Annual Technical Report 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
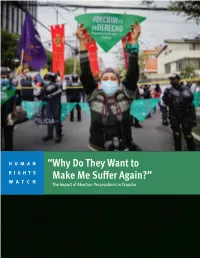
“Why Do They Want to Make Me Suffer Again?” the Impact of Abortion Prosecutions in Ecuador
HUMAN “Why Do They Want to RIGHTS WATCH Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador “Why Do They Want to Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador Copyright © 2021 Human Rights Watch All rights reserved. Printed in the United States of America ISBN: 978-1-62313-919-3 Cover design by Rafael Jimenez Human Rights Watch defends the rights of people worldwide. We scrupulously investigate abuses, expose the facts widely, and pressure those with power to respect rights and secure justice. Human Rights Watch is an independent, international organization that works as part of a vibrant movement to uphold human dignity and advance the cause of human rights for all. Human Rights Watch is an international organization with staff in more than 40 countries, and offices in Amsterdam, Beirut, Berlin, Brussels, Chicago, Geneva, Goma, Johannesburg, London, Los Angeles, Moscow, Nairobi, New York, Paris, San Francisco, Sydney, Tokyo, Toronto, Tunis, Washington DC, and Zurich. For more information, please visit our website: http://www.hrw.org JULY 2021 ISBN: 978-1-62313-919-3 “Why Do They Want to Make Me Suffer Again?” The Impact of Abortion Prosecutions in Ecuador Summary ........................................................................................................................... 1 Key Recommendations ....................................................................................................... 8 To the Presidency ................................................................................................................... -
Abortion and the Law in New
NSW PARLIAMENTARY LIBRARY RESEARCH SERVICE Abortion and the law in New South Wales by Talina Drabsch Briefing Paper No 9/05 ISSN 1325-4456 ISBN 0 7313 1784 X August 2005 © 2005 Except to the extent of the uses permitted under the Copyright Act 1968, no part of this document may be reproduced or transmitted in any form or by any means including information storage and retrieval systems, without the prior written consent from the Librarian, New South Wales Parliamentary Library, other than by Members of the New South Wales Parliament in the course of their official duties. Abortion and the law in New South Wales by Talina Drabsch NSW PARLIAMENTARY LIBRARY RESEARCH SERVICE David Clune (MA, PhD, Dip Lib), Manager..............................................(02) 9230 2484 Gareth Griffith (BSc (Econ) (Hons), LLB (Hons), PhD), Senior Research Officer, Politics and Government / Law .........................(02) 9230 2356 Talina Drabsch (BA, LLB (Hons)), Research Officer, Law ......................(02) 9230 2768 Lenny Roth (BCom, LLB), Research Officer, Law ...................................(02) 9230 3085 Stewart Smith (BSc (Hons), MELGL), Research Officer, Environment ...(02) 9230 2798 John Wilkinson (MA, PhD), Research Officer, Economics.......................(02) 9230 2006 Should Members or their staff require further information about this publication please contact the author. Information about Research Publications can be found on the Internet at: www.parliament.nsw.gov.au/WEB_FEED/PHWebContent.nsf/PHPages/LibraryPublications Advice on -

Defending the Human Right to Life in Latin America
Defending the Human Right to Life in Latin America Translated from the Spanish Americans United for Life, Washington, DC 20005 Copyright © 2012 by Americans United for Life All rights reserved First edition published 2012 Published in the United States of America ISBN 978-0-9777204-8-4 Defending the Human Right to Life in Latin America Dr. Charmaine Yoest, President & CEO Editors M. Laura Farfán Bertrán, Lawyer & Project Coordinator William L. Saunders, Senior Vice President & Senior Counsel Jeanneane Maxon, Vice President of External Affairs & Corporate Counsel Translator Noelia Estefanía Marchetti Translated from the Spanish Copyright 2012 by Americans United for Life. All rights reserved under International and Pan-American Copyright Conventions. No part of Defending the