Plus Cylinder Subjective Refraction, for Clinicans
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Examples of Manifolds
Examples of Manifolds Example 1 (Open Subset of IRn) Any open subset, O, of IRn is a manifold of dimension n. One possible atlas is A = (O, ϕid) , where ϕid is the identity map. That is, ϕid(x) = x. n Of course one possible choice of O is IR itself. Example 2 (The Circle) The circle S1 = (x,y) ∈ IR2 x2 + y2 = 1 is a manifold of dimension one. One possible atlas is A = {(U , ϕ ), (U , ϕ )} where 1 1 1 2 1 y U1 = S \{(−1, 0)} ϕ1(x,y) = arctan x with − π < ϕ1(x,y) <π ϕ1 1 y U2 = S \{(1, 0)} ϕ2(x,y) = arctan x with 0 < ϕ2(x,y) < 2π U1 n n n+1 2 2 Example 3 (S ) The n–sphere S = x =(x1, ··· ,xn+1) ∈ IR x1 +···+xn+1 =1 n A U , ϕ , V ,ψ i n is a manifold of dimension . One possible atlas is 1 = ( i i) ( i i) 1 ≤ ≤ +1 where, for each 1 ≤ i ≤ n + 1, n Ui = (x1, ··· ,xn+1) ∈ S xi > 0 ϕi(x1, ··· ,xn+1)=(x1, ··· ,xi−1,xi+1, ··· ,xn+1) n Vi = (x1, ··· ,xn+1) ∈ S xi < 0 ψi(x1, ··· ,xn+1)=(x1, ··· ,xi−1,xi+1, ··· ,xn+1) n So both ϕi and ψi project onto IR , viewed as the hyperplane xi = 0. Another possible atlas is n n A2 = S \{(0, ··· , 0, 1)}, ϕ , S \{(0, ··· , 0, −1)},ψ where 2x1 2xn ϕ(x , ··· ,xn ) = , ··· , 1 +1 1−xn+1 1−xn+1 2x1 2xn ψ(x , ··· ,xn ) = , ··· , 1 +1 1+xn+1 1+xn+1 are the stereographic projections from the north and south poles, respectively. -

An Introduction to Topology the Classification Theorem for Surfaces by E
An Introduction to Topology An Introduction to Topology The Classification theorem for Surfaces By E. C. Zeeman Introduction. The classification theorem is a beautiful example of geometric topology. Although it was discovered in the last century*, yet it manages to convey the spirit of present day research. The proof that we give here is elementary, and its is hoped more intuitive than that found in most textbooks, but in none the less rigorous. It is designed for readers who have never done any topology before. It is the sort of mathematics that could be taught in schools both to foster geometric intuition, and to counteract the present day alarming tendency to drop geometry. It is profound, and yet preserves a sense of fun. In Appendix 1 we explain how a deeper result can be proved if one has available the more sophisticated tools of analytic topology and algebraic topology. Examples. Before starting the theorem let us look at a few examples of surfaces. In any branch of mathematics it is always a good thing to start with examples, because they are the source of our intuition. All the following pictures are of surfaces in 3-dimensions. In example 1 by the word “sphere” we mean just the surface of the sphere, and not the inside. In fact in all the examples we mean just the surface and not the solid inside. 1. Sphere. 2. Torus (or inner tube). 3. Knotted torus. 4. Sphere with knotted torus bored through it. * Zeeman wrote this article in the mid-twentieth century. 1 An Introduction to Topology 5. -
The Sphere Project
;OL :WOLYL 7YVQLJ[ +XPDQLWDULDQ&KDUWHUDQG0LQLPXP 6WDQGDUGVLQ+XPDQLWDULDQ5HVSRQVH ;OL:WOLYL7YVQLJ[ 7KHULJKWWROLIHZLWKGLJQLW\ ;OL:WOLYL7YVQLJ[PZHUPUP[PH[P]L[VKL[LYTPULHUK WYVTV[LZ[HUKHYKZI`^OPJO[OLNSVIHSJVTT\UP[` /\THUP[HYPHU*OHY[LY YLZWVUKZ[V[OLWSPNO[VMWLVWSLHMMLJ[LKI`KPZHZ[LYZ /\THUP[HYPHU >P[O[OPZ/HUKIVVR:WOLYLPZ^VYRPUNMVYH^VYSKPU^OPJO [OLYPNO[VMHSSWLVWSLHMMLJ[LKI`KPZHZ[LYZ[VYLLZ[HISPZO[OLPY *OHY[LYHUK SP]LZHUKSP]LSPOVVKZPZYLJVNUPZLKHUKHJ[LK\WVUPU^H`Z[OH[ YLZWLJ[[OLPY]VPJLHUKWYVTV[L[OLPYKPNUP[`HUKZLJ\YP[` 4PUPT\T:[HUKHYKZ This Handbook contains: PU/\THUP[HYPHU (/\THUP[HYPHU*OHY[LY!SLNHSHUKTVYHSWYPUJPWSLZ^OPJO HUK YLÅLJ[[OLYPNO[ZVMKPZHZ[LYHMMLJ[LKWVW\SH[PVUZ 4PUPT\T:[HUKHYKZPU/\THUP[HYPHU9LZWVUZL 9LZWVUZL 7YV[LJ[PVU7YPUJPWSLZ *VYL:[HUKHYKZHUKTPUPT\TZ[HUKHYKZPUMV\YRL`SPMLZH]PUN O\THUP[HYPHUZLJ[VYZ!