Cancers of the Endocrine Organs – Endocrine Neoplasms Preferred Model of Care and Criteria for Reference Centres
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Adrenal Cancer Causes, Risk Factors, and Prevention Adrenal
cancer.org | 1.800.227.2345 Adrenal Cancer Causes, Risk Factors, and Prevention Risk Factors A risk factor is anything that affects your chance of getting a disease such as cancer. Learn more about the risk factors for adrenal cancer. ● Adrenal Cancer Risk Factors ● What Causes Adrenal Cancer? Prevention Since there are no known preventable risk factors for this cancer, it is not possible to prevent this disease. Adrenal Cancer Risk Factors A risk factor is anything that changes your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking, can be changed. Others, like a person’s age or family history, can’t be changed. Scientists have found few risk factors that make a person more likely to develop adrenal cancer. Even if a patient does have one or more risk factors for adrenal cancer, it is impossible to know for sure how much that risk factor contributed to causing the cancer. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 But having a risk factor, or even several, does not mean that you will get the disease. Many people with risk factors never develop adrenal cancer, while others with this disease may have few or no known risk factors. Genetic syndromes The majority of adrenal cortex cancers are not inherited (sporadic), but some (up to 15%) are caused by a genetic defect. This is more common in adrenal cancers in children. Li-Fraumeni syndrome The Li-Fraumeni syndrome is a rare condition that is most often caused by a defect in the TP53 gene. -

Endocrine Pathology (537-577)
LABORATORY INVESTIGATION THE BASIC AND TRANSLATIONAL PATHOLOGY RESEARCH JOURNAL LI VOLUME 99 | SUPPLEMENT 1 | MARCH 2019 2019 ABSTRACTS ENDOCRINE PATHOLOGY (537-577) MARCH 16-21, 2019 PLATF OR M & 2 01 9 ABSTRACTS P OSTER PRESENTATI ONS EDUCATI ON C O M MITTEE Jason L. Hornick , C h air Ja mes R. Cook R h o n d a K. Y a nti s s, Chair, Abstract Revie w Board S ar a h M. Dr y and Assign ment Co m mittee Willi a m C. F a q ui n Laura W. La mps , Chair, C ME Subco m mittee C ar ol F. F ar v er St e v e n D. Billi n g s , Interactive Microscopy Subco m mittee Y uri F e d ori w Shree G. Shar ma , Infor matics Subco m mittee Meera R. Ha meed R aj a R. S e et h al a , Short Course Coordinator Mi c h ell e S. Hir s c h Il a n W ei nr e b , Subco m mittee for Unique Live Course Offerings Laksh mi Priya Kunju D a vi d B. K a mi n s k y ( Ex- Of ici o) A n n a M ari e M ulli g a n Aleodor ( Doru) Andea Ri s h P ai Zubair Baloch Vi nita Parkas h Olca Bast urk A nil P ar w a ni Gregory R. Bean , Pat h ol o gist-i n- Trai ni n g D e e p a P atil D a ni el J. -

Nonfunctional Metastatic Parathyroid Carcinoma in the Setting of Multiple Endocrine Neoplasia Type 2A Syndrome
Hindawi Publishing Corporation Surgery Research and Practice Volume 2014, Article ID 731481, 4 pages http://dx.doi.org/10.1155/2014/731481 Case Report Nonfunctional Metastatic Parathyroid Carcinoma in the Setting of Multiple Endocrine Neoplasia Type 2A Syndrome María Posada-González,1 Joaquín Gómez-Ramírez,2 Manuel Luque-Ramírez,3 Mercedes Guijarro,4 Elena Martín-Pérez,1 Ana Rodríguez-Sánchez,1 Iñigo García-Sanz,1 and Eduardo Larrañaga1 1 Department of General and Gastrointestinal Surgery, La Princesa University Hospital, 62 Diego de Leon Street, 28006 Madrid, Spain 2 Department of General and Gastrointestinal Surgery, Fundacion´ Jimenez´ D´ıaz Hospital, 2 Reyes Catolicos Avenue, 28040 Madrid, Spain 3 Department of Endocrinology and Clinical Nutrition, Ramon´ y Cajal University Hospital, Colmenar Viejo Road 9.100 Km, 28034 Madrid, Spain 4 Department of Pathology, La Princesa University Hospital, 62 Diego de Leon Street, 28006 Madrid, Spain Correspondence should be addressed to Mar´ıa Posada-Gonzalez;´ [email protected] Received 28 August 2013; Accepted 26 September 2013; Published 20 February 2014 AcademicEditors:C.Foroulis,G.Lal,andF.Turegano´ Copyright © 2014 Mar´ıa Posada-Gonzalez´ et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Parathyroid carcinoma is a very rare malignancy. It has been associated with hyperparathyroidism-jaw tumour syndrome, familial isolated primary hyperparathyroidism, and multiple endocrine neoplasia type 1 (MEN-1) and 2A (MEN-2A) syndromes. We report a 54-year-old man with a MEN-2A which presents with a nonfunctional metastatic parathyroid carcinoma and a pheochromocytoma in the absence of medullary thyroid carcinoma. -

