Imaging Features Differentiating Vestibular Ganglion From
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Use of Calcium-Binding Proteins to Map Inputs in Vestibular Nuclei of the Gerbil
THE JOURNAL OF COMPARATIVE NEUROLOGY 386:317–327 (1997) Use of Calcium-Binding Proteins to Map Inputs in Vestibular Nuclei of the Gerbil GOLDA ANNE KEVETTER* AND ROBERT B. LEONARD Departments of Otolaryngology, Anatomy and Neurosciences, and Physiology and Biophysics, University of Texas Medical Branch, Galveston, Texas 77555 ABSTRACT We wished to determine whether calbindin and/or calretinin are appropriate markers for vestibular afferents, a population of neurons in the vestibular nuclear complex, or cerebellar Purkinje inputs. To accomplish this goal, immunocytochemical staining was observed in gerbils after lesions of the vestibular nerve central to the ganglion, the cerebellum, or both. Eleven to fourteen days after recovery, the brain was processed for immunocytochemical identification of calretinin and calbindin. After lesion of the vestibular nerve, no calretinin staining was seen in any of the vestibular nuclei except for a population of intrinsic neurons, which showed no obvious change in number or staining pattern. Calbindin staining was reduced in all nuclei except the dorsal part of the lateral vestibular nuclei. The density of staining of each marker, measured in the magnocellular medial vestibular nucleus, was signifi- cantly reduced. After the cerebellar lesion, no differences in calretinin staining were noted. However, calbindin staining was greatly reduced in all nuclei. The density of staining, measured in the caudal medial vestibular nucleus, was significantly lower. After a combined lesion of the cerebellum and vestibular nerve, the distribution and density of calretinin staining resembled that after vestibular nerve section alone, whereas calbindin staining was no longer seen. This study demonstrates that calretinin and calbindin are effective markers for the identification of vestibular afferents. -

Cranial Nerves 1, 5, 7-12
Cranial Nerve I Olfactory Nerve Nerve fiber modality: Special sensory afferent Cranial Nerves 1, 5, 7-12 Function: Olfaction Remarkable features: – Peripheral processes act as sensory receptors (the other special sensory nerves have separate Warren L Felton III, MD receptors) Professor and Associate Chair of Clinical – Primary afferent neurons undergo continuous Activities, Department of Neurology replacement throughout life Associate Professor of Ophthalmology – Primary afferent neurons synapse with secondary neurons in the olfactory bulb without synapsing Chair, Division of Neuro-Ophthalmology first in the thalamus (as do all other sensory VCU School of Medicine neurons) – Pathways to cortical areas are entirely ipsilateral 1 2 Crania Nerve I Cranial Nerve I Clinical Testing Pathology Anosmia, hyposmia: loss of or impaired Frequently overlooked in neurologic olfaction examination – 1% of population, 50% of population >60 years Aromatic stimulus placed under each – Note: patients with bilateral anosmia often report nostril with the other nostril occluded, eg impaired taste (ageusia, hypogeusia), though coffee, cloves, or soap taste is normal when tested Note that noxious stimuli such as Dysosmia: disordered olfaction ammonia are not used due to concomitant – Parosmia: distorted olfaction stimulation of CN V – Olfactory hallucination: presence of perceived odor in the absence of odor Quantitative clinical tests are available: • Aura preceding complex partial seizures of eg, University of Pennsylvania Smell temporal lobe origin -

Cranial Nerve VIII
Cranial Nerve VIII Color Code Important (The Vestibulo-Cochlear Nerve) Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the students should be able to: ✓ List the nuclei related to vestibular and cochlear nerves in the brain stem. ✓ Describe the type and site of each nucleus. ✓ Describe the vestibular pathways and its main connections. ✓ Describe the auditory pathway and its main connections. Due to the difference of arrangement of the lecture between the girls and boys slides we will stick to the girls slides then summarize the pathway according to the boys slides. Ponto-medullary Sulcus (cerebello- pontine angle) Recall: both cranial nerves 8 and 7 emerge from the ventral surface of the brainstem at the ponto- medullary sulcus (cerebello-pontine angle) Brain – Ventral Surface Vestibulo-Cochlear (VIII) 8th Cranial Nerve o Type: Special sensory (SSA) o Conveys impulses from inner ear to nervous system. o Components: • Vestibular part: conveys impulses associated with body posture ,balance and coordination of head & eye movements. • Cochlear part: conveys impulses associated with hearing. o Vestibular & cochlear parts leave the ventral surface* of brain stem through the pontomedullary sulcus ‘at cerebellopontine angle*’ (lateral to facial nerve), run laterally in posterior cranial fossa and enter the internal acoustic meatus along with 7th (facial) nerve. *see the previous slide Auditory Pathway Only on the girls’ slides 04:14 Characteristics: o It is a multisynaptic pathway o There are several locations between medulla and the thalamus where axons may synapse and not all the fibers behave in the same manner. -

