Treating Skin of Color NATIONALLY-RECOGNIZED DERMATOLOGIST CHARLES E CRUTCHFIELD III MD DISCUSSES SOME COMMON SKIN DISORDERS OBSERVED in SKIN of COLOR
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D. Director of Ethnic Skin Care Voluntary Assistant Professor Miller/University of Miami School of Medicine Department of Dermatology and Cutaneous Surgery What Determines Skin Color? What Determines Skin Color? No significant difference in the number of melanocytes between the races 2000 epidermal melanocytes/mm2 on head and forearm 1000 epidermal melanocytes/mm2 on the rest of the body differences present at birth Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff,K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192-220, New York, NY: McGraw Hill Melanosomes in Black and White Skin Black White Szabo G, Gerald AB, Pathak MA, Fitzpatrick TB. Nature1969;222:1081-1082 Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff, K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192- 220, New York, NY: McGraw Hill Role of Melanin-Advantages Melanin absorbs and scatters energy from UV and visible light to protect epidermal cells from UV damage Disadvantages Inflammation or injury to the skin is almost immediately accompanied by alteration in pigmentation Hyperpigmentation Hypopigmentation Dyschromias Post-Inflammatory hyperpigmentation Acne Melasma Lichen Planus Pigmentosus Progressive Macular Hypomelanosis -

Clinical Management of Cutaneous Adverse Events in Patients on Chemotherapy 449
Actas Dermosifiliogr. 2019;110(6):448---459 CONSENSUS DOCUMENT Clinical Management of Cutaneous Adverse Events in Patients on Chemotherapy: A National Consensus Statement by the Spanish Academy of Dermatology and Venereology and the Spanish Society of Medical Oncologyଝ a b c d e f O. Sanmartín, C. Beato, H. Jin Suh-Oh, I. Aragón, A. Espana,˜ M. Majem, g h i,∗ j S. Segura, A. Gúrpide, R. Botella, C. Grávalos a Servicio de Dermatología, Instituto Valenciano de Oncología, Valencia, Espana˜ b Departamento de Oncología Médica, Hospital Universitario Virgen Macarena, Sevilla, Espana˜ c Servicio de Dermatología, Complejo Hospitalario Universitario de Pontevedra, Pontevedra, Espana˜ d Departamento de Oncología Médica, Complejo Hospitalario Universitario de Huelva, Huelva, Espana˜ e Servicio de Dermatología, Clínica Universitaria de Navarra, Pamplona, Espana˜ f Departamento de Oncología Médica, Hospital de la Santa Creu i Sant Pau, Barcelona, Espana˜ g Servicio de Dermatología, Hospital del Mar, Barcelona, Espana˜ h Departamento de Oncología Médica, Clínica Universitaria de Navarra, Pamplona, Espana˜ i Servicio de Dermatología, Hospital Universitario La Fe, Facultad de Medicina, Universidad de Valencia, Valencia, Espana˜ j Servicio de Oncología Médica, Hospital Universitario Doce de Octubre, Madrid, Espana˜ KEYWORDS Abstract Although the arrival of new chemotherapy drugs and combinations has brought Chemotherapy; progress in terms of cancer patient survival, they entail many adverse effects that can Photosensitivity; compromise treatment, and hence -

Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood
Pediatric ddermatologyermatology Series Editor: Camila K. Janniger, MD Pityriasis Alba Revisited: Perspectives on an Enigmatic Disorder of Childhood Yuri T. Jadotte, MD; Camila K. Janniger, MD Pityriasis alba (PA) is a localized hypopigmented 80 years ago.2 Mainly seen in the pediatric popula- disorder of childhood with many existing clinical tion, it primarily affects the head and neck region, variants. It is more often detected in individuals with the face being the most commonly involved with a darker complexion but may occur in indi- site.1-3 Pityriasis alba is present in individuals with viduals of all skin types. Atopy, xerosis, and min- all skin types, though it is more noticeable in those with eral deficiencies are potential risk factors. Sun a darker complexion.1,3 This condition also is known exposure exacerbates the contrast between nor- as furfuraceous impetigo, erythema streptogenes, mal and lesional skin, making lesions more visible and pityriasis streptogenes.1 The term pityriasis alba and patients more likely to seek medical atten- remains accurate and appropriate given the etiologic tion. Poor cutaneous hydration appears to be a elusiveness of the disorder. common theme for most riskCUTIS factors and may help elucidate the pathogenesis of this disorder. The Epidemiology end result of this mechanism is inappropriate mel- Pityriasis alba primarily affects preadolescent children anosis manifesting as hypopigmentation. It must aged 3 to 16 years,4 with onset typically occurring be differentiated from other disorders of hypopig- between 6 and 12 years of age.5 Most patients are mentation, such as pityriasis versicolor alba, vitiligo, younger than 15 years,3 with up to 90% aged 6 to nevus depigmentosus, and nevus anemicus. -