>H[LYZ\WWS`ZHUP[H[PVUHUKO`NPLUL WYVTV[PVU"-VVKZLJ\YP[`HUKU\[YP[PVU":OLS[LYZL[[SLTLU[HUK UVUMVVKP[LTZ"/LHS[OHJ[PVU;OL`KLZJYPILwhat needs to be achieved in a humanitarian response in order for disaster- affected populations to survive and recover in stable conditions and with dignity. ;OL:WOLYL/HUKIVVRLUQV`ZIYVHKV^ULYZOPWI`HNLUJPLZHUK PUKP]PK\HSZVMMLYPUN[OLO\THUP[HYPHUZLJ[VYH common language for working together towards quality and accountability in disaster and conflict situations ;OL:WOLYL/HUKIVVROHZHU\TILYVMºJVTWHUPVU Z[HUKHYKZ»L_[LUKPUNP[ZZJVWLPUYLZWVUZL[VULLKZ[OH[ OH]LLTLYNLK^P[OPU[OLO\THUP[HYPHUZLJ[VY ;OL:WOLYL7YVQLJ[^HZPUP[PH[LKPU I`HU\TILY VMO\THUP[HYPHU5.6ZHUK[OL9LK*YVZZHUK 9LK*YLZJLU[4V]LTLU[ ,+0;065 7KHB6SKHUHB3URMHFWBFRYHUBHQBLQGG The Sphere Project Humanitarian Charter and Minimum Standards in Humanitarian Response Published by: The Sphere Project Copyright@The Sphere Project 2011 Email: [email protected] Website : www.sphereproject.org The Sphere Project was initiated in 1997 by a group of NGOs and the Red Cross and Red Crescent Movement to develop a set of universal minimum standards in core areas of humanitarian response: the Sphere Handbook. -
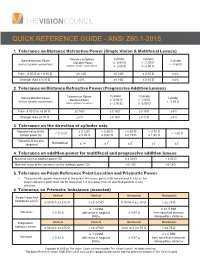
Quick Reference Guide - Ansi Z80.1-2015
QUICK REFERENCE GUIDE - ANSI Z80.1-2015 1. Tolerance on Distance Refractive Power (Single Vision & Multifocal Lenses) Cylinder Cylinder Sphere Meridian Power Tolerance on Sphere Cylinder Meridian Power ≥ 0.00 D > - 2.00 D (minus cylinder convention) > -4.50 D (minus cylinder convention) ≤ -2.00 D ≤ -4.50 D From - 6.50 D to + 6.50 D ± 0.13 D ± 0.13 D ± 0.15 D ± 4% Stronger than ± 6.50 D ± 2% ± 0.13 D ± 0.15 D ± 4% 2. Tolerance on Distance Refractive Power (Progressive Addition Lenses) Cylinder Cylinder Sphere Meridian Power Tolerance on Sphere Cylinder Meridian Power ≥ 0.00 D > - 2.00 D (minus cylinder convention) > -3.50 D (minus cylinder convention) ≤ -2.00 D ≤ -3.50 D From -8.00 D to +8.00 D ± 0.16 D ± 0.16 D ± 0.18 D ± 5% Stronger than ±8.00 D ± 2% ± 0.16 D ± 0.18 D ± 5% 3. Tolerance on the direction of cylinder axis Nominal value of the ≥ 0.12 D > 0.25 D > 0.50 D > 0.75 D < 0.12 D > 1.50 D cylinder power (D) ≤ 0.25 D ≤ 0.50 D ≤ 0.75 D ≤ 1.50 D Tolerance of the axis Not Defined ° ° ° ° ° (degrees) ± 14 ± 7 ± 5 ± 3 ± 2 4. Tolerance on addition power for multifocal and progressive addition lenses Nominal value of addition power (D) ≤ 4.00 D > 4.00 D Nominal value of the tolerance on the addition power (D) ± 0.12 D ± 0.18 D 5. Tolerance on Prism Reference Point Location and Prismatic Power • The prismatic power measured at the prism reference point shall not exceed 0.33Δ or the prism reference point shall not be more than 1.0 mm away from its specified position in any direction. -

Binocular Vision and the Stroop Test
1040-5488/16/9302-0194/0 VOL. 93, NO. 2, PP. 194Y208 OPTOMETRY AND VISION SCIENCE Copyright * 2015 American Academy of Optometry REVIEW Binocular Vision and the Stroop Test Franc¸ois Daniel* and ZoB Kapoula† ABSTRACT Purpose. Recent studies report a link between optometric results, learning disabilities, and problems in reading. This study examines the correlations between optometric tests of binocular vision, namely, of vergence and accommodation, reading speed, and cognitive executive functions as measured by the Stroop test. Methods. Fifty-one students (mean age, 20.43 T 1.25 years) were given a complete eye examination. They then performed the reading test L’Alouette and the Stroop interference test at their usual reading distance. Criteria for selection were the absence of significant refractive uncorrected error, strabismus, amblyopia, color vision defects, and other neurologic findings. Results. The results show a correlation between positive fusional vergences (PFVs) at near distance and the interference effect (IE) in the Stroop test: the higher the PFV value is, the less the IE. Furthermore, the subgroup of 11 students presenting convergence insufficiency, according to Scheiman and Wick criteria (2002), showed a significantly higher IE during the Stroop test than the other students (N = 18) who had normal binocular vision without symptoms at near. Importantly, there is no correlation between reading speed and PFV either for the entire sample or for the subgroups. Conclusions. These results suggest for the first time a link between convergence capacity and the interference score in the Stroop test. Such a link is attributable to the fact that vergence control and cognitive functions mobilize the same cortical areas, for example, parietofrontal areas. -
