Discoid Lupus Erythematosus: First Clue to ……
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D. Director of Ethnic Skin Care Voluntary Assistant Professor Miller/University of Miami School of Medicine Department of Dermatology and Cutaneous Surgery What Determines Skin Color? What Determines Skin Color? No significant difference in the number of melanocytes between the races 2000 epidermal melanocytes/mm2 on head and forearm 1000 epidermal melanocytes/mm2 on the rest of the body differences present at birth Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff,K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192-220, New York, NY: McGraw Hill Melanosomes in Black and White Skin Black White Szabo G, Gerald AB, Pathak MA, Fitzpatrick TB. Nature1969;222:1081-1082 Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff, K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192- 220, New York, NY: McGraw Hill Role of Melanin-Advantages Melanin absorbs and scatters energy from UV and visible light to protect epidermal cells from UV damage Disadvantages Inflammation or injury to the skin is almost immediately accompanied by alteration in pigmentation Hyperpigmentation Hypopigmentation Dyschromias Post-Inflammatory hyperpigmentation Acne Melasma Lichen Planus Pigmentosus Progressive Macular Hypomelanosis -

Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood
Pediatric ddermatologyermatology Series Editor: Camila K. Janniger, MD Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood Yuri T. Jadotte, MD; Camila K. Janniger, MD Pityriasis alba (PA) is a localized hypopigmented 80 years ago.2 Mainly seen in the pediatric popula- disorder of childhood with many existing clinical tion, it primarily affects the head and neck region, variants. It is more often detected in individuals with the face being the most commonly involved with a darker complexion but may occur in indi- site.1-3 Pityriasis alba is present in individuals with viduals of all skin types. Atopy, xerosis, and min- all skin types, though it is more noticeable in those with eral deficiencies are potential risk factors. Sun a darker complexion.1,3 This condition also is known exposure exacerbates the contrast between nor- as furfuraceous impetigo, erythema streptogenes, mal and lesional skin, making lesions more visible and pityriasis streptogenes.1 The term pityriasis alba and patients more likely to seek medical atten- remains accurate and appropriate given the etiologic tion. Poor cutaneous hydration appears to be a elusiveness of the disorder. common theme for most riskCUTIS factors and may help elucidate the pathogenesis of this disorder. The Epidemiology end result of this mechanism is inappropriate mel- Pityriasis alba primarily affects preadolescent children anosis manifesting as hypopigmentation. It must aged 3 to 16 years,4 with onset typically occurring be differentiated from other disorders of hypopig- between 6 and 12 years of age.5 Most patients are mentation, such as pityriasis versicolor alba, vitiligo, younger than 15 years,3 with up to 90% aged 6 to nevus depigmentosus, and nevus anemicus. -