M. Dauzvardis, Phd. 7/10/12 NERVES LISTED ACCORDING to FUNCTIONAL COMPONENTS
M. Dauzvardis, PhD. 7/10/12 NERVES LISTED ACCORDING TO FUNCTIONAL COMPONENTS SPECIAL SOMATIC AFFERENT (SSA) II. Optic: Optic stimuli are received by the rods and cones, relayed to second and third order neurons which comprise the optic nerve. (About half the fibers decussate in the optic chiasma). Impulses are along the optic nerve and optic tract to the lateral geniculate bodies of the diecephalon. Relay is then from the lateral geniculate bodies to the calcarine fissure area of the occipital lobes. VIII. Auditory (Acoustic) (Vestibulocochlear) A. Sound stimulates hair cells (receptors) of the Organ of Corti in the cochlea and impulses are carried along bipolar neurons with their cell bodies in the spiral ganglion to the dorsal and ventral cochlear nuclei of the medulla (hearing). B. Motion of the endolymph stimulates receptors in the sacculus and utriculus and the ampullae of the three semicircular canals. These impulses are carried along bipolar neurons whose cell bodies are in the vestibular ganglion and terminate in the medial, lateral, superior and spinal vestibular nuclei of the medulla (equilibrium). GENERAL SOMATIC AFFERENT (GSA) V. Trigeminal Ophthalmic branch: from cornea, conjunctiva, eyelid, forehead and nose. Maxillary branch: from skin of cheek, lower lid, side of nose and upper jaw, upper teeth, mucosa of mouth and maxillary sinuses. Mandibular branch: from skin of ear pinna, ear canal, temporal area, lower jaw and teeth, mucosa of mouth, gums and general sensation from anterior two‐thirds of the tongue. All of the above neurons have their cell bodies in the trigeminal ganglion and terminate in the sensory nuclei of the 5th nerve. -
Auditory & Vestibular Systems Steven Mcloon Department of Neuroscience University of Minnesota
Auditory & Vestibular Systems Steven McLoon Department of Neuroscience University of Minnesota 1 The auditory & vestibular systems have many similarities. • The sensory apparatus for both are in canals embedded in the bone of the inner ear. • Receptor cells (hair cells) for both are mechanosensory cells with fine stereocilia. • Information for both is carried into the brain via the vestibulochoclear nerve (cranial nerve VIII). 2 Auditory System • The auditory system detects and interprets sound. • Sound is the vibration of air molecules similar to ripples in water that propagate from a thrown rock. • The sound waves have an amplitude (loudness) and frequency (pitch). 3 Auditory System • Humans can typically hear 20 – 20,000 hertz (cycles per second). 4 Auditory System • Humans can typically hear 20 – 20,000 hertz (cycles per second). http://en.wikipedia.org/wiki/Audio_frequency 5 Auditory System • As a person ages, he/she loses the ability to hear high and low frequencies. 6 Auditory System External ear: • includes the pinna, external auditory meatus (ear canal) and tympanic membrane (ear drum). • The pinna and canal collect sound and guide it to the tympanic membrane. • The tympanic membrane vibrates in response to sound. 7 Auditory System Middle ear: • It is an air filled chamber. • The eustachian tube (auditory tube) connects the middle ear chamber with the pharynx (throat). • Three tiny bones in the chamber transfer the vibration of the tympanic membrane to the oval window of the inner ear. • Two tiny muscles can dampen the movement of the tympanic membrane and bones to protect against a loud sound. 8 Auditory System Inner ear: • The cochlea is a snail shaped tube incased in bone. -