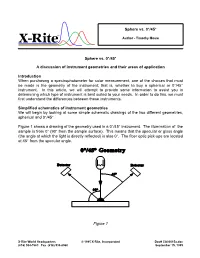
Sphere Vs. 0°/45° a Discussion of Instrument Geometries And
Sphere vs. 0°/45° ® Author - Timothy Mouw Sphere vs. 0°/45° A discussion of instrument geometries and their areas of application Introduction When purchasing a spectrophotometer for color measurement, one of the choices that must be made is the geometry of the instrument; that is, whether to buy a spherical or 0°/45° instrument. In this article, we will attempt to provide some information to assist you in determining which type of instrument is best suited to your needs. In order to do this, we must first understand the differences between these instruments. Simplified schematics of instrument geometries We will begin by looking at some simple schematic drawings of the two different geometries, spherical and 0°/45°. Figure 1 shows a drawing of the geometry used in a 0°/45° instrument. The illumination of the sample is from 0° (90° from the sample surface). This means that the specular or gloss angle (the angle at which the light is directly reflected) is also 0°. The fiber optic pick-ups are located at 45° from the specular angle. Figure 1 X-Rite World Headquarters © 1995 X-Rite, Incorporated Doc# CA00015a.doc (616) 534-7663 Fax (616) 534-8960 September 15, 1995 Figure 2 shows a drawing of the geometry used in an 8° diffuse sphere instrument. The sphere wall is lined with a highly reflective white substance and the light source is located on the rear of the sphere wall. A baffle prevents the light source from directly illuminating the sample, thus providing diffuse illumination. The sample is viewed at 8° from perpendicular which means that the specular or gloss angle is also 8° from perpendicular. -

And Minus Cylinder Subjective Refraction Techniques for Clinicians January 2016
Mark E Wilkinson, OD Plus and Minus Cylinder Subjective Refraction Techniques for Clinicians January 2016 General Refraction Techniques Prior to starting your refraction, baseline visual acuities (OD, OS and OU) must be determined. For individuals with near vision complaints, and all presbyopes, near acuity should also be documented using M notation, with the testing distance documented if different than 16 inches (40 centimeters). Accurately assessing visual acuity is important for many reasons. It allows the clinician to: § Determine best corrected acuity with refraction § Monitor the effect of treatment and/or progression of disease § Estimate the dioptric power of optical devices necessary for reading regular size print § Verify eligibility for tasks such as driving § Verify eligibility as “legally blind” When measuring distance acuity, there is no longer a need to measure visual acuity in a darkened room. In the past, when projected charts were used, the room lights had to be lowered for better contrast on the chart. Now, with high definition LCD monitor acuity charts and ETDRS charts, contrast is no longer an issue. Additionally, for some patients, particularly those with difficulties adjusting to lower lighting conditions, taking them from a normally lit waiting room into a darkened clinic or work up room will artificially lower their acuity, because they do not have enough time for their eyes to adjust to the lower light conditions. Because clinical decisions are based on these acuity measurements, accurate assessment of each person’s acuity is critically important. With this in mind, all acuity testing should be done with the overhead lights on in the exam or work up room. -

Recognizing Surfaces