A New Insight on Atopic Skin Diathesis: Is It Correlated with the Severity of Melasma
A New Insight on Atopic Skin Diathesis: Is It Correlated with the Severity of Melasma Danar Wicaksono1*, Rima Mustafa2, Sri Awalia Febriana1, Kristiana Etnawati1 1 Dermatovenereology Department, Faculty of Medicine Universitas Gadjah Mada – Dr. Sardjito General Hospital, Yogyakarta-Indonesia 2 Clinical Epidemiology and Biostatistics Unit, Faculty of Medicine Universitas Gadjah Mada –Dr. Sardjito General Hospital, Yogyakarta-Indonesia Keywords: Melasma, atopic skin diathesis (ASD), MASI score, atopic dermatitis (AD) Abstract: Melasma is a macular lesion of light brown to dark on the sun-exposed area, especially on the face. Atopic Skin Diathesis (ASD) is a clinical term to describe skin atopics with previous, present or future atopic dermatitis (AD). Dennie-Morgan infraorbital folds are secondary creases in the skin below the lower eyelids with a sensitivity of 78% and a specificity of 76% to diagnose AD. Melasma skin is characterized by impaired stratum corneum integrity and a delayed barrier recovery rate. Barrier dysfunction will stimulate keratinocyte to secrete keratinocyte-derived factor, which plays role in skin pigmentation process in melasma. To analyze correlation between ASD and Melasma Area Severity Index (MASI) score in melasma patient. This study is an observational analytic study with cross sectional design. Measurement of ASD and MASI score were done in 60 subjects with melasma who went to dermatology outpatient clinic Dr. Sardjito General Hospital from July 2017 to Januari 2018. The correlation between ASD and MASI score was analyzed using Pearson correlation. The result of this study showed no significant correlation between ASD and MASI scores (r: 0.02, p: 0,85). Crude Relative Risk (RR) for Dennie-Morgan infraorbital folds and MASI score was 4 (1.01-15.87). -
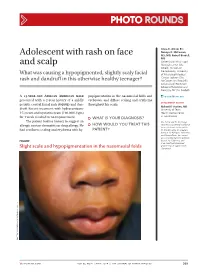
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Pattern of Skin Diseases in a Rural Village Development Community of Nepal Shrestha R1, Lama L2, Gurung D3, Shrestha DP4, Rosdahl I5
Vol. 12, No. 1, 2014 Original Article Pattern Of Skin Diseases In A Rural Village Development Community Of Nepal Shrestha R1, Lama L2, Gurung D3, Shrestha DP4, Rosdahl I5 1,2Clinical Tutor, Department of Dermatology, Abstract National Academy of Medical Sciences, Bir Introduction: Skin diseases are a common cause of morbidity in Hospital, Kathmandu, Nepal; 3Consultant Nepal as per the health services report. There is limited information Dermatologist, DI Skin Hospital and Research on the prevalence and pattern of skin diseases in the community. Center, Kathmandu, Nepal; 4Professor, Department of Dermatology & Venereology, Institute of Objectives: This study was conducted to determine the pattern of Medicine, Maharajgunj Medical Campus, skin diseases in a rural village development community of Nepal. Kathmandu, Nepal; 5Visiting Professor, Department of Dermatology, Kathmandu Medical College, Material and methods: Two dermatologic health camps were Kathmandu, Nepal. conducted, during which, the villagers were examined by dermatologists. The skin diseases diagnosed were recorded in a Address for correspondence proforma. Dr. Dwarika P Shrestha Results: There were 433 individuals examined and 359 (male-47.9%; female-52.1%) had skin disease identified clinically (camp prevalence- Department of Dermatology, IOM, 83%). The age of patients ranged from 1 to 80 years (mean-24.5; Kathmandu, Nepal SD±15.9), with majority in the age group of 10-19 years. The most Telephone: 5592217; common skin disease category was eczemas (36.4%), followed by E-mail: [email protected] infections (28.4%), acne (22%), pigment disorders (34%) and urticaria (12.3%). Citation Conclusion: Skin diseases were common in the community. The Shrestha R, Lama L, Gurung D, Shrestha DP, five most common Skin disease categories were eczemas, infections, Rosdahl I. -

