A Rare Case of a Subepidermal Bullous Disorder in a Child
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D. Director of Ethnic Skin Care Voluntary Assistant Professor Miller/University of Miami School of Medicine Department of Dermatology and Cutaneous Surgery What Determines Skin Color? What Determines Skin Color? No significant difference in the number of melanocytes between the races 2000 epidermal melanocytes/mm2 on head and forearm 1000 epidermal melanocytes/mm2 on the rest of the body differences present at birth Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff,K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192-220, New York, NY: McGraw Hill Melanosomes in Black and White Skin Black White Szabo G, Gerald AB, Pathak MA, Fitzpatrick TB. Nature1969;222:1081-1082 Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff, K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192- 220, New York, NY: McGraw Hill Role of Melanin-Advantages Melanin absorbs and scatters energy from UV and visible light to protect epidermal cells from UV damage Disadvantages Inflammation or injury to the skin is almost immediately accompanied by alteration in pigmentation Hyperpigmentation Hypopigmentation Dyschromias Post-Inflammatory hyperpigmentation Acne Melasma Lichen Planus Pigmentosus Progressive Macular Hypomelanosis -

Medicare Human Services (DHHS) Centers for Medicare & Coverage Issues Manual Medicaid Services (CMS) Transmittal 155 Date: MAY 1, 2002
Department of Health & Medicare Human Services (DHHS) Centers for Medicare & Coverage Issues Manual Medicaid Services (CMS) Transmittal 155 Date: MAY 1, 2002 CHANGE REQUEST 2149 HEADER SECTION NUMBERS PAGES TO INSERT PAGES TO DELETE Table of Contents 2 1 45-30 - 45-31 2 2 NEW/REVISED MATERIAL--EFFECTIVE DATE: October 1, 2002 IMPLEMENTATION DATE: October 1, 2002 Section 45-31, Intravenous Immune Globulin’s (IVIg) for the Treatment of Autoimmune Mucocutaneous Blistering Diseases, is added to provide limited coverage for the use of IVIg for the treatment of biopsy-proven (1) Pemphigus Vulgaris, (2) Pemphigus Foliaceus, (3) Bullous Pemphigoid, (4) Mucous Membrane Pemphigoid (a.k.a., Cicatricial Pemphigoid), and (5) Epidermolysis Bullosa Acquisita. Use J1563 to bill for IVIg for the treatment of biopsy-proven (1) Pemphigus Vulgaris, (2) Pemphigus Foliaceus, (3) Bullous Pemphigoid, (4) Mucous Membrane Pemphigoid, and (5) Epidermolysis Bullosa Acquisita. This revision to the Coverage Issues Manual is a national coverage decision (NCD). The NCDs are binding on all Medicare carriers, intermediaries, peer review organizations, health maintenance organizations, competitive medical plans, and health care prepayment plans. Under 42 CFR 422.256(b), an NCD that expands coverage is also binding on a Medicare+Choice Organization. In addition, an administrative law judge may not review an NCD. (See §1869(f)(1)(A)(i) of the Social Security Act.) These instructions should be implemented within your current operating budget. DISCLAIMER: The revision date and transmittal number only apply to the redlined material. All other material was previously published in the manual and is only being reprinted. CMS-Pub. -

Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood
Pediatric ddermatologyermatology Series Editor: Camila K. Janniger, MD Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood Yuri T. Jadotte, MD; Camila K. Janniger, MD Pityriasis alba (PA) is a localized hypopigmented 80 years ago.2 Mainly seen in the pediatric popula- disorder of childhood with many existing clinical tion, it primarily affects the head and neck region, variants. It is more often detected in individuals with the face being the most commonly involved with a darker complexion but may occur in indi- site.1-3 Pityriasis alba is present in individuals with viduals of all skin types. Atopy, xerosis, and min- all skin types, though it is more noticeable in those with eral deficiencies are potential risk factors. Sun a darker complexion.1,3 This condition also is known exposure exacerbates the contrast between nor- as furfuraceous impetigo, erythema streptogenes, mal and lesional skin, making lesions more visible and pityriasis streptogenes.1 The term pityriasis alba and patients more likely to seek medical atten- remains accurate and appropriate given the etiologic tion. Poor cutaneous hydration appears to be a elusiveness of the disorder. common theme for most riskCUTIS factors and may help elucidate the pathogenesis of this disorder. The Epidemiology end result of this mechanism is inappropriate mel- Pityriasis alba primarily affects preadolescent children anosis manifesting as hypopigmentation. It must aged 3 to 16 years,4 with onset typically occurring be differentiated from other disorders of hypopig- between 6 and 12 years of age.5 Most patients are mentation, such as pityriasis versicolor alba, vitiligo, younger than 15 years,3 with up to 90% aged 6 to nevus depigmentosus, and nevus anemicus. -

Bullous Pemphigoid/Pemphigus and Administration of the Pfizer/Biontech Vaccine (Comirnaty®). Introduction the Pfizer/Bionte
Bullous Pemphigoid/Pemphigus and administration of the Pfizer/BioNTech vaccine (Comirnaty®). Introduction The Pfizer/BioNTech vaccine (Comirnaty®) is a COVID-19-mRNA-vaccine (nucleoside modified). It is indicated for active immunisation to prevent COVID-19 caused by SARS-CoV-2 virus, in individuals 16 years of age and older. [1] The nucleoside-modified messenger RNA in Comirnaty® is formulated in lipid nanoparticles, which enable delivery of the nonreplicating RNA into host cells to direct transient expression of the SARS-CoV-2 S antigen. The mRNA codes for membrane-anchored, full-length Spike glycoprotein with two point mutations within the central helix. [1] Comirnaty® has been registered in Europe since December 21st, 2020. Bullous skin diseases are a group of dermatoses characterized by blisters and bullae in the skin and mucous membranes. The most common are pemphigus and bullous pemphigoid (BP). Pemphigus and bullous pemphigoid are autoantibody-mediated blistering skin diseases. In pemphigus, keratinocytes in epidermis and mucous membranes lose cell-cell adhesion, and in pemphigoid, the basal keratinocytes lose adhesion to the basement membrane. Bullous pemphigoid is a more common disease than pemphigus [2]. Bullous pemphigoid is the most common heterogeneous subepidermal autoimmune blistering disease (incidence 7 per million person year) [3,4], with an increasing prevalence after the age of 70, although it can also occur in the younger. It is characterized by auto-antibodies against different structural proteins of the hemidesmosomes in the epidermal basement membrane zone (EBMZ). Bullous pemphigoid typically causes severe pruritus with predominantly cutaneous lesions consisting of tense (fluid filled) bullae, erythema, and urticarial plaques. -

A New Insight on Atopic Skin Diathesis: Is It Correlated with the Severity of Melasma
A New Insight on Atopic Skin Diathesis: Is It Correlated with the Severity of Melasma Danar Wicaksono1*, Rima Mustafa2, Sri Awalia Febriana1, Kristiana Etnawati1 1 Dermatovenereology Department, Faculty of Medicine Universitas Gadjah Mada – Dr. Sardjito General Hospital, Yogyakarta-Indonesia 2 Clinical Epidemiology and Biostatistics Unit, Faculty of Medicine Universitas Gadjah Mada –Dr. Sardjito General Hospital, Yogyakarta-Indonesia Keywords: Melasma, atopic skin diathesis (ASD), MASI score, atopic dermatitis (AD) Abstract: Melasma is a macular lesion of light brown to dark on the sun-exposed area, especially on the face. Atopic Skin Diathesis (ASD) is a clinical term to describe skin atopics with previous, present or future atopic dermatitis (AD). Dennie-Morgan infraorbital folds are secondary creases in the skin below the lower eyelids with a sensitivity of 78% and a specificity of 76% to diagnose AD. Melasma skin is characterized by impaired stratum corneum integrity and a delayed barrier recovery rate. Barrier dysfunction will stimulate keratinocyte to secrete keratinocyte-derived factor, which plays role in skin pigmentation process in melasma. To analyze correlation between ASD and Melasma Area Severity Index (MASI) score in melasma patient. This study is an observational analytic study with cross sectional design. Measurement of ASD and MASI score were done in 60 subjects with melasma who went to dermatology outpatient clinic Dr. Sardjito General Hospital from July 2017 to Januari 2018. The correlation between ASD and MASI score was analyzed using Pearson correlation. The result of this study showed no significant correlation between ASD and MASI scores (r: 0.02, p: 0,85). Crude Relative Risk (RR) for Dennie-Morgan infraorbital folds and MASI score was 4 (1.01-15.87). -