Human Right to Life in Latin América may be reproduced or transmitted in any form, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system now known or to be invented, without permission in writing from the publisher, except by a reviewer who wishes to quote brief passages in an article or a review written for inclusion in a magazine, newspaper, or broadcast. For information, please contact: Americans United for Life 655 15th Street NW, Suite 410, Washington, DC 20005, United States of America; 202-289-1478 www.aul.org Table of Contents Introduction – Human Rights and the Right to Life William L. Saunders 11 Overview – Latin America Reaffirms its Commitment to Life M. Laura Farfán Bertrán 15 Legislation Guidelines for Latin America 21 I. General Guidelines to a Constitutional Amendment 21 II. Prohibition of Hormonal “Emergency Contraception” 22 III. Rights Acknowledgement 23 A. -

Global Justice Center
Submission to the Committee against Torture in relation to its examination of the United States of America’s Third to Fifth State Party Report The United States’ Abortion Restrictions on Foreign Assistance Deny Safe Abortion Services to Women and Girls Raped in Armed Conflict November 2014 2 United States: GJC & OMCT Submission to the Committee against Torture Table of Contents I. Executive Summary................................................................................................................... 3 II. Introduction ................................................................................................................................ 4 III. The Organizations Submitting this Report ....................................................................... 6 IV. US Abortion Restrictions on Foreign Assistance ............................................................ 7 V. Denial of Abortions Causes Severe Physical and Mental Pain and Suffering ........ 9 VI. Growing International Recognition that War Rape Victims Require Abortion Services and that the Denial of Abortion Constitutes Torture or Cruel, Inhuman or Degrading Treatment ....................................................................................................... 12 VII. US Responsibility to Prevent Torture and Ill-Treatment .......................................... 14 VIII. The Denial of Abortion Services to War Rape Victims is Discriminatory ............ 16 IX. US Abortion Restrictions Deny Rehabilitation from Rape ....................................... -
Abortion Facts and Figures 2021
ABORTION FACTS & FIGURES 2021 ABORTION FACTS & FIGURES TABLE OF CONTENTS PART ONE Introduction . 1 Global Overview . 2 African Overview . 4 By the Numbers . 6 Maternal Health . .9 Safe Abortion . 11 Unsafe Abortion . 13 Post-Abortion Care . 15 Contraception . 17 Unmet Need for Family Planning . 22 Abortion Laws and Policies . 24. PART TWO Glossary . 28 Appendix I: International Conventions . 30. Appendix II: How Unsafe Abortions Are Counted . 32 Appendix III: About the Sources . .33 Regional Data for Africa . 34 Regional Data for Asia . 44 Regional Data for Latin America and the Caribbean . 54. POPULATION REFERENCE BUREAU Population Reference Bureau INFORMS people around the world about population, health, and the environment, and EMPOWERS them to use that information to ADVANCE the well-being of current and future generations . This guide was written by Deborah Mesce, former PRB program director, international media training . The graphic designer was Sean Noyce . Thank you to Alana Barton, director of media programs; AÏssata Fall, senior policy advisor; Charlotte Feldman-Jacobs, former associate vice president; Kate P . Gilles, former program director; Tess McLoud, policy analyst; Cathryn Streifel, senior policy advisor; and Heidi Worley, senior writer; all at PRB, for their inputs and guidance . Thank you as well to Anneka Van Scoyoc, PRB senior graphic designer, for guiding the design process . © 2021 Population Reference Bureau . All rights reserved . This publication is available in print and on PRB’s website . To become a PRB member or to order PRB materials, contact us at: 1875 Connecticut Ave ., NW, Suite 520 Washington, DC 20009-5728 PHONE: 1-800-877-9881 E-MAIL: communications@prb .org WEB: www .prb .org For permission to reproduce parts of this publication, contact PRB at permissions@prb org. -