RECOGNIZING SURFACES Ivo Nikolov and Alexandru I. Suciu Mathematics Department College of Arts and Sciences Northeastern University Abstract The subject of this poster is the interplay between the topology and the combinatorics of surfaces. The main problem of Topology is to classify spaces up to continuous deformations, known as homeomorphisms. Under certain conditions, topological invariants that capture qualitative and quantitative properties of spaces lead to the enumeration of homeomorphism types. Surfaces are some of the simplest, yet most interesting topological objects. The poster focuses on the main topological invariants of two-dimensional manifolds—orientability, number of boundary components, genus, and Euler characteristic—and how these invariants solve the classification problem for compact surfaces. The poster introduces a Java applet that was written in Fall, 1998 as a class project for a Topology I course. It implements an algorithm that determines the homeomorphism type of a closed surface from a combinatorial description as a polygon with edges identified in pairs. The input for the applet is a string of integers, encoding the edge identifications. The output of the applet consists of three topological invariants that completely classify the resulting surface. Topology of Surfaces Topology is the abstraction of certain geometrical ideas, such as continuity and closeness. Roughly speaking, topol- ogy is the exploration of manifolds, and of the properties that remain invariant under continuous, invertible transforma- tions, known as homeomorphisms. The basic problem is to classify manifolds according to homeomorphism type. In higher dimensions, this is an impossible task, but, in low di- mensions, it can be done. Surfaces are some of the simplest, yet most interesting topological objects. -

The Real Projective Spaces in Homotopy Type Theory
The real projective spaces in homotopy type theory Ulrik Buchholtz Egbert Rijke Technische Universität Darmstadt Carnegie Mellon University Email: [email protected] Email: [email protected] Abstract—Homotopy type theory is a version of Martin- topology and homotopy theory developed in homotopy Löf type theory taking advantage of its homotopical models. type theory (homotopy groups, including the fundamen- In particular, we can use and construct objects of homotopy tal group of the circle, the Hopf fibration, the Freuden- theory and reason about them using higher inductive types. In this article, we construct the real projective spaces, key thal suspension theorem and the van Kampen theorem, players in homotopy theory, as certain higher inductive types for example). Here we give an elementary construction in homotopy type theory. The classical definition of RPn, in homotopy type theory of the real projective spaces as the quotient space identifying antipodal points of the RPn and we develop some of their basic properties. n-sphere, does not translate directly to homotopy type theory. R n In classical homotopy theory the real projective space Instead, we define P by induction on n simultaneously n with its tautological bundle of 2-element sets. As the base RP is either defined as the space of lines through the + case, we take RP−1 to be the empty type. In the inductive origin in Rn 1 or as the quotient by the antipodal action step, we take RPn+1 to be the mapping cone of the projection of the 2-element group on the sphere Sn [4]. -

The Sphere Packing Problem in Dimension 8 Arxiv:1603.04246V2
The sphere packing problem in dimension 8 Maryna S. Viazovska April 5, 2017 8 In this paper we prove that no packing of unit balls in Euclidean space R has density greater than that of the E8-lattice packing. Keywords: Sphere packing, Modular forms, Fourier analysis AMS subject classification: 52C17, 11F03, 11F30 1 Introduction The sphere packing constant measures which portion of d-dimensional Euclidean space d can be covered by non-overlapping unit balls. More precisely, let R be the Euclidean d vector space equipped with distance k · k and Lebesgue measure Vol(·). For x 2 R and d r 2 R>0 we denote by Bd(x; r) the open ball in R with center x and radius r. Let d X ⊂ R be a discrete set of points