Early Trigeminal Ganglion Afferents Enter the Cerebellum Before the Purkinje Cells Are Born and Target the Nuclear Transitory Zo
Brain Structure and Function (2019) 224:2421–2436 https://doi.org/10.1007/s00429-019-01916-7 ORIGINAL ARTICLE Early trigeminal ganglion aferents enter the cerebellum before the Purkinje cells are born and target the nuclear transitory zone Hassan Marzban1,3 · Maryam Rahimi‑Balaei1 · Richard Hawkes2 Received: 24 May 2018 / Accepted: 25 June 2019 / Published online: 29 June 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract In the standard model for the development of climbing and mossy fber aferent pathways to the cerebellum, the ingrowing axons target the embryonic Purkinje cell somata (around embryonic ages (E13–E16 in mice). In this report, we describe a novel earlier stage in aferent development. Immunostaining for a neuroflament-associated antigen (NAA) reveals the early axon distributions with remarkable clarity. Using a combination of DiI axon tract tracing, analysis of neurogenin1 null mice, which do not develop trigeminal ganglia, and mouse embryos maintained in vitro, we show that the frst axons to innervate the cerebellar primordium as early as E9 arise from the trigeminal ganglion. Therefore, early trigeminal axons are in situ before the Purkinje cells are born. Double immunostaining for NAA and markers of the diferent domains in the cerebellar primordium reveal that aferents frst target the nuclear transitory zone (E9–E10), and only later (E10–E11) are the axons, either collaterals from the trigeminal ganglion or a new aferent source (e.g., vestibular ganglia), seen in the Purkinje cell plate. The fnding that the earliest axons to the cerebellum derive from the trigeminal ganglion and enter the cerebellar primordium before the Purkinje cells are born, where they seem to target the cerebellar nuclei, reveals a novel stage in the development of the cerebellar aferents. -

VESTIBULAR SYSTEM (Balance/Equilibrium) the Vestibular Stimulus Is Provided by Earth's Gravity, and Head/Body Movement. Locate
VESTIBULAR SYSTEM (Balance/Equilibrium) The vestibular stimulus is provided by Earth’s gravity, and head/body movement. Located in the labyrinths of the inner ear, in two components: 1. Vestibular sacs - gravity & head direction 2. Semicircular canals - angular acceleration (changes in the rotation of the head, not steady rotation) 1. Vestibular sacs (Otolith organs) - made of: a) Utricle (“little pouch”) b) Saccule (“little sac”) Signaling mechanism of Vestibular sacs Receptive organ located on the “floor” of Utricle and on “wall” of Saccule when head is in upright position - crystals move within gelatinous mass upon head movement; - crystals slightly bend cilia of hair cells also located within gelatinous mass; - this increases or decreases rate of action potentials in bipolar vestibular sensory neurons. Otoconia: Calcium carbonate crystals Gelatinous mass Cilia Hair cells Vestibular nerve Vestibular ganglion 2. Semicircular canals: 3 ring structures; each filled with fluid, separated by a membrane. Signaling mechanism of Semicircular canals -head movement induces movement of endolymph, but inertial resistance of endolymph slightly bends cupula (endolymph movement is initially slower than head mvmt); - cupula bending slightly moves the cilia of hair cells; - this bending changes rate of action potentials in bipolar vestibular sensory neurons; - when head movement stops: endolymph movement continues for slightly longer, again bending the cupula but in reverse direction on hair cells which changes rate of APs; - detects “acceleration” -

A Place Principle for Vertigo
Auris Nasus Larynx 35 (2008) 1–10 www.elsevier.com/locate/anl A place principle for vertigo Richard R. Gacek * Department of Otolaryngology, Head and Neck Surgery, University of Massachusetts Medical School, Worcester, MA 01655, USA Received 16 March 2007; accepted 13 April 2007 Available online 24 October 2007 Abstract Objective: To provide a road map of the vestibular labyrinth and its innervation leading to a place principle for different forms of vertigo. Method: The literature describing the anatomy and physiology of the vestibular system was reviewed. Results: Different forms of vertigo may be determined by the type of sense organ, type of ganglion cell and location in the vestibular nerve. Conclusion: Partial lesions (viral) of the vestibular ganglion are manifested as various forms of vertigo. # 2007 Elsevier Ireland Ltd. All rights reserved. Keywords: Vertigo; Vestibular nerve; Pathology Contents 1. Introduction . ............................................................................... 1 2. Sense organ. ............................................................................... 2 3. Ganglion cells ............................................................................... 4 4. Hair cells . ............................................................................... 5 5. Hair cell polarization . ....................................................................... 5 6. Efferent vestibular system ....................................................................... 8 7. A place principle for vertigo . ................................................................. -