Northern Ireland Barriers to Accessing Abortion Services
NORTHERN IRELAND BARRIERS TO ACCESSING ABORTION SERVICES Amnesty International Publications First published in 2015 by Amnesty International Publications International Secretariat Peter Benenson House 1 Easton Street London WC1X 0DW United Kingdom www.amnesty.org © Amnesty International Publications 2015 Index: EUR 45/0157/2015 Original Language: English Printed by Amnesty International, International Secretariat, United Kingdom All rights reserved. This publication is copyright, but may be reproduced by any method without fee for advocacy, campaigning and teaching purposes, but not for resale. The copyright holders request that all such use be registered with them for impact assessment purposes. For copying in any other circumstances, or for reuse in other publications, or for translation or adaptation, prior written permission must be obtained from the publishers, and a fee may be payable. To request permission, or for any other inquiries, please contact [email protected] Amnesty International is a global movement of more than 3 million supporters, members and activists in more than 150 countries and territories who campaign to end grave abuses of human rights. Our vision is for every person to enjoy all the rights enshrined in the Universal Declaration of Human Rights and other international human rights standards. We are independent of any government, political ideology, economic interest or religion and are funded mainly by our membership and public donations. CONTENTS Executive summary ...................................................................................................... -

Reasons Why We Need to Decriminalize Abortion by Clara Rita A
EnGendeRights, Inc. Asserting Gender Equality Reasons Why We Need to Decriminalize Abortion By Clara Rita A. Padilla 1) To save women’s lives and prevent disability from unsafe abortion complications No woman should die or suffer disability from unsafe abortion complications.1 Deaths from unsafe abortion complications are preventable deaths with access to safe abortion2 and post-abortion care. This bill when passed into law will save the lives of thousands of women. The restrictive, colonial, and antiquated 1930 Revised Penal Code abortion law never reduced the number of women inducing abortion. It has only endangered the lives of hundreds of thousands of Filipino women who are forced to undergo unsafe abortion. Prosecution of women who induce abortion and those assisting them is not the answer. Despite the restrictive abortion law and without access to appropriate medical information, supplies and trained health providers, Filipino women, especially poor women with at least three children, have made personal decisions to induce abortion clandestinely and under unsafe conditions risking their lives and health. In 2012 alone, 610,000 Filipino women induced abortion, over 100,000 women were hospitalized, 3 and 1000 women died due to unsafe abortion complications.4 Based on statistics, the number of induced abortions increases proportionately with the increasing Philippine population.5 This 2012 statistics show that lack of access to safe and legal abortion has a grave public health impact on women’s lives and health translating to: • 3 women dying every day from unsafe abortion complications6 • 11 women hospitalized every hour 7 • 70 women induce abortion every hour8 Each year, complications from unsafe abortion is one of the five leading causes of maternal death— between 4.7% – 13.2%—and a leading cause of hospitalization in the Philippines.9 The high number of women dying yearly from complications from unsafe abortion surpass even the number of people who die from dengue. -
Forced Abortion and Sterilization in China: the View from the Inside