Dermatitis Herpetiformis
Dermatitis herpetiformis Authors: Professors Paolo Fabbri 1 and Marzia Caproni Creation date: November 2003 Update: February 2005 Scientific editor: Professor Benvenuto Giannotti 1II Clinica Dermatologica, Dipartimento di Scienze Dermatologiche, Università degli Studi di Firenze, Via degli Alfani 37, 50121, Firenze, Italy. [email protected] Summary Keywords Disease name and synonyms Definition Prevalence Clinical manifestations Differential diagnosis Etiopathogenesis Management – treatment Diagnostic criteria – methods References Summary Dermatitis herpetiformis (DH) is a subepidermal bullous disease characterized by chronic recurrence of itchy, erythematous papules, urticarial wheals and grouped vesicles that appear symmetrically on the extensor surfaces, buttocks and back. Children and young adults are mostly affected. Prevalence is estimated to be about 10 to 39 cases/100,000/year, with incidence ranging from 0,9 (Italy) to 2,6 (Northern Ireland) new cases/100,000/year. The disease is the cutaneous expression of a gluten-sensitive enteropathy identifiable with celiac disease. The clinical and histological pictures of both entities are quite similar. Granular IgA deposits at the dermo-epidermal junction, neutrophils and eosinophils together with activated CD4+ Th2 lymphocytes are supposed to represent the main immune mechanisms that co- operate in the pathogenesis of the disease. A strict gluten withdrawal from diet represents the basis for treatment. Keywords autoimmune bullous diseases, celiac disease, tissue transglutaminase, anti-endomysium antibodies, anti- tissue transglutaminase antibodies, gluten sensitivity, dapsone. deposits at the dermal papillae represent the immunological marker of the disease, that is strictly associated with a gluten-sensitive Disease name and synonyms enteropathy (GSE), indistinguishable from celiac - Dermatitis herpetiformis (DH), disease (CD). 1 - Duhring-Brocq disease, - Duhring’s dermatitis. -

Transcription
Amethyst: Welcome, everyone! This call is now being recorded. I would like to thank you for being on the call this evening and to our Sponsors Genentech, Principia Biopharma, Argenx, and Cabaletta Bio for making today’s call possible. Today’s topic is Peer Support to answer your question about living with pemphigus and pemphigoid with the IPPF’s Peer Health Coaches. So before we begin, I want to take a quick poll to see how many of you have connected with an IPPF Peer Health Coach (either by phone or email)? While you are answering the poll let me introduce you to the IPPF Peer Health coaches: Marc Yale is the Executive Director of the IPPF and also works as a PHC. Marc was diagnosed in 2007 with Cicatricial Pemphigoid, a rare autoimmune blistering skin disease. Like others with a rare disease, he experienced delays in diagnosis and difficulty finding a knowledgeable physician. Eventually, Marc lost his vision from the disease. This inspired him to help others with the disease. In 2008, he joined the IPPF as a Peer Health Coach. Becky Strong is the Outreach Director of the International Pemphigus & Pemphigoid Foundation and also works as a PHC. She was diagnosed with pemphigus vulgaris in 2010 after a 17-month journey that included seeing six different doctors from various specialties. She continues to use this experience to shine a light on the average pemphigus and pemphigoid patient experience of delayed diagnosis and bring attention to how healthcare professionals can change the patient experience. Mei Ling Moore was diagnosed with Pemphigus Vulgaris in February of 2002. -

