCLAIMERS The views in this monograph are solely those of the authors, and do not represent the views of the Georgia Institute of Technology or the University of Michigan. This monograph is not intended as a substitute for the medical advice of physicians. The reader should regularly consult a physician in matters relating to his/her health and particularly with respect to any symptoms that may require diagnosis or medical attention. -

Bergamot) Juice Extracted from Three Different Cultivars Vincenzo Sicari*, Teresa Maria Pellicanò (Received December 14, 2015
Journal of Applied Botany and Food Quality 89, 171 - 175 (2016), DOI:10.5073/JABFQ.2016.089.021 Department of Agraria, University “Mediterranea” of Reggio Calabria, Reggio Calabria (RC), Italy Phytochemical properties and antioxidant potential from Citrus bergamia, Risso (bergamot) juice extracted from three different cultivars Vincenzo Sicari*, Teresa Maria Pellicanò (Received December 14, 2015) Summary Bergamot presents a unique profile of flavonoids and flavonoid Secondary substances occurring in plant-derived products possess glycosides in its juice, such as neoeriocitrin, neohesperidin, naringin, biological activity and thus may protect human beings from various narirutin (SICARI et al., 2015). Diets rich in flavonoids reduce post- diseases. ischemic miocardiac damage in rats (FACINO et al., 1999), coronaric The following physical and nutritional properties of three bergamot damage and the incidence of heart attacks in elderly man (HERTOG cultivars (Castagnaro, Fantastico and Femminello) were determined et al., 1993). and compared: pH, titratable acidity, vitamin C, total flavonoids, The major causes of cell damage following oxidative stress are total polyphenols, antocianyn, bioactive molecules and antioxidant reactive oxygen species (ROS). Reactive oxygen species (ROS) are capacity (ABTS and DPPH assay). The comparison data, were found produced as a normal product of plant cellular metabolism. Various to be statistically different. environmental stresses lead to excessive production of ROS causing In all juice samples analyzed the highest antioxidant capacity was progressive oxidative damage and ultimately cell death (SASTRE found in Castagnaro juice (64.21% I of DPPH and 1.97% I of ABTS) et al., 2000). compared to Fantastico (44.48% I of DPPH and 1.83% I of ABTS) After ingestion as food the flavanone glycosides are metabolized and Femminello (33.39% I of DPPH and 1.13% I of ABTS). -

Glycosides in Lemon Fruit
Food Sci. Technol. Int. Tokyo, 4 (1), 48-53, 1998 Characteristics of Antioxidative Flavonoid Glycosides in Lemon Fruit Yoshiaki MIYAKE,1 Kanefumi YAMAMOT0,1 Yasujiro MORIMITSU2 and Toshihiko OSAWA2 * Central Research Laboratory of Pokka Corporation, Ltd., 45-2 Kumanosyo, Shikatsu-cho, Nishikasugai-gun, Aichi 481, Japan 2Department of Applied Biological Sciences, Nagoya University, Nagoya 46401, Japan Received June 12, 1997; Accepted September 27, 1997 We investigated the antioxidative flavonoid glycosides in the peel extract of lemon fruit (Citrus limon). Six flavanon glycosides: eriocitrin, neoeriocitrin, narirutin, naringin, hesperidin, and neohesperidin, and three flavone glycosides: diosmin, 6~-di- C-p-glucosyldiosmin (DGD), and 6- C-p-glucosyldiosmin (GD) were identified by high- performance liquid chromatography (HPLC) analysis. Their antioxidative activity was examined using a linoleic acid autoxidation system. The antioxidative activity of eriocitrin, neoeriocitrin and DGD was stronger than that of the others. Flavonoid glycosides were present primarily in the peel of lemon fruit. There was only a small difference in the content of the flavonoid glycosides of the lemon fruit juice from various sources and varieties. Lemon fruit contained abundant amounts of eriocitrin and hesperidin and also contained narirutin, diosmin, and DGD, but GD, neoeriocitrin, naringin, and neohesperidin were present only in trace amounts. The content of DGD, GD, and eriocitrin was especially abundant in lemons and limes; however, they were scarcely found in other citrus fruits. The content of flavonoid compounds in lemon juice obtained by an in-line extractor at a juice factory was more abundant than that obtained by hand-squeezing. These compounds were found to be stable even under heat treatment conditions (121'C, 15 min) in acidic solution. -