FORCED ABORTION AND STERILIZATION IN CHINA: THE VIEW FROM THE INSIDE HEARING BEFORE THE SUBCOMMITTEE ON INTERNATIONAL OPERATIONS AND HUMAN RIGHTS OF THE COMMITTEE ON INTERNATIONAL RELATIONS HOUSE OF REPRESENTATIVES ONE HUNDRED FIFTH CONGRESS SECOND SESSION JUNE 10, 1998 Printed for the use of the Committee on International Relations 0 U.S. GOVERNMENT PRINTING OFFICE 49-740 CC WASHINGTON : 1998 For sale by the U.S. Government Printing Office Superintendent of Documents, Congressional Sales Office, Washington, DC 20402 ISBN 0-16-057398-X o -J44-4 COMMITTEE ON INTERNATIONAL RELATIONS BENJAMIN A. GILMAN, New York, Chairman WILLIAM GOODLING, Pennsylvania LEE HAMILTON, Indiana JAMES A. LEACH, Iowa SAM GEJDENSON, Connecticut HENRY J. HYDE, Illinois TOM LANTOS, California DOUG BEREUTER, Nebraska HOWARD BERMAN, California CHRISTOPHER SMITH, New Jersey GARY ACKERMAN, New York DAN BURTON, Indiana ENI F.H. FALEOMAVAEGA, American ELTON GALLEGLY, California Samoa ILEANA ROS-LEHTINEN, Florida MATTHEW G. MARTINEZ, California CASS BALLENGER, North Carolina DONALD M. PAYNE, New Jersey DANA ROHRABACHER, California ROBERT ANDREWS, New Jersey DONALD A. MANZULLO, Illinois ROBERT MENENDEZ, New Jersey EDWARD R. ROYCE, California SHERROD BROWN, Ohio PETER T. KING, New York CYNTHIA A. McKINNEY, Georgia JAY KIM, California ALCEE L. HASTINGS, Florida STEVEN J. CHABOT, Ohio PAT DANNER, Missouri MARSHALL "MARK" SANFORD, South EARL HILLIARD, Alabama Carolina BRAD SHERMAN, California MATT SALMON, Arizona ROBERT WEXLER, Florida AMO HOUGHTON, New York STEVE ROTHMAN, New Jersey TOM CAMPBELL, California BOB CLEMENT, Tennessee JON FOX, Pennsylvania BILL LUTHER, Minnesota JOHN McHUGH, New York JIM DAVIS, Florida LINDSEY GRAHAM, South Carolina LOIS CAPPS, California ROY BLUNT, Missouri KEVIN BRADY, Texas RICHARD BURR, North Carolina RICHARD J. -
2010-2011 GEMMA Annual Report
GEMMA Fund Annual Report 2010-2011 Developed and designed by Darcy White, Kavitha Balakumar and Danielle Fincher. March 2012. Mission The GEMMA Fund supports Emory University public health graduate students’ research and their collaborations with public health organizations, including the publishing and publicity of student research !ndings in order to contribute to the prevention of maternal deaths from abortion. Background According to the World Health Organization (WHO), in 2008 about 21.6 million women obtained unsafe abortions and 47,000 women died from abortion-related complications. If the 55 million women who have abortions each year worldwide were to obtain abortions as safely as women in the United States, fewer than 100 women world-wide would die as a result of the abortion. Moreover, WHO reports that unsafe abortions are virtually absent and overall abortion rates are lower in countries with less-restrictive abortion laws.* In response to reports of continuing high maternal mortality from abortion in many other countries, sometimes even neglected in safe motherhood strategies, the GEMMA Fund believes that improved surveillance of maternal deaths and complications associated with abortion and monitoring and evaluation of appropriate interventions will help to eliminate these deaths. To encourage scholarship toward this speci!c public health goal, Dr. Roger and Susan Rochat of the Rollins School of Public Health (RSPH) have established an endowed fund known as the Global Elimination of Maternal Mortality due to Abortion (GEMMA) Fund dedicated to the prevention of maternal deaths from abortion. * World Health Organization (WHO), Unsafe Abortion: Global and Regional Estimates of the Incidence of Unsafe Abortion and Associated Mortality in 2008, sixth ed., Geneva: WHO, 2011. -

Sharing Responsibility: Women, Society and Abortion Worldwide
SHARINGTHEALANGUTTMACHERINSTITUTE RESPONSIBILITYWOMEN SOCIETY &ABORTION WORLDWIDE STHE HALAN AGUTTMACHERRIN INSTITUTEG RESPONSIBILITY WOMEN SOCIETY &ABORTION WORLDWIDE Acknowledgments haring Responsibility: Women, Society and Pathfinder International, Peru; Tomas Frejka, independent Abortion Worldwide brings together research consultant, United States; Adrienne Germain, International findings about induced abortion and Women’s Health Coalition, United States; Forrest S unplanned pregnancy from the work of The Greenslade, Harrison McKay and Judith Winkler, Ipas, Alan Guttmacher Institute (AGI), assisted by a large num- United States; Dale Huntington, Population Council, ber of individuals and organizations. Susheela Singh, direc- Egypt and