A New Insight on Atopic Skin Diathesis: Is It Correlated with the Severity of Melasma
A New Insight on Atopic Skin Diathesis: Is It Correlated with the Severity of Melasma Danar Wicaksono1*, Rima Mustafa2, Sri Awalia Febriana1, Kristiana Etnawati1 1 Dermatovenereology Department, Faculty of Medicine Universitas Gadjah Mada – Dr. Sardjito General Hospital, Yogyakarta-Indonesia 2 Clinical Epidemiology and Biostatistics Unit, Faculty of Medicine Universitas Gadjah Mada –Dr. Sardjito General Hospital, Yogyakarta-Indonesia Keywords: Melasma, atopic skin diathesis (ASD), MASI score, atopic dermatitis (AD) Abstract: Melasma is a macular lesion of light brown to dark on the sun-exposed area, especially on the face. Atopic Skin Diathesis (ASD) is a clinical term to describe skin atopics with previous, present or future atopic dermatitis (AD). Dennie-Morgan infraorbital folds are secondary creases in the skin below the lower eyelids with a sensitivity of 78% and a specificity of 76% to diagnose AD. Melasma skin is characterized by impaired stratum corneum integrity and a delayed barrier recovery rate. Barrier dysfunction will stimulate keratinocyte to secrete keratinocyte-derived factor, which plays role in skin pigmentation process in melasma. To analyze correlation between ASD and Melasma Area Severity Index (MASI) score in melasma patient. This study is an observational analytic study with cross sectional design. Measurement of ASD and MASI score were done in 60 subjects with melasma who went to dermatology outpatient clinic Dr. Sardjito General Hospital from July 2017 to Januari 2018. The correlation between ASD and MASI score was analyzed using Pearson correlation. The result of this study showed no significant correlation between ASD and MASI scores (r: 0.02, p: 0,85). Crude Relative Risk (RR) for Dennie-Morgan infraorbital folds and MASI score was 4 (1.01-15.87). -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass. -

NAIL CHANGES in RECENT and OLD LEPROSY PATIENTS José M
NAIL CHANGES IN RECENT AND OLD LEPROSY PATIENTS José M. Ramos,1 Francisco Reyes,2 Isabel Belinchón3 1. Department of Internal Medicine, Hospital General Universitario de Alicante, Alicante, Spain; Associate Professor, Department of Medicine, Miguel Hernández University, Spain; Medical-coordinator, Gambo General Rural Hospital, Ethiopia 2. Medical Director, Gambo General Rural Hospital, Ethiopia 3. Department of Dermatology, Hospital General Universitario de Alicante, Alicante, Spain; Associate Professor, Department of Medicine, Miguel Hernández University, Spain Disclosure: No potential conflict of interest. Received: 27.09.13 Accepted: 21.10.13 Citation: EMJ Dermatol. 2013;1:44-52. ABSTRACT Nails are elements of skin that can often be omitted from the dermatological assessment of leprosy. However, there are common nail conditions that require special management. This article considers nail presentations in leprosy patients. General and specific conditions will be discussed. It also considers the common nail conditions seen in leprosy patients and provides a guide to diagnosis and management. Keywords: Leprosy, nails, neuropathy, multibacillary leprosy, paucibacillary leprosy, acro-osteolysis, bone atrophy, type 2 lepra reaction, anonychia, clofazimine, dapsone. INTRODUCTION Leprosy can cause damage to the nails, generally indirectly. There are few reviews about the Leprosy is a chronic granulomatous infection affectation of the nails due to leprosy. Nails are caused by Mycobacterium leprae, known keratin-based elements of the skin structure that since ancient times and with great historical are often omitted from the dermatological connotations.1 This infection is not fatal but affects assessment of leprosy. However, there are the skin and peripheral nerves. The disease causes common nail conditions that require diagnosis cutaneous lesions, skin lesions, and neuropathy, and management. -