Important Flavonoids and Their Role As a Therapeutic Agent
molecules Review Important Flavonoids and Their Role as a Therapeutic Agent Asad Ullah 1 , Sidra Munir 1 , Syed Lal Badshah 1,* , Noreen Khan 1, Lubna Ghani 2, Benjamin Gabriel Poulson 3 , Abdul-Hamid Emwas 4 and Mariusz Jaremko 3,* 1 Department of Chemistry, Islamia College University Peshawar, Peshawar 25120, Pakistan; [email protected] (A.U.); [email protected] (S.M.); [email protected] (N.K.) 2 Department of Chemistry, The University of Azad Jammu and Kashmir, Muzaffarabad, Azad Kashmir 13230, Pakistan; [email protected] 3 Division of Biological and Environmental Sciences and Engineering (BESE), King Abdullah University of Science and Technology (KAUST), Thuwal 23955-6900, Saudi Arabia; [email protected] 4 Core Labs, King Abdullah University of Science and Technology (KAUST), Thuwal 23955-6900, Saudi Arabia; [email protected] * Correspondence: [email protected] (S.L.B.); [email protected] (M.J.) Received: 20 September 2020; Accepted: 1 November 2020; Published: 11 November 2020 Abstract: Flavonoids are phytochemical compounds present in many plants, fruits, vegetables, and leaves, with potential applications in medicinal chemistry. Flavonoids possess a number of medicinal benefits, including anticancer, antioxidant, anti-inflammatory, and antiviral properties. They also have neuroprotective and cardio-protective effects. These biological activities depend upon the type of flavonoid, its (possible) mode of action, and its bioavailability. These cost-effective medicinal components have significant biological activities, and their effectiveness has been proved for a variety of diseases. The most recent work is focused on their isolation, synthesis of their analogs, and their effects on human health using a variety of techniques and animal models. -

Antioxidant and Anti-Inflammatory Activity of Citrus Flavanones Mix
antioxidants Article Antioxidant and Anti-Inflammatory Activity of Citrus Flavanones Mix and Its Stability after In Vitro Simulated Digestion Marcella Denaro †, Antonella Smeriglio *,† and Domenico Trombetta Department of Chemical, Biological, Pharmaceutical and Environmental Sciences, University of Messina, Viale Palatucci, 98168 Messina, Italy; [email protected] (M.D.); [email protected] (D.T.) * Correspondence: [email protected]; Tel.: +39-090-676-4039 † Both authors contributed equally. Abstract: Recently, several studies have highlighted the role of Citrus flavanones in counteracting oxidative stress and inflammatory response in bowel diseases. The aim of study was to identify the most promising Citrus flavanones by a preliminary antioxidant and anti-inflammatory screening by in vitro cell-free assays, and then to mix the most powerful ones in equimolar ratio in order to investigate a potential synergistic activity. The obtained flavanones mix (FM) was then subjected to in vitro simulated digestion to evaluate the availability of the parent compounds at the intestinal level. Finally, the anti-inflammatory activity was investigated on a Caco-2 cell-based model stimulated with interleukin (IL)-1β. FM showed stronger antioxidant and anti-inflammatory activity with respect to the single flavanones, demonstrating the occurrence of synergistic activity. The LC-DAD-ESI- MS/MS analysis of gastric and duodenal digested FM (DFM) showed that all compounds remained unchanged at the end of digestion. As proof, a superimposable behavior was observed between FM and DFM in the anti-inflammatory assay carried out on Caco-2 cells. Indeed, it was observed that both FM and DFM decreased the IL-6, IL-8, and nitric oxide (NO) release similarly to the reference Citation: Denaro, M.; Smeriglio, A.; anti-inflammatory drug dexamethasone. -
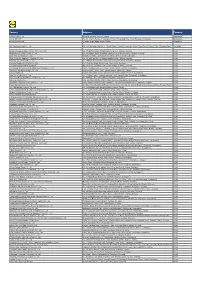
Factory Address Country
Factory Address Country Durable Plastic Ltd. Mulgaon, Kaligonj, Gazipur, Dhaka Bangladesh Lhotse (BD) Ltd. Plot No. 60&61, Sector -3, Karnaphuli Export Processing Zone, North Potenga, Chittagong Bangladesh Bengal Plastics Ltd. Yearpur, Zirabo Bazar, Savar, Dhaka Bangladesh ASF Sporting Goods Co., Ltd. Km 38.5, National Road No. 3, Thlork Village, Chonrok Commune, Korng Pisey District, Konrrg Pisey, Kampong Speu Cambodia Ningbo Zhongyuan Alljoy Fishing Tackle Co., Ltd. No. 416 Binhai Road, Hangzhou Bay New Zone, Ningbo, Zhejiang China Ningbo Energy Power Tools Co., Ltd. No. 50 Dongbei Road, Dongqiao Industrial Zone, Haishu District, Ningbo, Zhejiang China Junhe Pumps Holding Co., Ltd. Wanzhong Villiage, Jishigang Town, Haishu District, Ningbo, Zhejiang China Skybest Electric Appliance (Suzhou) Co., Ltd. No. 18 Hua Hong Street, Suzhou Industrial Park, Suzhou, Jiangsu China Zhejiang Safun Industrial Co., Ltd. No. 7 Mingyuannan Road, Economic Development Zone, Yongkang, Zhejiang China Zhejiang Dingxin Arts&Crafts Co., Ltd. No. 21 Linxian Road, Baishuiyang Town, Linhai, Zhejiang China Zhejiang Natural Outdoor Goods Inc. Xiacao Village, Pingqiao Town, Tiantai County, Taizhou, Zhejiang China Guangdong Xinbao Electrical Appliances Holdings Co., Ltd. South Zhenghe Road, Leliu Town, Shunde District, Foshan, Guangdong China Yangzhou Juli Sports Articles Co., Ltd. Fudong Village, Xiaoji Town, Jiangdu District, Yangzhou, Jiangsu China Eyarn Lighting Ltd. Yaying Gang, Shixi Village, Shishan Town, Nanhai District, Foshan, Guangdong China Lipan Gift & Lighting Co., Ltd. No. 2 Guliao Road 3, Science Industrial Zone, Tangxia Town, Dongguan, Guangdong China Zhan Jiang Kang Nian Rubber Product Co., Ltd. No. 85 Middle Shen Chuan Road, Zhanjiang, Guangdong China Ansen Electronics Co. Ning Tau Administrative District, Qiao Tau Zhen, Dongguan, Guangdong China Changshu Tongrun Auto Accessory Co., Ltd. -

