Contact Dermatitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D. Director of Ethnic Skin Care Voluntary Assistant Professor Miller/University of Miami School of Medicine Department of Dermatology and Cutaneous Surgery What Determines Skin Color? What Determines Skin Color? No significant difference in the number of melanocytes between the races 2000 epidermal melanocytes/mm2 on head and forearm 1000 epidermal melanocytes/mm2 on the rest of the body differences present at birth Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff,K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192-220, New York, NY: McGraw Hill Melanosomes in Black and White Skin Black White Szabo G, Gerald AB, Pathak MA, Fitzpatrick TB. Nature1969;222:1081-1082 Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff, K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192- 220, New York, NY: McGraw Hill Role of Melanin-Advantages Melanin absorbs and scatters energy from UV and visible light to protect epidermal cells from UV damage Disadvantages Inflammation or injury to the skin is almost immediately accompanied by alteration in pigmentation Hyperpigmentation Hypopigmentation Dyschromias Post-Inflammatory hyperpigmentation Acne Melasma Lichen Planus Pigmentosus Progressive Macular Hypomelanosis -

22 Asteatotic Eczema (Xerosis, Xerotic Eczema, Eczema Craquelé, Eczema Cannalé, Eczema Hiemalis, Winter Itch)
22 Asteatotic Eczema (Xerosis, Xerotic Eczema, Eczema Craquelé, Eczema Cannalé, Eczema Hiemalis, Winter Itch) INTRODUCTION This common dermatitis is often misdiagnosed and usually overtreated. Familiarity with the physical findings will allow an accurate assessment of the underlying cause, and symptoms can usually be corrected with simple measures. The condition occurs for a number of reasons, especially the following: 1. With age, skin sebum secretion diminishes, as does the water-holding capacity of the epidermis. These changes are particularly marked on the lower extremities. 2. Bathing further depletes the epidermis of its water-retaining constituents. 3. Climate has a major effect, and most patients experience symptoms for the first time during a winter season as their skin dries from exposure to the low indoor humidity produced as buildings are heated against inclement weather. Incidence will vary from place to place, depending on the severity of the season and the overall regional weather. CLINICAL APPLICATION QUESTIONS In the early spring, a 75-five-year-old woman visits your office with a complaint of generalized itching. The symptoms began in late December on local skin areas, and have progressed throughout the winter. You suspect an asteatotic eczema. 1. What information from her history may help support your suspicions? 2. What are the primary lesions in areas of asteatotic eczema? 3. What are the secondary lesions seen in asteatotic eczema? 4. What typical configurations strongly support your suspicions? 5. This woman has minimal physical findings, and some provoking factors are evi- dent in her history, but she fails to improve with treatment. What should be done next? APPLICATION GUIDELINES Specific History Onset Symptoms usually are noted in the fifth and sixth decades of life for the first time. -

Japanese Guidelines for Atopic Dermatitis 2020*
Allergology International 69 (2020) 356e369 Contents lists available at ScienceDirect Allergology International journal homepage: http://www.elsevier.com/locate/alit Invited Review Article Japanese guidelines for atopic dermatitis 2020* * Norito Katoh a, , 1, Yukihiro Ohya b, 1, Masanori Ikeda c, Tamotsu Ebihara d, Ichiro Katayama e, Hidehisa Saeki f, Naoki Shimojo g, Akio Tanaka h, Takeshi Nakahara i, Mizuho Nagao j, Michihiro Hide h, Yuji Fujita g, Takao Fujisawa k, Masaki Futamura l, Koji Masuda a, Hiroyuki Murota m, Kiwako Yamamoto-Hanada b, Committee for Clinical Practice Guidelines for the Management of Atopic Dermatitis 2018, The Japanese Society of Allergology, The Japanese Dermatology Association a Department of Dermatology, Kyoto Prefectural University of Medicine Graduate School of Medical Science, Kyoto, Japan b Allergy Center, National Center for Child Health and Development, Tokyo, Japan c Department of Pediatric Acute Medicine, Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences, Okayama, Japan d Department of Dermatology, Keio University School of Medicine, Tokyo, Japan e Department of Dermatology, Graduate School of Medicine, Osaka University, Suita, Japan f Department of Dermatology, Graduate School of Medicine, Nihon Medical School, Tokyo, Japan g Department of Pediatrics, Graduate School of Medicine, Chiba University, Chiba, Japan h Department of Dermatology, Hiroshima University Graduate School of Biomedical Sciences, Hiroshima, Japan i Division of Skin Surface Sensing, Department -