A Rare Case of a Subepidermal Bullous Disorder in a Child
Pediatric dermatology Series Editor: Camila K. Janniger, MD Bullous Systemic Lupus Erythematosus With Lupus Nephritis: A Rare Case of a Subepidermal Bullous Disorder in a Child Shital Poojary, MD, FCPS, DNB; Sama Rais, MBBS Bullous systemic lupus erythematosus (BSLE) characterized by a distinct constellation of clini- is a rare subset of systemic lupus erythemato- cal, histologic, and immunologic features.1 Bullous sus (SLE) with bullous lesions in a case fulfilling the systemic lupus erythematosus is extremely rare in American Rheumatism Association (Atlanta) crite- children.2 We report a case of a 9-year-old Indian girl ria, histologically characterized by a neutrophil- with BSLE and lupus nephritis; we review the clinical predominant infiltrate in theCUTIS upper dermis with features as well as the etiopathogenesis of BSLE. immunoglobulin (IgG, IgA, IgM) and C3 deposi- tion at the basement membrane zone (BMZ). It Case Report often is associated with autoimmunity to type VII A 9-year-old girl presented with a blistering eruption collagen (NC1 [noncollagenous domain 1] over her chest, back, arms, and neck of 15 days’ dura- domain), although occasionally other antigens tion; swelling around the eyes and feet of 15 days’ such as laminin 5, laminin 6, and BP230 (bullous duration; and a low-grade fever of 2 months’ dura- pemphigoidDo antigen) have beenNot described. Bullous tion. PhysicalCopy examination revealed multiple tense systemic lupus erythematosus is extremely rare vesicles and bullae overlying urticarial plaques on in children. the neck, chest (Figure 1), back, and arms with no We report here a case of a 9-year-old girl with mucous membrane involvement. -

Views in Allergy and Immunology
CLINICAL REVIEWS IN ALLERGY AND IMMUNOLOGY Dermatology for the Allergist Dennis Kim, MD, and Richard Lockey, MD specific laboratory tests and pathognomonic skin findings do Abstract: Allergists/immunologists see patients with a variety of not exist (Table 1). skin disorders. Some, such as atopic and allergic contact dermatitis, There are 3 forms of AD: acute, subacute, and chronic. are caused by abnormal immunologic reactions, whereas others, Acute AD is characterized by intensely pruritic, erythematous such as seborrheic dermatitis or rosacea, lack an immunologic basis. papules associated with excoriations, vesiculations, and se- This review summarizes a select group of dermatologic problems rous exudates. Subacute AD is associated with erythematous, commonly encountered by an allergist/immunologist. excoriated, scaling papules. Chronic AD is associated with Key Words: dermatology, dermatitis, allergy, allergic, allergist, thickened lichenified skin and fibrotic papules. There is skin, disease considerable overlap of these 3 forms, especially with chronic (WAO Journal 2010; 3:202–215) AD, which can manifest in all 3 ways in the same patient. The relationship between AD and causative allergens is difficult to establish. However, clinical studies suggest that extrinsic factors can impact the course of disease. Therefore, in some cases, it is helpful to perform skin testing on foods INTRODUCTION that are commonly associated with food allergy (wheat, milk, llergists/immunologists see patients with a variety of skin soy, egg, peanut, tree nuts, molluscan, and crustaceous shell- Adisorders. Some, such as atopic and allergic contact fish) and aeroallergens to rule out allergic triggers that can dermatitis, are caused by abnormal immunologic reactions, sometimes exacerbate this disease. -

Treating Skin of Color NATIONALLY-RECOGNIZED DERMATOLOGIST CHARLES E CRUTCHFIELD III MD DISCUSSES SOME COMMON SKIN DISORDERS OBSERVED in SKIN of COLOR
Crutchfield-skin2 6/7/06 1:29 PM Page 34 skin treating skin of color NATIONALLY-RECOGNIZED DERMATOLOGIST CHARLES E CRUTCHFIELD III MD DISCUSSES SOME COMMON SKIN DISORDERS OBSERVED IN SKIN OF COLOR. ost skin diseases occur in people of only had black and white photographs. Additionally, all nationalities, regardless of their many lesions have been described as red, pink, salmon, skin color. Certain problems or fawn-colored. This certainly is true in Caucasian encountered in the skin are more skin; indeed many of the textbooks that were written common in people with different had this as the majority patient type. However, in tan, Mhues of skin, and sometimes a disorder seems more brown, or dark-brown skin, inflammation can look prominent because it affects skin color. grey, copper, or violaceous in color. Additionally, certain conditions will have a slightly different presentation in Variations in skin color pigmented skin (see pityriasis rosea). Skin color is determined by cells called melanocytes. Melanocytes are specialized cells within the skin that Post-inflammatory hyperpigmentation produce a pigment known as melanin. Melanin is produced and stored within special structures, known as and hypopigmentation melanosomes, contained in the melanocytes. The Melanocytes are very sensitive cells and can either stop melanocytes make up only a small percentage of overall producing color or produce excessive color in cases of skin cells. In fact, only two to three percent of all skin inflammation. Normally in children the cells stop cells are melanocytes. The variation in skin color we see producing color (I explain to parents that the cells tend across all people is determined by the type and amount to go to sleep), especially in irritation of the diaper area. -