Oral Signs of Systemic Disease CDA 2015 Lecture Notes
2015-08-28 Oral Signs of Oral Signs of Systemic Disease Systemic Disease Why do you need to know? ! AHA! I diagnosed your systemic disease – less likely ! Helping your patients with known Karen Burgess, DDS, MSc, FRCDC systemic diseases - more likely Oral Pathology and Oral Medicine, Faculty of Dentistry, University of Toronto Department of Dentistry, Princess Margaret Hospital Department of Dentistry, Mt Sinai Hospital 2015-08-29 2015-08-29 2015-08-29 2015-08-29 2015-08-29 2015-08-29 Normal or Abnormal? Clinical description ! Type of abnormality (shape) ! The hardest part of oral pathology ! Number ! Colour ! Consistency ! Size - measure accurately ! Surface texture ! Location 2015-08-29 2015-08-29 2015-08-29 1 2015-08-28 Vocabulary Clinical description ! Ulcer ! Type of abnormality (shape) ! Vesicle/Bulla ! Number ! Macule ! Colour ! Patch ! Consistency ! Plaque ! Size - measure accurately ! Polyp- sessile or pedunculated ! Surface texture ! Location 2015-08-29 2015-08-29 2015-08-29 Description 2015-08-29 2015-08-29 2015-08-29 Differential Diagnosis Differential Diagnosis Differential Diagnosis ! Erythema multiforme ! Mucous membrane pemphigoid ! Primary herpes ! Erythema multiforme –"Any genital or eye lesions –"How long has it been present? ! Mucous membrane pemphigoid –"Any blisters? –"Any skin lesions? ! Pemphigus vulgaris ! Pemphigus vulgaris –"any skin lesions? ! Lichen planus ! Primary herpes –"Any blisters? –"How long has it been present? ! Lichen planus What information will help you narrow down –"Any other symptoms – malaise, -