Cochleovestibular Nerve Development Is Integrated with Migratory Neural Crest Cells
Developmental Biology 385 (2014) 200–210 Contents lists available at ScienceDirect Developmental Biology journal homepage: www.elsevier.com/locate/developmentalbiology Cochleovestibular nerve development is integrated with migratory neural crest cells Lisa L. Sandell a,n, Naomi E. Butler Tjaden b,c, Amanda J. Barlow d, Paul A. Trainor b,c a University of Louisville, Department of Molecular, Cellular and Craniofacial Biology, Louisville, KY 40201, USA b Stowers Institute for Medical Research, Kansas City, MO 64110, USA c Department of Anatomy and Cell Biology, University of Kansas Medical Center, Kansas City, KS 66160, USA d Department of Surgery, University of Wisconsin, Madison, WI 53792, USA article info abstract Article history: The cochleovestibular (CV) nerve, which connects the inner ear to the brain, is the nerve that enables the Received 28 August 2013 senses of hearing and balance. The aim of this study was to document the morphological development of Received in revised form the mouse CV nerve with respect to the two embryonic cells types that produce it, specifically, the otic 1 November 2013 vesicle-derived progenitors that give rise to neurons, and the neural crest cell (NCC) progenitors that give Accepted 8 November 2013 rise to glia. Otic tissues of mouse embryos carrying NCC lineage reporter transgenes were whole mount Available online 16 November 2013 immunostained to identify neurons and NCC. Serial optical sections were collected by confocal Keywords: microscopy and were compiled to render the three dimensional (3D) structure of the developing CV Ear nerve. Spatial organization of the NCC and developing neurons suggest that neuronal and glial Otic populations of the CV nerve develop in tandem from early stages of nerve formation. -
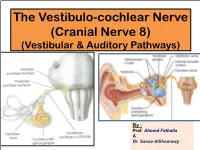
The Vestibulo-Cochlear Nerve (Cranial Nerve 8) (Vestibular & Auditory Pathways)
The Vestibulo-cochlear Nerve (Cranial Nerve 8) (Vestibular & Auditory Pathways) By : Prof. Ahmed Fathalla & Dr. Sanaa AlShaarawy OBJECTIVES At the end of the lecture, the students should be able to: qList the nuclei related to vestibular and cochlear nerves in the brain stem. qDescribe the type and site of each nucleus. qDescribe the vestibular pathways and its main connections. qDescribe the auditory pathway and its main connections. BRAIN – VENTRAL SURFACE Ponto-medullary Sulcus (cerebello- pontine angle) Vestibulo-Cochlear Nerve • Type: Special sensory (SSA) • Conveys impulses from inner ear to nervous system. • Components: § Vestibular part: conveys impulses associated with body posture ,balance and coordination of head & eye movements. § Cochlear part: conveys impulses associated with hearing. • Vestibular & cochlear parts leave the ventral surface of brain stem through the pontomedullary sulcus ‘at crebellopontine angle’ (lateral to facial nerve), run laterally in posterior cranial fossa and enter the internal acoustic meatus along with 7th nerve. Vestibular Nerve • The cell bodies (1st order neurons) are Vestibular nuclei belong to located in the vestibular ganglion special somatic afferent within the internal auditory meatus. column in brain stem. • The Peripheral processes (vestibular nerve fibers) make dendritic contact with hair cells of the membranous labyrinth (inner ear). 2 • The central processes (form the vestibular nerve) ‘’Efferent Fibres’’ : 1. Mostly end up in the lateral, medial, inferior and superior 1 vestibular nuclei (2nd order neurons) of the rostral medulla, located beneath the lateral part of the floor of 4th ventricle 2. Some fibers go to the cerebellum through the inferior cerebellar peduncle • Other Efferents from the vestibular nuclei project to other regions for the maintenance of balance, conscious awareness of vestibular stimulation , co-ordination of head & eye movements and control the posture. -