such that kx − yk ≥ 2 for any distinct x; y 2 X. Then the union [ P = Bd(x; 1) x2X d is a sphere packing. If X is a lattice in R then we say that P is a lattice sphere packing. The finite density of a packing P is defined as Vol(P\ Bd(0; r)) ∆P (r) := ; r > 0: Vol(Bd(0; r)) We define the density of a packing P as the limit superior ∆P := lim sup ∆P (r): r!1 arXiv:1603.04246v2 [math.NT] 4 Apr 2017 The number be want to know is the supremum over all possible packing densities ∆d := sup ∆P ; d P⊂R sphere packing 1 called the sphere packing constant. For which dimensions do we know the exact value of ∆d? Trivially, in dimension 1 we have ∆1 = 1. -

Care of the Patient with Accommodative and Vergence Dysfunction
OPTOMETRIC CLINICAL PRACTICE GUIDELINE Care of the Patient with Accommodative and Vergence Dysfunction OPTOMETRY: THE PRIMARY EYE CARE PROFESSION Doctors of optometry are independent primary health care providers who examine, diagnose, treat, and manage diseases and disorders of the visual system, the eye, and associated structures as well as diagnose related systemic conditions. Optometrists provide more than two-thirds of the primary eye care services in the United States. They are more widely distributed geographically than other eye care providers and are readily accessible for the delivery of eye and vision care services. There are approximately 36,000 full-time-equivalent doctors of optometry currently in practice in the United States. Optometrists practice in more than 6,500 communities across the United States, serving as the sole primary eye care providers in more than 3,500 communities. The mission of the profession of optometry is to fulfill the vision and eye care needs of the public through clinical care, research, and education, all of which enhance the quality of life. OPTOMETRIC CLINICAL PRACTICE GUIDELINE CARE OF THE PATIENT WITH ACCOMMODATIVE AND VERGENCE DYSFUNCTION Reference Guide for Clinicians Prepared by the American Optometric Association Consensus Panel on Care of the Patient with Accommodative and Vergence Dysfunction: Jeffrey S. Cooper, M.S., O.D., Principal Author Carole R. Burns, O.D. Susan A. Cotter, O.D. Kent M. Daum, O.D., Ph.D. John R. Griffin, M.S., O.D. Mitchell M. Scheiman, O.D. Revised by: Jeffrey S. Cooper, M.S., O.D. December 2010 Reviewed by the AOA Clinical Guidelines Coordinating Committee: David A. -

Hyperbolic Geometry
Flavors of Geometry MSRI Publications Volume 31,1997 Hyperbolic Geometry JAMES W. CANNON, WILLIAM J. FLOYD, RICHARD KENYON, AND WALTER R. PARRY Contents 1. Introduction 59 2. The Origins of Hyperbolic Geometry 60 3. Why Call it Hyperbolic Geometry? 63 4. Understanding the One-Dimensional Case 65 5. Generalizing to Higher Dimensions 67 6. Rudiments of Riemannian Geometry 68 7. Five Models of Hyperbolic Space 69 8. Stereographic Projection 72 9. Geodesics 77 10. Isometries and Distances in the Hyperboloid Model 80 11. The Space at Infinity 84 12. The Geometric Classification of Isometries 84 13. Curious Facts about Hyperbolic Space 86 14. The Sixth Model 95 15. Why Study Hyperbolic Geometry? 98 16. When Does a Manifold Have a Hyperbolic Structure? 103 17. How to Get Analytic Coordinates at Infinity? 106 References 108 Index 110 1. Introduction Hyperbolic geometry was created in the first half of the nineteenth century in the midst of attempts to understand Euclid’s axiomatic basis for geometry. It is one type of non-Euclidean geometry, that is, a geometry that discards one of Euclid’s axioms. Einstein and Minkowski found in non-Euclidean geometry a This work was supported in part by The Geometry Center, University of Minnesota, an STC funded by NSF, DOE, and Minnesota Technology, Inc., by the Mathematical Sciences Research Institute, and by NSF research grants. 59 60 J. W. CANNON, W. J. FLOYD, R. KENYON, AND W. R. PARRY geometric basis for the understanding of physical time and space. In the early part of the twentieth century every serious student of mathematics and physics studied non-Euclidean geometry.