MEN1 Gene Mutation with Parathyroid Carcinoma: First Report of a Familial Case
6 8 L Cinque, A Sparaneo et al. MEN1familial familialcase and caseparathyroid andcarcinoma 886–8916:8 8866–891:886 Research parathyroid carcinoma Open Access MEN1 gene mutation with parathyroid carcinoma: first report of a familial case Luigia Cinque1,*, Angelo Sparaneo2,*, Antonio S Salcuni3, Danilo de Martino4, Claudia Battista3, Francesco Logoluso5, Orazio Palumbo1, Roberto Cocchi6, Evaristo Maiello7, Paolo Graziano8, Geoffrey N Hendy9, David E C Cole10, Alfredo Scillitani3 and Vito Guarnieri1 1Medical Genetics, IRCCS Casa Sollievo della Sofferenza Hospital, San Giovanni Rotondo (FG), Italy 2Laboratory of Oncology, IRCCS Casa Sollievo della Sofferenza Hospital, San Giovanni Rotondo (FG), Italy 3Endocrinology, IRCCS Casa Sollievo della Sofferenza Hospital, San Giovanni Rotondo (FG), Italy 4Thoracic Surgery, IRCCS Casa Sollievo della Sofferenza Hospital, San Giovanni Rotondo (FG), Italy 5Department of Emergency and Organ Transplantation, Unit of Endocrinology, University Medical School of Bari ‘Aldo Moro’, Bari, Italy 6Maxillofacial Surgery, IRCCS Casa Sollievo della Sofferenza Hospital, San Giovanni Rotondo (FG), Italy 7Oncoematology, IRCCS Casa Sollievo della Sofferenza Hospital, San Giovanni Rotondo (FG), Italy 8Pathology, IRCCS Casa Sollievo della Sofferenza Hospital, San Giovanni Rotondo (FG), Italy 9Departments of Medicine, Physiology and Human Genetics, McGill University and Metabolic Disorders and Correspondence Complications, McGill University Health Centre Research Institute, Montreal, Quebec, Canada should be addressed 10Departments -

Synchronous Primary Hyperparathyroidism and Papillary Thyroid Carcinoma in a 50-Year-Old Female, Who Initially Presented with Uncontrolled Hypertension
Open Access http://www.jparathyroid.com Journal of Journal of Parathyroid Disease 2014,2(2),69–70 Epidemiology and Prevention Synchronous primary hyperparathyroidism and papillary thyroid carcinoma in a 50-year-old female, who initially presented with uncontrolled hypertension Seyed Seifollah Beladi Mousavi1, Hamid Nasri2*, Saeed Behradmanesh3 hough, the association between parathyroid and Implication for health policy/practice/research/ thyroid diseases is not uncommon, however medical education concurrent presence of parathyroid adenoma An association between parathyroid adenoma Tand thyroid cancer is rare (1,2). The association between and thyroid cancer is rare. Awareness of this concurrent thyroid and parathyroid disease was firstly situation will enable clinicians to consider for explained by Kissin et al. in 1947 (2). Awareness of possible thyroid pathology in patients with primary this situation will enable clinicians to consider for hyperparathyroidism. Both of these endocrine diseases possible thyroid pathology in patients with primary could then be managed with a single surgery involving hyperparathyroidism. While thyroid follicular cells and concomitant resection of the thyroid and involved parathyroid cells are embryologically different. It is evident parathyroid glands. that presence of parathyroid adenoma leading to primary hyperparathyroidism and coexistent of thyroid papillary cancer is rare. Both of these endocrine diseases could then coincidence of papillary thyroid carcinoma. After surgery, be managed with a single surgery involving concomitant serum parathormone and calcium returned to their normal resection of the thyroid and involved parathyroid glands. values and patient was referred to an endocrinologist for A 50-year-old female, referred to the nephrology clinic for continuing the treatment of papillary carcinoma. -

Parathyroid Carcinoma Presenting As an Acute Pancreatitis