2U11/13U195 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date Χ n n 20 October 2011 (20.10.2011) 2U11/13U195 Al (51) International Patent Classification: ka Pharmaceutical Co., Ltd., 1-7-1, Dosho-machi, Chuo- C12P 19/34 (2006.01) C07H 21/04 (2006.01) ku, Osaka-shi, Osaka 541-0045 (JP). (21) International Application Number: (74) Agents: KELLOGG, Rosemary et al; Swanson & PCT/US201 1/032017 Bratschun, L.L.C., 8210 SouthPark Terrace, Littleton, Colorado 80120 (US). (22) International Filing Date: 12 April 201 1 (12.04.201 1) (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, English (25) Filing Language: AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (26) Publication Language: English CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (30) Priority Data: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 61/323,145 12 April 2010 (12.04.2010) US KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (71) Applicants (for all designated States except US): SOMA- ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, LOGIC, INC. [US/US]; 2945 Wilderness Place, Boulder, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, Colorado 80301 (US). OTSUKA PHARMACEUTI¬ SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, CAL CO., LTD. -

Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood
Pediatric ddermatologyermatology Series Editor: Camila K. Janniger, MD Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood Yuri T. Jadotte, MD; Camila K. Janniger, MD Pityriasis alba (PA) is a localized hypopigmented 80 years ago.2 Mainly seen in the pediatric popula- disorder of childhood with many existing clinical tion, it primarily affects the head and neck region, variants. It is more often detected in individuals with the face being the most commonly involved with a darker complexion but may occur in indi- site.1-3 Pityriasis alba is present in individuals with viduals of all skin types. Atopy, xerosis, and min- all skin types, though it is more noticeable in those with eral deficiencies are potential risk factors. Sun a darker complexion.1,3 This condition also is known exposure exacerbates the contrast between nor- as furfuraceous impetigo, erythema streptogenes, mal and lesional skin, making lesions more visible and pityriasis streptogenes.1 The term pityriasis alba and patients more likely to seek medical atten- remains accurate and appropriate given the etiologic tion. Poor cutaneous hydration appears to be a elusiveness of the disorder. common theme for most riskCUTIS factors and may help elucidate the pathogenesis of this disorder. The Epidemiology end result of this mechanism is inappropriate mel- Pityriasis alba primarily affects preadolescent children anosis manifesting as hypopigmentation. It must aged 3 to 16 years,4 with onset typically occurring be differentiated from other disorders of hypopig- between 6 and 12 years of age.5 Most patients are mentation, such as pityriasis versicolor alba, vitiligo, younger than 15 years,3 with up to 90% aged 6 to nevus depigmentosus, and nevus anemicus. -

A New Insight on Atopic Skin Diathesis: Is It Correlated with the Severity of Melasma
A New Insight on Atopic Skin Diathesis: Is It Correlated with the Severity of Melasma Danar Wicaksono1*, Rima Mustafa2, Sri Awalia Febriana1, Kristiana Etnawati1 1 Dermatovenereology Department, Faculty of Medicine Universitas Gadjah Mada – Dr. Sardjito General Hospital, Yogyakarta-Indonesia 2 Clinical Epidemiology and Biostatistics Unit, Faculty of Medicine Universitas Gadjah Mada –Dr. Sardjito General Hospital, Yogyakarta-Indonesia Keywords: Melasma, atopic skin diathesis (ASD), MASI score, atopic dermatitis (AD) Abstract: Melasma is a macular lesion of light brown to dark on the sun-exposed area, especially on the face. Atopic Skin Diathesis (ASD) is a clinical term to describe skin atopics with previous, present or future atopic dermatitis (AD). Dennie-Morgan infraorbital folds are secondary creases in the skin below the lower eyelids with a sensitivity of 78% and a specificity of 76% to diagnose AD. Melasma skin is characterized by impaired stratum corneum integrity and a delayed barrier recovery rate. Barrier dysfunction will stimulate keratinocyte to secrete keratinocyte-derived factor, which plays role in skin pigmentation process in melasma. To analyze correlation between ASD and Melasma Area Severity Index (MASI) score in melasma patient. This study is an observational analytic study with cross sectional design. Measurement of ASD and MASI score were done in 60 subjects with melasma who went to dermatology outpatient clinic Dr. Sardjito General Hospital from July 2017 to Januari 2018. The correlation between ASD and MASI score was analyzed using Pearson correlation. The result of this study showed no significant correlation between ASD and MASI scores (r: 0.02, p: 0,85). Crude Relative Risk (RR) for Dennie-Morgan infraorbital folds and MASI score was 4 (1.01-15.87). -