W O 2014/006097 a L 9 January 2014 (09.01.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date W O 2014/006097 A l 9 January 2014 (09.01.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A01N 43/16 (2006.01) A01N 65/36 (2009.01) kind of national protection available): AE, AG, AL, AM, A61K 8/49 (2006.01) A01P 1/00 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A61K 31/352 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KN, KP, KR, PCT/EP20 13/064042 KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, (22) International Filing Date: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, 3 July 20 13 (03.07.2013) OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, (25) Filing Language: English TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 12174837.0 3 July 2012 (03.07.2012) EP GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (71) Applicant: CEBEC GROUP LTD. -

Effect of Post-Harvest LED and UV Light Irradiation on the Accumulation of Flavonoids and Limonoids in the Segments of Newhall Navel Oranges
molecules Article Effect of Post-Harvest LED and UV Light Irradiation on the Accumulation of Flavonoids and Limonoids in the Segments of Newhall Navel Oranges (Citrus sinensis Osbeck) Shengyu Liu 1, Linping Hu 1, Dong Jiang 2 and Wanpeng Xi 1,3,* 1 College of Horticulture and Landscape Architecture, Southwest University, Chongqing 400716, China; [email protected] (S.L.); [email protected] (L.H.) 2 Citrus Research Institute, Chinese Academy of Agricultural Sciences, Chongqing 400712, China; [email protected] 3 Key Laboratory of Horticulture Science for Southern Mountainous Regions, Ministry of Education, Chongqing 400715, China * Correspondence: [email protected]; Tel.: +86-23-68250483; Fax: +86-23-68251274 Received: 20 March 2019; Accepted: 4 May 2019; Published: 6 May 2019 Abstract: To investigate the effect of post-harvest light irradiation on the accumulation of flavonoids and limonoids, harvested Newhall navel oranges were continuously exposed to light-emitting diode (LED) and ultraviolet (UV) light irradiation for 6 days, and the composition and content of flavonoids and limonoids in the segments were determined using UPLC-qTOF-MS at 0, 6, and 15 days after harvest. In total, six polymethoxylated flavonoids (PMFs), five flavone-O/C-glycosides, seven flavanone-O-glycosides, and three limonoids were identified in the segments. The accumulation of these components was altered by light irradiation. Red and blue light resulted in higher levels of PMFs during exposure periods. The accumulation of PMFs was also significantly induced after white light, UVB and UVC irradiation were removed. Red and UVC irradiation induced the accumulation of flavone and flavanone glycosides throughout the entire experimental period. -