Hair and Nail Disorders
Hair and Nail Disorders E.J. Mayeaux, Jr., M.D., FAAFP Professor of Family Medicine Professor of Obstetrics/Gynecology Louisiana State University Health Sciences Center Shreveport, LA Hair Classification • Terminal (large) hairs – Found on the head and beard – Larger diameters and roots that extend into sub q fat LSUCourtesy Health of SciencesDr. E.J. Mayeaux, Center Jr., – M.D.USA Hair Classification • Vellus hairs are smaller in length and diameter and have less pigment • Intermediate hairs have mixed characteristics CourtesyLSU Health of E.J. Sciences Mayeaux, Jr.,Center M.D. – USA Life cycle of a hair • Hair grows at 0.35 mm/day • Cycle is typically as follows: – Anagen phase (active growth) - 3 years – Catagen (transitional) - 2-3 weeks – Telogen (preshedding or rest) about 3 Mon. • > 85% of hairs of the scalp are in Anagen – Lose 75 – 100 hairs a day • Each hair follicle’s cycle is usually asynchronous with others around it LSU Health Sciences Center – USA Alopecia Definition • Defined as partial or complete loss of hair from where it would normally grow • Can be total, diffuse, patchy, or localized Courtesy of E.J. Mayeaux, Jr., M.D. CourtesyLSU of Healththe Color Sciences Atlas of Family Center Medicine – USA Classification of Alopecia Scarring Nonscarring Neoplastic Medications Nevoid Congenital Injury such as burns Infectious Systemic illnesses Genetic (male pattern) (LE) Toxic (arsenic) Congenital Nutritional Traumatic Endocrine Immunologic PhysiologicLSU Health Sciences Center – USA General Evaluation of Hair Loss • Hx is -
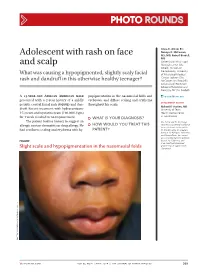
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Pattern of Skin Diseases in a Rural Village Development Community of Nepal Shrestha R1, Lama L2, Gurung D3, Shrestha DP4, Rosdahl I5
Vol. 12, No. 1, 2014 Original Article Pattern Of Skin Diseases In A Rural Village Development Community Of Nepal Shrestha R1, Lama L2, Gurung D3, Shrestha DP4, Rosdahl I5 1,2Clinical Tutor, Department of Dermatology, Abstract National Academy of Medical Sciences, Bir Introduction: Skin diseases are a common cause of morbidity in Hospital, Kathmandu, Nepal; 3Consultant Nepal as per the health services report. There is limited information Dermatologist, DI Skin Hospital and Research on the prevalence and pattern of skin diseases in the community. Center, Kathmandu, Nepal; 4Professor, Department of Dermatology & Venereology, Institute of Objectives: This study was conducted to determine the pattern of Medicine, Maharajgunj Medical Campus, skin diseases in a rural village development community of Nepal. Kathmandu, Nepal; 5Visiting Professor, Department of Dermatology, Kathmandu Medical College, Material and methods: Two dermatologic health camps were Kathmandu, Nepal. conducted, during which, the villagers were examined by dermatologists. The skin diseases diagnosed were recorded in a Address for correspondence proforma. Dr. Dwarika P Shrestha Results: There were 433 individuals examined and 359 (male-47.9%; female-52.1%) had skin disease identified clinically (camp prevalence- Department of Dermatology, IOM, 83%). The age of patients ranged from 1 to 80 years (mean-24.5; Kathmandu, Nepal SD±15.9), with majority in the age group of 10-19 years. The most Telephone: 5592217; common skin disease category was eczemas (36.4%), followed by E-mail: [email protected] infections (28.4%), acne (22%), pigment disorders (34%) and urticaria (12.3%). Citation Conclusion: Skin diseases were common in the community. The Shrestha R, Lama L, Gurung D, Shrestha DP, five most common Skin disease categories were eczemas, infections, Rosdahl I. -