Turkish Guideline for Atopic Dermatitis 2018
Review DOI: 10.6003/jtad.18122r1 Turkish Guideline for Atopic Dermatitis 2018 Burhan Engin,1 MD, Emel Bülbül Başkan,2 MD, Murat Borlu,3 MD, Selda Pelin Kartal,4 MD, Başak Yalçın,5 MD, Savaş Yaylı,6 MD, Server Serdaroğlu,1 MD Address: 1İstanbul Üniversitesi-Cerrahpaşa, Cerrahpaşa Tıp Fakültesi, Deri ve Zührevi Hastalıkları Anabilim Dalı, İstanbul, 2Uludağ Üniversitesi Tıp Fakültesi, Deri ve Zührevi Hastalıkları Anabilim Dalı, Bursa, 3Erciyes Üniversitesi Tıp Fakültesi, Deri ve Zührevi Hastalıkları Anabilim Dalı, Bursa, 4Sağlık Bilimleri Üniversitesi, Ankara Dışkapı Yıldırım Beyazıt Eğitim ve Araştırma Hastanesi, Deri ve Zührevi Hastalıkları Anabilim Dalı, Ankara, 5Ankara Yıldırım Beyazıt Üniversitesi, Deri ve Zührevi Hastalıkları Anabilim Dalı, Ankara, 6Karadeniz Teknik Üniversitesi Tıp Fakültesi, Deri ve Zührevi Hastalıkları Anabilim Dalı, Trabzon, Türkiye E-mail: [email protected] Corresponding Author: Dr. Burhan Engin, İstanbul Üniversitesi-Cerrahpaşa, Cerrahpaşa Tıp Fakültesi, Deri ve Zührevi Hastalıkları Anabilim Dalı, İstanbul, Türkiye Published: J Turk Acad Dermatol 2018; 12 (2): 18122r1. This article is available from: http://www.jtad.org/2018/2/jtad18122r1.pdf Keywords: Turkish guideline, Atopik dermatit Abstract Background: Atopic dermatitis (AD) is a common inflammatory skin disease worldwide and life-long prevalence thereof can exceed 20% in developed countries. The prevalence of the disease increases gradually in developing countries and in African and Asian countries with low income. AD affects quality of life unfavorably in a significant manner. The cost of AD is quite high both due to healthcare expenses required for treatment and causing labor loss. Patients receive long-term treatments owing to the fact that it is a disease with a chronic course and there is no curative treatment which also cause medicine expenses and a number of toxicities. -

Seborrheic Dermatitis
432 Teams Dermatology Done by: Wael Al Saleh & Abdulrahman Al-Akeel Reviewer: Wael Al Saleh & Abdulrahman Al-Akeel 9 Team Leader: Basil Al Suwaine Color Code: Original, Team’s note, Important, Doctor’s note, Not important, Old teamwork 432 Dermatology Team Lecture 9: Atopic dermatitis/ Eczema Objectives 1- To know the definition & classification of Dermatitis/Eczema 2- To recognize the primary presentation of different types of eczema 3- To understand the possible pathogenesis of each type of eczema 4- To know the scheme of managements lines P a g e | 1 432 Dermatology Team Lecture 9: Atopic dermatitis/ Eczema Introduction: A groups and spectrum of related disorders with pruritus being the hallmark of the disease, they also come with dry skin. Every atopic dermatitis is eczema but not every eczema are atopic dermatitis. Atopic dermatitis mean that the patient has eczema (excoriated skin, itching and re-onset) and atopy (atopy; the patient or one of his family has allergic rhinitis, asthma or eczema). It starts early of life (eczema can happen at any time). It classified as: - Acute, characterized by erythema, papules, vesicles, oozing, and crusting. - Subacute, clinically it is represented by erythema, scaling, and crusting. - Chronic, presents with thickening of the skin, skin markings become prominent (lichenification); pigmentation and fissuring of the skin occur. Acute on top of chronic very dry 4 years old boy with chronic, itchy, well defined brownish plaque with bleeding plaques. lichenifications. Ill defined plaques Well defined erythematous excoriated Lichenification is the hallmark for plaques on both cheeks with erosion. chronic course. P a g e | 2 432 Dermatology Team Lecture 9: Atopic dermatitis/ Eczema Dermatitis Classification of dermatitis: Atopic, more common in children Seborrheic (oily skin)- (like naso-labial folds, scalp, ears) Contact dermatitis, substance cause eczema - Allergic - Irritant Nummular, coined shape, usually in the shin. -