International Journal of Radiology & Radiation Therapy Case Report Open Access Parathyroid carcinoma presenting as an acute pancreatitis Abstract Volume 3 Issue 3 - 2017 Parathyroid carcinoma is the cause of only 1% of hyperparathyroidism cases. The Enrique Cadena,1,2,3 Alfredo Romero-Rojas1,3 incidence of acute pancreatitis in patients with hyperparathyroidism was reported to 1Department of Head and Neck Surgery and Pathology, be only 1.5%. The occurrence of pancreatitis in patients with parathyroid carcinoma National Cancer Institute, Colombia is unusual, ranging from 0% to 15%. Here, we report a very rare case of parathyroid 2Department of Surgery, National University of Colombia, carcinoma presenting as an acute pancreatitis in a 45years old woman, who was Colombia suspected for hypercalcemia and higher levels of intact parathyroid hormone. The 3Department of Head and Neck Surgery and Pathology, Marly parathyroid carcinoma was verified with ultrasound, CT Scan, and single-photon Clinic, Colombia emission computed tomography. The pathological anatomy report showed a minimally invasive parathyroid carcinoma. Following surgery, the patient was free after almost Correspondence: Enrique Cadena, Department of Head and a 4years follow up. Neck Surgery and Pathology, National Cancer Institute, Bogotá, 1st Street # 9-85, Colombia, Tel 5713341111, 5713341478, Keywords: acute necrotizing pancreatitis, hypercalcemia, primary Email [email protected] hyperparathyroidism, parathyroid carcinoma Received: May 29, 2017 | Published: June 27, 2017 Abbreviations: HPT, hyperparathyroidism; PHPT, primary (2.5mg/dl) levels. Kidney and liver function tests, albumin and hyperparathyroidism; SPECT, single-photon emission computed to- triglyceride levels were all within normal limits. The patient was mography; CT, computed tomography; iPTH, intact parathyroid hor- treated initially with intravenous fluids and H2 blockers, and no oral mone. -

Downloaded from Bioscientifica.Com at 09/30/2021 02:21:58AM Via Free Access
27 8 Endocrine-Related C R C Pieterman, Future directives in 27:8 T9–T25 Cancer S M Sadowski et al. MEN1-related PanNETs THEMATIC REVIEW HEREDITARY ENDOCRINE TUMOURS: CURRENT STATE-OF-THE-ART AND RESEARCH OPPORTUNITIES MEN1-related pancreatic NETs: identification of unmet clinical needs and future directives C R C Pieterman1,2,*, S M Sadowski3,*, J E Maxwell4, M H G Katz4, K E Lines5, C M Heaphy6,†, A Tirosh7, J E Blau8, N D Perrier1, M A Lewis9,10, J P Metzcar11,12, D M Halperin13, R V Thakker5 and G D Valk2 1Section of Surgical Endocrinology, Department of Surgical Oncology, University of Texas MD Anderson Cancer Center, Houston, Texas, USA 2Department of Endocrine Oncology, University Medical Center Utrecht, Utrecht, The Netherlands 3Endocrine Surgery, Surgical Oncology Program, National Cancer Institute, National Institutes of Health, Bethesda, Maryland, USA 4Department of Surgical Oncology, University of Texas MD Anderson Cancer Center, Houston, Texas, USA 5Academic Endocrine Unit, Radcliffe Department of Medicine, OCDEM, University of Oxford, Oxford, UK 6Departments of Pathology and Oncology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA 7Neuroendocrine Tumors Service, Division of Endocrinology, Metabolism and Diabetes, The Chaim Sheba Medical Center, and Sackler Faculty of Medicine, Tel-Aviv University, Tel-Aviv, Israel 8Metabolic Diseases Branch, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, Maryland, USA 9Gastrointestinal Oncology, Intermountain -
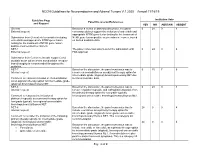
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19
NCCN Guidelines for Neuroendocrine and Adrenal Tumors V.1.2020 – Annual 11/18/19 Guideline Page Institution Vote Panel Discussion/References and Request YES NO ABSTAIN ABSENT General Based on a review of data and discussion, the panel 0 24 0 4 External request: consensus did not support the inclusion of entrectinib and appropriate NTRK gene fusion testing for the treatment of Submission from Genentech to consider including NTRK gene fusion-positive neuroendocrine cancer, based entrectinib and appropriate NTRK gene fusion on limited available data. testing for the treatment of NTRK gene fusion- positive neuroendocrine cancers. NET-1 The panel consensus was to defer the submission until 0 24 0 4 External request: FDA approval. Submission from Curium to include copper Cu 64 dotatate as an option where somatostatin receptor- based imaging is recommended throughout the guideline. NET-7 Based on the discussion, the panel consensus was to 0 15 7 6 Internal request: remove chemoradiation as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET due Comment to reassess inclusion of chemoradiation