Discoid Lupus Erythematosus: First Clue to ……
Discoid lupus erythematosus: First clue to ……. Sri Lanka Journal of Child Health , 2016; 45 (4): 279-280 Case Reports Discoid lupus erythematosus: First clue to autoimmune haemolytic anaemia in a child *K M D Mallesh 1, Arun Basavanahalli Chandregowda 2, Prakash Javarappa 2 Sri Lanka Journal of Child Health , 2016; 45 (4): 279-280 DOI: http://dx.doi.org/10.4038/sljch.v45i4.8185 (Key words: Discoid lupus erythematosus; autoimmune haemolytic anaemia; cutaneous lupus) Introduction Criteria for diagnosing SLE. Child was treated with Discoid lupus erythematosus (DLE) is uncommon pulsed methyl prednisone (30mg/kg) for five days in the first decade of life. It has been described as followed by prednisone 1mg/kg/day for 4 weeks part of systemic lupus erythematosus (SLE) or in tapering over next 4 weeks. Congestive heart isolation in adults1. We report a case of severe failure was managed with furosemide and enalapril. haemolytic anaemia with discoid lesions that gave Discoid lesions were treated with topical a clue to diagnosis and management. triamcinolone acetonide 0.1% cream and sun screening. Lesions responded to treatment over 4 Case report weeks (Figure B). Haemoglobin level improved A 10 year old girl presented with headache, fever, and child was asymptomatic at latest follow up. weakness and skin lesions over face for 1 month. Child had been transfused with blood earlier for severe anaemia. Examination revealed severe pallor, jaundice, hepatosplenomegaly and congestive heart failure. There were two discoid, scaly macules with irregular margins and peripheral hyperpigmentation in the left side of the face below lower eyelid (Figure A). Investigations revealed a haemoglobin level of 4.7g/dl, dimorphic anaemia, positive direct Coombs test, positive antinuclear antibodies, negative venereal disease laboratory test, negative double stranded deoxyribonucleic acid, negative anti- phospholipid antibodies and negative ribonucleoprotein. -

A Rare Case of a Subepidermal Bullous Disorder in a Child
Pediatric dermatology Series Editor: Camila K. Janniger, MD Bullous Systemic Lupus Erythematosus With Lupus Nephritis: A Rare Case of a Subepidermal Bullous Disorder in a Child Shital Poojary, MD, FCPS, DNB; Sama Rais, MBBS Bullous systemic lupus erythematosus (BSLE) characterized by a distinct constellation of clini- is a rare subset of systemic lupus erythemato- cal, histologic, and immunologic features.1 Bullous sus (SLE) with bullous lesions in a case fulfilling the systemic lupus erythematosus is extremely rare in American Rheumatism Association (Atlanta) crite- children.2 We report a case of a 9-year-old Indian girl ria, histologically characterized by a neutrophil- with BSLE and lupus nephritis; we review the clinical predominant infiltrate in theCUTIS upper dermis with features as well as the etiopathogenesis of BSLE. immunoglobulin (IgG, IgA, IgM) and C3 deposi- tion at the basement membrane zone (BMZ). It Case Report often is associated with autoimmunity to type VII A 9-year-old girl presented with a blistering eruption collagen (NC1 [noncollagenous domain 1] over her chest, back, arms, and neck of 15 days’ dura- domain), although occasionally other antigens tion; swelling around the eyes and feet of 15 days’ such as laminin 5, laminin 6, and BP230 (bullous duration; and a low-grade fever of 2 months’ dura- pemphigoidDo antigen) have beenNot described. Bullous tion. PhysicalCopy examination revealed multiple tense systemic lupus erythematosus is extremely rare vesicles and bullae overlying urticarial plaques on in children. the neck, chest (Figure 1), back, and arms with no We report here a case of a 9-year-old girl with mucous membrane involvement. -

Views in Allergy and Immunology
CLINICAL REVIEWS IN ALLERGY AND IMMUNOLOGY Dermatology for the Allergist Dennis Kim, MD, and Richard Lockey, MD specific laboratory tests and pathognomonic skin findings do Abstract: Allergists/immunologists see patients with a variety of not exist (Table 1). skin disorders. Some, such as atopic and allergic contact dermatitis, There are 3 forms of AD: acute, subacute, and chronic. are caused by abnormal immunologic reactions, whereas others, Acute AD is characterized by intensely pruritic, erythematous such as seborrheic dermatitis or rosacea, lack an immunologic basis. papules associated with excoriations, vesiculations, and se- This review summarizes a select group of dermatologic problems rous exudates. Subacute AD is associated with erythematous, commonly encountered by an allergist/immunologist. excoriated, scaling papules. Chronic AD is associated with Key Words: dermatology, dermatitis, allergy, allergic, allergist, thickened lichenified skin and fibrotic papules. There is skin, disease considerable overlap of these 3 forms, especially with chronic (WAO Journal 2010; 3:202–215) AD, which can manifest in all 3 ways in the same patient. The relationship between AD and causative allergens is difficult to establish. However, clinical studies suggest that extrinsic factors can impact the course of disease. Therefore, in some cases, it is helpful to perform skin testing on foods INTRODUCTION that are commonly associated with food allergy (wheat, milk, llergists/immunologists see patients with a variety of skin soy, egg, peanut, tree nuts, molluscan, and crustaceous shell- Adisorders. Some, such as atopic and allergic contact fish) and aeroallergens to rule out allergic triggers that can dermatitis, are caused by abnormal immunologic reactions, sometimes exacerbate this disease.