Pathophysiology and Treatment of Pruritus in Elderly
International Journal of Molecular Sciences Review Pathophysiology and Treatment of Pruritus in Elderly Bo Young Chung † , Ji Young Um †, Jin Cheol Kim , Seok Young Kang , Chun Wook Park and Hye One Kim * Department of Dermatology, Kangnam Sacred Heart Hospital, Hallym University, Seoul KS013, Korea; [email protected] (B.Y.C.); [email protected] (J.Y.U.); [email protected] (J.C.K.); [email protected] (S.Y.K.); [email protected] (C.W.P.) * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: Pruritus is a relatively common symptom that anyone can experience at any point in their life and is more common in the elderly. Pruritus in elderly can be defined as chronic pruritus in a person over 65 years old. The pathophysiology of pruritus in elderly is still unclear, and the quality of life is reduced. Generally, itch can be clinically classified into six types: Itch caused by systemic diseases, itch caused by skin diseases, neuropathic pruritus, psychogenic pruritus, pruritus with multiple factors, and from unknown causes. Senile pruritus can be defined as a chronic pruritus of unknown origin in elderly people. Various neuronal mediators, signaling mechanisms at neuronal terminals, central and peripheral neurotransmission pathways, and neuronal sensitizations are included in the processes causing itch. A variety of therapies are used and several novel drugs are being developed to relieve itch, including systemic and topical treatments. Keywords: elderly; ion channel; itch; neurotransmission pathophysiology of itch; pruritogen; senile pruritus; treatment of itch 1. Introduction Citation: Chung, B.Y.; Um, J.Y.; Kim, Pruritus is a relatively common symptom that anyone can experience at any point in J.C.; Kang, S.Y.; Park, C.W.; Kim, H.O. -

The Art of Diagnosis
Dermatology elective for yr. 5 Natta Rajatanavin , MD. Div. of dermatology Dep. Of Medicine , Ramathibodi Hospital Mahidol University 23rd Feb 2015 How to diagnosis and manage eczema and psoriasis. Objectives • Identify and describe the morphology of eczema and psoriasis • Describe associated triggers or risk factors for eczema and psoriasis • Describe the clinical features of psoriatic arthritis • List the basic principles of treatment for eczema and psoriasis Approach dermatologic disease with an understanding of basic skin structure and microanatomy Can you name the four major layers of the epidermis? Stratum corneum Stratum granulosum (granular cell layer) Stratum spinosum (spiny layer) Stratum basale (basal cell layer) 6 Scale/scale crust Eczema/dermatitis Layers of the skin Epidermis Below the dermis lies fat, also called Dermis subcutis, panniculus, or Subcutis hypodermis. 10 Erythema nodosum Eczema/ dermatitis No.1 common skin problem Most common symptom is pruritus Eczema/dermatitis is a immunologic reaction of our skin to antigens Langerhans Cells important in the induction of delayed-type hypersensitivity 14 Classification of eczema Exogenous • Allergic • Photo allergic dermatitis • Irritant Endogenous • Skin barrier defect • sequence of histological events in eczema after contact with antigen. Eczema; acute, sub-acute stage Subacute eczema Subacute eczema histology Eczema; chronic stage Lichenfication: lichen simplex chronicus lichen simplex chronicus histology Classification of Exogenous eczema • Allergic contact dermatitis -
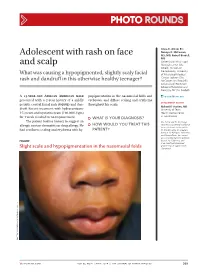
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Pattern of Skin Diseases in a Rural Village Development Community of Nepal Shrestha R1, Lama L2, Gurung D3, Shrestha DP4, Rosdahl I5
Vol. 12, No. 1, 2014 Original Article Pattern Of Skin Diseases In A Rural Village Development Community Of Nepal Shrestha R1, Lama L2, Gurung D3, Shrestha DP4, Rosdahl I5 1,2Clinical Tutor, Department of Dermatology, Abstract National Academy of Medical Sciences, Bir Introduction: Skin diseases are a common cause of morbidity in Hospital, Kathmandu, Nepal; 3Consultant Nepal as per the health services report. There is limited information Dermatologist, DI Skin Hospital and Research on the prevalence and pattern of skin diseases in the community. Center, Kathmandu, Nepal; 4Professor, Department of Dermatology & Venereology, Institute of Objectives: This study was conducted to determine the pattern of Medicine, Maharajgunj Medical Campus, skin diseases in a rural village development community of Nepal. Kathmandu, Nepal; 5Visiting Professor, Department of Dermatology, Kathmandu Medical College, Material and methods: Two dermatologic health camps were Kathmandu, Nepal. conducted, during which, the villagers were examined by dermatologists. The skin diseases diagnosed were recorded in a Address for correspondence proforma. Dr. Dwarika P Shrestha Results: There were 433 individuals examined and 359 (male-47.9%; female-52.1%) had skin disease identified clinically (camp prevalence- Department of Dermatology, IOM, 83%). The age of patients ranged from 1 to 80 years (mean-24.5; Kathmandu, Nepal SD±15.9), with majority in the age group of 10-19 years. The most Telephone: 5592217; common skin disease category was eczemas (36.4%), followed by E-mail: [email protected] infections (28.4%), acne (22%), pigment disorders (34%) and urticaria (12.3%). Citation Conclusion: Skin diseases were common in the community. The Shrestha R, Lama L, Gurung D, Shrestha DP, five most common Skin disease categories were eczemas, infections, Rosdahl I.