United States; Ngozi Iwere, Community Life tor of research at AGI, oversaw the development of this Project, Nigeria; Shireen Jejeebhoy, consultant, Special report, which is based on analyses conducted by her, Programme of Research, Development and Research Stanley Henshaw, deputy director of research, Akinrinola Training in Human Reproduction, World Health Bankole, senior research associate, and Taylor Haas, research Organization, Switzerland and India; Evert Ketting, inter- associate. Deirdre Wulf, independent consultant, wrote the national consultant on family planning and sexual and report, which was edited by Dore Hollander, senior editor, reproductive health, Netherlands; Firman Lubis, Yayasan and Jeanette Johnson, director of publications. Kusuma Buana, Indonesia; Paulina Makinwa-Adebusoye, The -

Privacy Protection for Doctors Who Performed Abortions
WANTED: PRIVACY PROTECTION FOR DOCTORS WHO PERFORM ABORTIONS ANGELA CHRISTINA COUCH* INTRODUCTION Since 1993, abortion-related violence has been increasingly in the news.' Patients, abortion protesters, and pro-choice groups all have been affected, but the doctors who perform abortions have most recently been the target of much of the and-abortion violence. In an effort to make abortions unavailable, many pro-life groups have resorted to exposure campaigns aimed at disclosing to the general public the names of doctors who perform abortions.' Fearing such exposure will- cost them their lives, many doctors are taking radical * Emory University School of Law, Candidate forJuris Doctor, May 1996. The Author would like to thank Dean Howard 0. Hunter, Karen Ann Ballotta, Barbara Rochelle, and Karyn Hudson for their guidance in writing this Comment. The Author is also indebted to the following individuals for their tremendous editing efforts: Regan M. Greene Sandra Bernstein, Crystal S. Deese, Marcella R. Eckels, Troy W. Garris, Zahra S. Karinshak, and Amy Schaner Stanley. The Author is eternally grateful to Khoi Nguyen for his dedication, patience, and understanding. 1. MorningEdition(NPR radio broadcast, Feb. 3,1995) (1995 WL 2957329). "The statistics are only too familiar;, five murders at clinics in less than two years, 400 death threats in 1994 alone. In the last dozen years, according to the Bureau of.Alcohol Tobacco and Firearms, there have been 37 bombings in 33 states, 123 cases of arson, 1,500 cases of assault, stalking, sabotage, and burglary, and some $13 million in property damage." Id 2. See William Booth, Abortion Battle Fatigue; Slain Physician's Replacement Vents Fears, Frustration, WASH. -

A CRIME the Threat to Vulnerable Women in Latin America
WHEN ABORTION IS A CRIME The threat to vulnerable women in Latin America Health. Access. Rights. ISBN: 1–933095–73–3 © Ipas 2013, 2014 Produced in the United States of America Suggested citation: Kane, G., Galli, B., & Skuster, P. (2013). When abortion is a crime: The threat to vulnerable women in Latin America (third ed.) Chapel Hill, NC: Ipas. Ipas is a nonprofit organization that works around the world to increase women’s ability to exercise their sexual and reproductive rights, especially the right to safe abor- tion. We seek to eliminate unsafe abortion and the result- ing deaths and injuries and to expand women’s access to comprehensive abortion care, including contraception and related reproductive health information and care. We strive to foster a legal, policy and social environment sup- portive of women’s rights to make their own sexual and reproductive health decisions freely and safely. Ipas is a registered 501(c)(3) nonprofit organization. All contributions to Ipas are tax deductible to the full extent allowed by law. For more information or to donate to Ipas: Ipas P.O. Box 9990 Chapel Hill, NC 27515 USA 1.919.967.7052 [email protected] www.ipas.org The photographs used in this publication are for illustra- tive purposes only; they do not imply any particular atti- tudes, behaviors, or actions on the part of any person who appears in the photographs. WHEN ABORTION IS A CRIME The threat to vulnerable women in Latin America Authors: Gillian Kane, Senior Policy Advisor, Ipas Beatriz Galli, Latin America Policy Associate, Ipas Patty