Cranial Nerve Disorders: Clinical Manifestations and Topographyଝ
Radiología. 2019;61(2):99---123 www.elsevier.es/rx UPDATE IN RADIOLOGY Cranial nerve disorders: Clinical manifestations and topographyଝ a,∗ a b c M. Jorquera Moya , S. Merino Menéndez , J. Porta Etessam , J. Escribano Vera , a M. Yus Fuertes a Sección de Neurorradiología, Hospital Clínico San Carlos, Madrid, Spain b Servicio de Neurología, Hospital Clínico San Carlos, Madrid, Spain c Neurorradiología, Hospital Ruber Internacional, Madrid, Spain Received 17 November 2017; accepted 27 September 2018 KEYWORDS Abstract The detection of pathological conditions related to the twelve cranial pairs rep- Cranial pairs; resents a significant challenge for both clinicians and radiologists; imaging techniques are Cranial nerves; fundamental for the management of many patients with these conditions. In addition to knowl- Cranial neuropathies; edge about the anatomy and pathological entities that can potentially affect the cranial pairs, Neuralgia; the imaging evaluation of patients with possible cranial pair disorders requires specific exami- Cranial nerve palsy nation protocols, acquisition techniques, and image processing. This article provides a review of the most common symptoms and syndromes related with the cranial pairs that might require imaging tests, together with a brief overview of the anatomy, the most common underlying processes, and the most appropriate imaging tests for different indications. © 2018 SERAM. Published by Elsevier Espana,˜ S.L.U. All rights reserved. PALABRAS CLAVE Sintomatología derivada de los pares craneales: Clínica y topografía Pares craneales; Resumen La detección de la patología relacionada con los doce pares craneales representa Nervios craneales; un importante desafío, tanto para los clínicos como para los radiólogos. Las técnicas de imagen Neuropatía de pares craneales; son fundamentales para el manejo de muchos de los pacientes. -

The Vestibulocochlear Nerve (VIII)
Diagnostic and Interventional Imaging (2013) 94, 1043—1050 . CONTINUING EDUCATION PROGRAM: FOCUS . The vestibulocochlear nerve (VIII) a,∗ b a F. Benoudiba , F. Toulgoat , J.-L. Sarrazin a Department of neuroradiology, Kremlin-Bicêtre university hospital, 78, rue du Général-Leclerc, 94275 Le Kremlin-Bicêtre, France b Diagnostic and interventional neuroradiology, Laennec hospital, Nantes university hospitals, boulevard Jacques-Monod, Saint-Herblain, 44093 Nantes cedex 1, France KEYWORDS Abstract The vestibulocochlear nerve (8th cranial nerve) is a sensory nerve. It is made up of Cranial nerves; two nerves, the cochlear, which transmits sound and the vestibular which controls balance. It is Pathology; an intracranial nerve which runs from the sensory receptors in the internal ear to the brain stem Vestibulocochlear nuclei and finally to the auditory areas: the post-central gyrus and superior temporal auditory nerve (VIII) cortex. The most common lesions responsible for damage to VIII are vestibular Schwannomas. This report reviews the anatomy and various investigations of the nerve. © 2013 Published by Elsevier Masson SAS on behalf of the Éditions françaises de radiologie. The cochlear nerve Review of anatomy [1] The cochlear nerve has a peripheral sensory origin and follows a centripetal path. It ori- ginates in the cochlear membrane sensory canal, forming the spiral organ (the organ of Corti) and lies on the basilar membrane (Fig. 1). The neuronal fibers of the protoneu- ron connect to the ciliated cells on the spiral lamina (Fig. 2). The axons are grouped together along the axis of the cochlea (modiolus), forming the cochlear nerve which then enters the internal auditory meatus (IAM). Within the internal auditory meatus, the nerve joins the vestibular nerve to form the vestibulocochlear nerve which crosses the cere- bellopontine angle (Figs.