Epidermolysis Bullosa Acquisita Associated with Relapsing Polychondritis: an Association with Eosinophilia? Christine A
Epidermolysis Bullosa Acquisita Associated with Relapsing Polychondritis: An Association with Eosinophilia? Christine A. Papa, DO, Danville, Pennsylvania Michele S. Maroon, MD, Danville, Pennsylvania William B. Tyler, MD, Danville, Pennsylvania Epidermolysis bullosa acquisita is a blistering dis- order that has been associated with other autoim- mune diseases. It has not previously been associ- ated with relapsing polychondritis (RPC). RPC is an autoimmune disorder that frequently displays peripheral eosinophilia. The eosinophil has been implicated in mediation of tissue damage and bul- lae formation. RPC should be added to the list of diseases seen in association with EBA. pidermolysis bullosa acquisita (EBA) is a rare, usually chronic blistering disorder that has been associated with systemic diseases in which au- E 1 toimmune pathogenesis has been implicated. It has not been described in association with relapsing polychon- dritis (RPC). Three clinical forms of EBA exist.2 The classic presentation has noninflammatory acral bullae associated with trauma that heal with scarring and milia. The bullous pemphigoid-like presentation has widespread inflammatory bullae surrounded by urticar- ial plaques involving the trunk; these heal without scar- FIGURE 1. Sharply marginated erythema and edema of ring or milia. The cicatricial pemphigoid-like presen- cartilaginous ear. tation has predominantly mucosal involvement. EBA is often refractory to treatment. ly (Figure 1) and less intensely over the cartilaginous alae. Her nonspecific eruption rapidly evolved to tense Case Report bullae on edematous, erythematous urticarial bases over A previously healthy 75-year-old white woman was a 3-day period (Figure 2). There was no mucosal hospitalized for a 3-week history of generalized weak- involvement. -
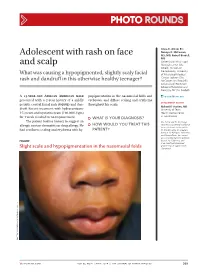
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Radiation-Induced Pemphigus Or Pemphigoid Disease in 3 Patients with Distinct Underlying Malignancies
Radiation-Induced Pemphigus or Pemphigoid Disease in 3 Patients With Distinct Underlying Malignancies Wonwoo Shon, DO; David A. Wada, MD; Amer N. Kalaaji, MD PRACTICE POINTS • The use of radiation therapy is increasing because of its therapeutic benefit, especially in advanced-stage cancer patients. • Although there is a wide range of adverse effects associated with radiation therapy, pemphigus or pemphigoid disease is rare and needs to be distinguished from other skin diseases or even recurrent underlying cancer. • The precise mechanism of radiation-induced pemphigus or pemphigoid disease is unknown, but clinicians should be alert to this potentially serious complication, and all cutaneous eruptions developing during and after radiation therapy should be evaluated with routine histologic examination in conjunction with direct immunofluorescence, serum for indirect immunofluorescence, and enzyme-linked immunosorbent assay. The cutaneous lesions of radiation-induced pem- eruption is unknown, clinicians should be alert for phigus or pemphigoid disease may resemble this potentially serious complication and evaluate other skin diseases, including recurrent underly- all cutaneous eruptions developing during and ing cancer. We performed a computerized search after radiotherapy. of Mayo Clinic (Rochester, Minnesota) archives Cutis. 2016;97:219-222. and identified 3 cases of pemphigus or pemphi- goid disease that occurredCUTIS after radiation therapy Do not copy for breast, cervical, and metastatic malignancies, number of adverse cutaneous effects may respectively. In 2 of these patients, the disease result from radiation therapy, including was initially confined to the irradiated field but A radiodermatitis, alopecia, and radiation- subsequently disseminated to other parts of the induced neoplasms. Radiation therapy rarely induces patients’ bodies, including mucosal surfaces. -

Pattern of Skin Diseases in a Rural Village Development Community of Nepal Shrestha R1, Lama L2, Gurung D3, Shrestha DP4, Rosdahl I5
Vol. 12, No. 1, 2014 Original Article Pattern Of Skin Diseases In A Rural Village Development Community Of Nepal Shrestha R1, Lama L2, Gurung D3, Shrestha DP4, Rosdahl I5 1,2Clinical Tutor, Department of Dermatology, Abstract National Academy of Medical Sciences, Bir Introduction: Skin diseases are a common cause of morbidity in Hospital, Kathmandu, Nepal; 3Consultant Nepal as per the health services report. There is limited information Dermatologist, DI Skin Hospital and Research on the prevalence and pattern of skin diseases in the community. Center, Kathmandu, Nepal; 4Professor, Department of Dermatology & Venereology, Institute of Objectives: This study was conducted to determine the pattern of Medicine, Maharajgunj Medical Campus, skin diseases in a rural village development community of Nepal. Kathmandu, Nepal; 5Visiting Professor, Department of Dermatology, Kathmandu Medical College, Material and methods: Two dermatologic health camps were Kathmandu, Nepal. conducted, during which, the villagers were examined by dermatologists. The skin diseases diagnosed were recorded in a Address for correspondence proforma. Dr. Dwarika P Shrestha Results: There were 433 individuals examined and 359 (male-47.9%; female-52.1%) had skin disease identified clinically (camp prevalence- Department of Dermatology, IOM, 83%). The age of patients ranged from 1 to 80 years (mean-24.5; Kathmandu, Nepal SD±15.9), with majority in the age group of 10-19 years. The most Telephone: 5592217; common skin disease category was eczemas (36.4%), followed by E-mail: [email protected] infections (28.4%), acne (22%), pigment disorders (34%) and urticaria (12.3%). Citation Conclusion: Skin diseases were common in the community. The Shrestha R, Lama L, Gurung D, Shrestha DP, five most common Skin disease categories were eczemas, infections, Rosdahl I.