Modes of Action of Herbal Medicines and Plant Secondary Metabolites
Medicines 2015, 2, 251-286; doi:10.3390/medicines2030251 OPEN ACCESS medicines ISSN 2305-6320 www.mdpi.com/journal/medicines Review Modes of Action of Herbal Medicines and Plant Secondary Metabolites Michael Wink Institute of Pharmacy and Molecular Biotechnology, Heidelberg University, INF 364, Heidelberg D-69120, Germany; E-Mail: [email protected]; Tel.: +49-6221-544-881; Fax: +49-6221-544-884 Academic Editor: Shufeng Zhou Received: 13 August 2015 / Accepted: 31 August 2015 / Published: 8 September 2015 Abstract: Plants produce a wide diversity of secondary metabolites (SM) which serve them as defense compounds against herbivores, and other plants and microbes, but also as signal compounds. In general, SM exhibit a wide array of biological and pharmacological properties. Because of this, some plants or products isolated from them have been and are still used to treat infections, health disorders or diseases. This review provides evidence that many SM have a broad spectrum of bioactivities. They often interact with the main targets in cells, such as proteins, biomembranes or nucleic acids. Whereas some SM appear to have been optimized on a few molecular targets, such as alkaloids on receptors of neurotransmitters, others (such as phenolics and terpenoids) are less specific and attack a multitude of proteins by building hydrogen, hydrophobic and ionic bonds, thus modulating their 3D structures and in consequence their bioactivities. The main modes of action are described for the major groups of common plant secondary metabolites. The multitarget activities of many SM can explain the medical application of complex extracts from medicinal plants for more health disorders which involve several targets. -

Supplementary Materials for the Article: a Running Start Or a Clean Slate
Supplementary Materials for the article: A running start or a clean slate? How a history of cooperation affects the ability of cities to cooperate on environmental governance Rui Mu1, * and Wouter Spekkink2 1 Dalian University of Technology, Faculty of Humanities and Social Sciences; [email protected] 2 The University of Manchester, Sustainable Consumption Institute; [email protected] * Correspondence: [email protected]; Tel.: +86-139-0411-9150 Appendix 1: Environmental Governance Actions in Beijing-Tianjin-Hebei Urban Agglomeration Event time Preorder Action Event Event name and description Actors involved (year-month-day) event no. type no. Part A: Joint actions at the agglomeration level MOEP NDRC Action plan for Beijing, Tianjin, Hebei and the surrounding areas to implement MOIIT 2013 9 17 FJA R1 air pollution control MOF MOHURD NEA BG TG HP MOEP NDRC Collaboration mechanism of air pollution control in Beijing, Tianjin, Hebei and 2013 10 23 R1 FJA MOIIT R2 the surrounding areas MOF MOHURD CMA NEA MOT BG Coordination office of air pollution control in Beijing, Tianjin, Hebei and the 2013 10 23 R2 FJA TG R3 surrounding areas HP 1 MOEP NDRC MOIIT MOF MOHURD CMA NEA MOT BG Clean Production Improvement Plan for Key Industrial Enterprises in Beijing, TG 2014 1 9 R1 FJA R4 Tianjin, Hebei and the Surrounding Areas HP MOIIT MOEP BTHAPCLG Regional air pollution joint prevention and control forum (the first meeting) 2014 3 3 R2, R3 IJA BEPA R5 was held by the Coordination Office. TEPA HEPA Coordination working unit was established for comprehensive atmospheric BTHAPCLG 2014 3 25 R3 FJA R6 pollution control. -

Space As Sociocultural Construct: Reinterpreting the Traditional Residences in Jinqu Basin, China from the Perspective of Space Syntax
sustainability Article Space as Sociocultural Construct: Reinterpreting the Traditional Residences in Jinqu Basin, China from the Perspective of Space Syntax Yu Chen 1,2,†, Keyou Xu 1,†, Pei Liu 1, Ruyu Jiang 1, Jingyi Qiu 1, Kangle Ding 3,* and Hiroatsu Fukuda 2,* 1 College of Landscape and Architecture, Zhejiang A&F University, Hangzhou 311300, China; [email protected] (Y.C.); [email protected] (K.X.); [email protected] (P.L.); [email protected] (R.J.); [email protected] (J.Q.) 2 Faculty of Environmental Engineering, The University of Kitakyushu, Kitakyushu 808-0135, Japan 3 School of Civil Engineering and Architecture, Zhejiang University of Science and Technology, Hangzhou 310023, China * Correspondence: [email protected] (K.D.); [email protected] (H.F.) † These authors contributed equally to the study. Abstract: The traditional residence with protogenetic spatial arrangement is regarded as a critical carrier of social logic of space, which makes it an ideal object for studying the relationship between the spatial form and social context. To this end, a comparative analysis is conducted using Depthmap Software. This study is based on space syntax theory between two groups of proxies of sharp differences in spatial organization in one geomorphic unit where the natural factors show little variations, while the human factors present a bifurcating distribution. Furthermore, the study clarifies the differences among genotypes of the domestic space system. Finally, combined with Citation: Chen, Y.; Xu, K.; Liu, P.; historical material, it proves the dual division of regional sociocultural factors as decisive forces Jiang, R.; Qiu, J.; Ding, K.; Fukuda, H.