Pediatric Psoriasis
Pediatric Papulosquamous and Eczematous Disorders St. John’s Episcopal Hospital Program Director- Dr. Suzanne Sirota-Rozenberg Dr. Brett Dolgin, DO Dr. Asma Ahmed, DO Dr. Anna Slobodskya, DO Dr. Stephanie Lasky, DO Dr. Louis Siegel, DO Dr. Evelyn Gordon, DO Dr. Vanita Chand, DO Pediatric Psoriasis Epidemiology • Psoriasis can first appear at any age, from infancy to the eighth decade of life • The prevalence of psoriasis in children ages 0 to 18 years old is 1% with an incidence of 40.8 per 100,000 ppl • ~ 75% have onset before 40 years of age What causes psoriasis? • Multifactorial • Genetics – HLA associations (Cw6, B13, B17, B57, B27, DR7) • Abnormal T cell activation – Th1, Th17 with increased cytokines IL 1, 2, 12, 17, 23, IFN-gamma, TNF-alpha • External triggers: – Injury (Koebner phenomenon) – medications (lithium, IFNs, β-blockers, antimalarials, rapid taper of systemic corticosteroids) – infections (particularly streptococcal tonsillitis). Pediatric Psoriasis Types: • Acute Guttate Psoriasis – Small erythematous plaques occurring after infection (MOST common in children) • 40% of patients with guttate psoriasis will progress to develop plaque type psoriasis • Chronic plaque Psoriasis – erythematous plaques with scaling • Flexural Psoriasis – Erythematous areas between skin folds • Scalp Psoriasis – Thick scale found on scalp • Nail Psoriasis – Nail dystrophy • Erythrodermic Psoriasis– Severe erythema covering all or most of the body • Pustular Psoriasis – Acutely arising pustules • Photosensitive Psoriasis – Seen in areas of sun -

A Rash of Information - It's Dermatology Day
INTENSIVE UPDATE AUGUST 24 - 26, 2018 & BOARD REVIEW Loews Chicago O’Hare Hotel Rosemont, IL INNOVATIVE • COMPREHENSIVE • HANDS-ON A Rash of Information - It's Dermatology Day Rob Danoff, DO, MS, FACOFP, FAAFP The American College of Osteopathic Family Physicians is accredited by the American Osteopathic Association Council to sponsor continuing medical education for osteopathic physicians. The American College of Osteopathic Family Physicians designates the lectures and workshops for Category 1-A credits on an hour-for-hour basis, pending approval by the AOA CCME, ACOFP is not responsible for the content. + A Rash of Information – It’s Dermatology Day ACOFP Intensive Review Update 8-25-18 Rob Danoff, DO, MS, FACOFP, FAAFP + Disclosure No conflicts of interest to disclose The presentation will not involve discussion of products for investigational use 1 + What’s the Diagnosis? + Pityriasis Alba Mainly affects children and adolescents – prevalence about 5% A type of eczema – unknown cause - often seen in those with dry skin and atopic dermatitis – sun exposure may trigger Most common locations are face: cheeks and chin May also be seen on neck, shoulders and upper arm Hypopigmentation more noticeable in summer, especially on darker skin tones Dry skin and scale more noticeable in dry winter weather Lesions go through stages – scaly pink plaque to hypo- pigmented plaque with fine scale to post-inflammatory macule with no scale and then eventual resolution in a few months or a few years 2 + Key Points – Pityriasis Alba Does NOT enhance -