to limited available data. as an adjuvant therapy option for intermediate grade (atypical) bronchopulmonary NET. NET-8 Based on the discussion, the panel consensus was to 0 24 0 4 Internal request: remove cisplatin/etoposide and carboplatin/etoposide from the primary therapy option for low grade (typical), Comment to reassess the inclusion of locoregional unresectable bronchopulmonary/thymus NET. platinum/etoposide as a primary therapy option for low grade (typical), locoregional unresectable bronchopulmonary/thymus NET. NET-8 Based on the discussion, the panel consensus was to 24 0 0 4 Internal request: include everolimus as a primary therapy option for intermediate grade (atypical), locoregional unresectable Comment to consider the inclusion of the following bronchopulmonary/thymus NET. -

Neoplastic Metastases to the Endocrine Glands
27 1 Endocrine-Related A Angelousi et al. Metastases to endocrine 27:1 R1–R20 Cancer organs REVIEW Neoplastic metastases to the endocrine glands Anna Angelousi1, Krystallenia I Alexandraki2, George Kyriakopoulos3, Marina Tsoli2, Dimitrios Thomas2, Gregory Kaltsas2 and Ashley Grossman4,5,6 1Endocrine Unit, 1st Department of Internal Medicine, Laiko Hospital, National and Kapodistrian University of Athens, Athens, Greece 2Endocrine Unit, 1st Department of Propaedeutic Medicine, Laiko University Hospital, Medical School, National and Kapodistrian University of Athens, Athens, Greece 3Department of Pathology, General Hospital ‘Evangelismos’, Αthens, Greece 4Department of Endocrinology, OCDEM, University of Oxford, Oxford, UK 5Neuroendocrine Tumour Unit, Royal Free Hospital, London, UK 6Centre for Endocrinology, Barts and the London School of Medicine, Queen Mary University of London, London, UK Correspondence should be addressed to A Angelousi: [email protected] Abstract Endocrine organs are metastatic targets for several primary cancers, either through Key Words direct extension from nearby tumour cells or dissemination via the venous, arterial and f glands lymphatic routes. Although any endocrine tissue can be affected, most clinically relevant f cancer metastases involve the pituitary and adrenal glands with the commonest manifestations f metastases being diabetes insipidus and adrenal insufficiency respectively. The most common f pituitary primary tumours metastasing to the adrenals include melanomas, breast and lung f adrenal carcinomas, which may lead to adrenal insufficiency in the presence of bilateral adrenal f thyroid involvement. Breast and lung cancers are the most common primaries metastasing to f ovaries the pituitary, leading to pituitary dysfunction in approximately 30% of cases. The thyroid gland can be affected by renal, colorectal, lung and breast carcinomas, and melanomas, but has rarely been associated with thyroid dysfunction. -
View Its Management Considering the Recent Relevant Literature
Ferraro et al. BMC Endocrine Disorders 2019, 19(Suppl 1):46 https://doi.org/10.1186/s12902-019-0368-1 RESEARCH Open Access Current concepts in parathyroid carcinoma: a single Centre experience Valentina Ferraro1†, Lucia Ilaria Sgaramella1†, Giovanna Di Meo1, Francesco Paolo Prete2, Francesco Logoluso2, Francesco Minerva1, Marica Noviello1, Giuseppina Renzulli3, Angela Gurrado1 and Mario Testini1* Abstract Background: Parathyroid carcinoma is a rare neoplasm that may present sporadically or in the context of a genetic syndrome. Diagnosis and management are challenging due to the lack of clinical and pathological features that may reliably distinguish malignant from benign disease. Methods: From January 2013 to December 2017, from 358 consecutive patients affected by parathyroid diseases, 3 patients with parathyroid carcinoma were treated at our academic Department of General Surgery. We present our experience as illustrative of the different features of clinical presentation of parathyroid carcinoma and review its management considering the recent relevant literature. Results: Case 1: A 62-year-old man was hospitalized for left-sided palpable neck mass, hypercalcemia and elevated PTH. US-guided FNA was suspect for parathyroid carcinoma. A large cystic mass was excised in bloc with total thyroidectomy and central neck dissection. Genetic studies framed a pathologically confirmed parathyroid carcinoma within MEN1 syndrome. Case 2: A 48-year-old woman with hypothyroidism had total thyroidectomy performed for a suspect for right follicular thyroid lesion. Pathology revealed parathyroid carcinoma. Case 3: A47 year-old man was admitted for hypercalcaemic crisis and renal failure in the context of PHPT. A lesion suggestive on US and MIBI scan for parathyroid adenoma in the right lower position was removed by mini-invasive approach. -