Pityriasis Alba
PEDIATRIC DERMATOLOGY Series Editor: Camila K. Janniger, MD Pityriasis Alba Richie L. Lin, MD; Camila K. Janniger, MD Pityriasis alba (PA) is a common benign condi- Epidemiology tion in children that has no definitive treatment. PA is common, affecting between 1.9% and 5.25% Its etiology and pathogenesis are still poorly of preadolescent children.5-9 In one series of patients understood. Recent studies have found direct with PA, 81% were 15 years or younger.2 In a differ- correlations between the incidence of PA and ent retrospective analysis of cases, 90% were aged 6 atopy, amount of sun exposure, lack of sun- to 12 years, and 10% were aged 13 to 16 years.10 screen use, and frequency of bathing. It is often There is no gender predisposition.2,5-7 PA is found in an incidental finding on physical examination all parts of the world.2,4-7 One series shows a because it is usually asymptomatic. Although markedly higher incidence among school children of treatment with emollients and mild topical corti- poorer socioeconomic background.7 costeroids may accelerate the repigmentation, they have limited efficacy. Without intervention, Etiology and Pathogenesis the lesions normally resolve within months to Many terms have been used to describe PA, includ- years. Extensive PA and pigmenting PA are ing erythema streptogenes, pityriasis streptogenes, and rarer variants. impetigo furfuracea.4 However, these names imply a Cutis. 2005;76:21-24. known cause. Bacterial, fungal, and parasitic infec- tions are more frequent among individuals with PA, ityriasis alba (PA) was first recognized more but no definitive associations have been found.3,10 than 80 years ago as a localized disorder of Nutritional deficiencies also are common.2,3,10 Some P hypopigmentation that was less marked than authors have suggested that xerosis and atopy are vitiligo.1 PA mostly affects the head and neck implicated in the pathogenesis of PA.2,4,10,11 The region of children. -

The Itch That Rashes Cynthia Griffith MPAS, PA-C
The Itch That Rashes Cynthia Griffith MPAS, PA-C 1 Atopic Dermatitis Pityriasis Alba Nummular Eczema Dyshidrotic Eczema Lichen Simplex Chronicus Semantics: Eczema is a descriptive term not technically a diagnosis. The term refers to a group of inflammatory skin eruptions; atopic dermatitis, contact dermatitis, dyshidrotic eczema, ect. 3 Atopic Dermatitis Chronic, pruritic skin disease caused by barrier dysfunction, genetics, environment, impaired immune response. "The itch that rashes" Atopic Dermatitis Aggravators Stress, heat, sweating, and external irritants You should refrain from wearing wool as this can further irritate your skin. Emotional stress Extremes of weather. Infection Atopic Dermatitis Clinical presentation: Erythematous papules, that coalesce to form erythematous plaques that may display weeping, crusting, or scale over cheeks, forehead, scalp and extensor surfaces in toddlers and infants Atopic Dermatitis Clinical presentation: Lichenified, eczematous plaques in flexural areas of the neck, elbows, wrists, and ankles in older kids and adults Atopic Dermatitis Atopy Triad: Allergic rhinitis, Asthma, Atopic dermatitis Treatment: First line: long term emollients, short term topical steroids, antibiotics for secondary infection Second line: Topical calcineurin inhibitors - tacrolimus and pimecrolimus Food allergy may be a factor in kids with refractory AD Atopic Dermatitis Adult Patient care tips Hot baths, alkaline soaps, vigorous rubbing and scrubbing should be avoided. Water should be kept tepid and a mild cleanser (not antibiotic cleanser) should be used only on soiled skin. Soap should be used only on arm pits, genital region and scalp. Immediately after bathing while the skin is still moist apply a thin coat of Vaseline or Aquaphor to skin. Atopic Dermatitis Adult Patient care tips Humidifiers are helpful.