NCCN Neuroendocrine Tumors Guidelines Are Divided Into 6 Endocrine Systems, Which Produce and Secrete Regulatory Hormones
NCCN Clinical Practice Guidelines in Oncology™ Neuroendocrine Tumors V.1.2007 Continue www.nccn.org Guidelines Index ® Practice Guidelines Neuroendocrine TOC NCCN in Oncology – v.1.2007 Neuroendocrine Tumors MS, References NCCN Neuroendocrine Tumors Panel Members * Orlo H. Clark, MD/Chair ¶ John F. Gibbs, MD ¶ Thomas W. Ratliff, MD † UCSF Comprehensive Cancer Center Roswell Park Cancer Institute St. Jude Children's Research Hospital/University of Tennessee Jaffer Ajani, MD †¤ Martin J. Heslin, MD ¶ Cancer Institute The University of Texas M. D. University of Alabama at Anderson Cancer Center Birmingham Comprehensive Leonard Saltz, MD † Cancer Center Memorial Sloan-Kettering Cancer Al B. Benson, III, MD † Center Robert H. Lurie Comprehensive Fouad Kandeel, MD Cancer Center of Northwestern City of Hope Cancer Center David E. Schteingart, MD ð University University of Michigan Anne Kessinger, MD † Comprehensive Cancer Center David Byrd, MD ¶ UNMC Eppley Cancer Center at The Fred Hutchinson Cancer Research Nebraska Medical Center Manisha H. Shah, MD † Center/Seattle Cancer Care Alliance Arthur G. James Cancer Hospital & Matthew H. Kulke, MD † Richard J. Solove Research Gerard M. Doherty, MD ¶ Dana-Farber/Partners CancerCare Institute at The Ohio State University of Michigan Comprehensive University Cancer Center Larry Kvols, MD † H. Lee Moffitt Cancer Center & Stephen Shibata, MD † Paul F. Engstrom, MD † Research Institute at the University City of Hope Cancer Center Fox Chase Cancer Center of South Florida David S. Ettinger, MD † John A. Olson, Jr., MD, PhD ¶ The Sidney Kimmel Comprehensive Duke Comprehensive Cancer Cancer Center at Johns Hopkins Center * Writing Committee Member ¶ Surgery/Surgical oncology † Medical oncology ¤ Gastroenterology ð Endocrinology Continue Version 1.2007, 03/14/07 © 2007 National Comprehensive Cancer Network, Inc. -

A Case of Postpartum Hypopituitarism Accompanied by Cushing's
Endocrine Journal 2005, 52 (2), 219–222 A Case of Postpartum Hypopituitarism Accompanied by Cushing’s Syndrome as a Result of an Adrenocortical Carcinoma MEHMET SENCAN AND HATICE SEBILA DOKMETAS* Department of Hematology, Faculty of Medicine, Cumhuriyet University, 58140 Sivas, Turkey *Department of Endocrinology, Faculty of Medicine, Cumhuriyet University, 58140 Sivas, Turkey Abstract. Sheehan’s syndrome frequently causes hypopituitarism either immediately or after a delay of several years, depending on the degrees of postpartum ischemic pituitary necrosis. A 55 year-old woman whose last child was born 27 yr ago with massive hemorrhage was diagnosed as postpartum hypopituitarism. She had deficiency of growth hormone, prolactin, gonadotropins and thyrotropin. However, she interestingly had apparent hypercortisolism without suppression response to the dexamethasone tests. We found an adrenal mass with distant metastases to the liver and lung while investigating the origin of the hypercortisolism. Hyperandrogenism and very high levels of 17 hydroxyprogesterone were present. Accordingly, the patient was diagnosed as hypopituitarism due to Sheehan’s syndrome accompanied by Cushing’s syndrome as a result of an adrenocortical carcinoma. Key words: Sheehan’s syndrome, Hypopituitarism, Hypercortisolism, Adrenocortical carcinoma (Endocrine Journal 52: 219–222, 2005) SHEEHAN’S syndrome occurs as a result of ischemic with adrenocortical carcinoma may show different pituitary necrosis due to severe postpartum hemor- endocrine syndromes depending on the secretion of rhage and is characterized by various degrees of tumor; hypercortisolism and hyperandrogenism are hypopituitarism [1, 2]. Sheehan’s syndrome is a rare the most prevalent [4, 5]. postpartum complication of pregnancy with better In this report, a case with hypopituitarism due to obstetric care in developed countries.