Effect of Particle Size on the Performance of an N95 Filtering Facepiece Respirator and a Surgical Mask at Various Breathing Conditions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Informing the Use of N95 Respirators by the General Public to Reduce Wildfire Smoke Exposure
Informing the use of N95 respirators by the general public to reduce wildfire smoke exposure Kaitlyn Kelly A thesis submitted in partial fulfillment of the requirements for the degree of Master of Public Health University of Washington 2020 Committee: Tania Busch Isaksen Marc Beaudreau Marissa Baker Program Authorized to Offer Degree: Environmental and Occupational Health Sciences School of Public Health 1 ©Copyright 2020 Kaitlyn Kelly 2 University of Washington Abstract Informing the use of N95 respirators by the general public to reduce wildfire smoke exposure Kaitlyn Kelly Chair of the Supervisory Committee: Tania Busch Isaksen Department of Environmental and Occupational Health Sciences Climate change is increasing the frequency, intensity, and duration of wildfires. To reduce personal exposure to wildfire smoke and resulting adverse health effects, N95 respirators are increasingly used by the general public to filter out fine particles (PM2.5) present in smoke. When mandated in an occupational setting, the use of N95 masks requires medical clearance, proper training, and fit testing. This rigorous attention to training and proper respirator fit is generally, neither required or practiced by, the lay public. A literature resource summary was conducted to understand the current state-of-knowledge around the use of N95 respirators and training in occupational and other settings to inform novel use for the general public during wildfire smoke events. The goal of this study pilot was to assess the efficacy of training materials by quantifying the transference of knowledge from selected interventions into N95 respirator fit in a convenience sample of untrained, lay public. This is the first study to assess efficacy of N95 respirator training materials for the general public during wildfire smoke events. -

EBOLA VIRUS DISEASE Essential Information for Workers
New York Committee for Occupational Safety and Health 61 Broadway Suite 1710, New York, NY 10006 email: [email protected] (212) 227-6440 fax: (212) 227-9854 website: www.nycosh.org Long Island office: NYSUT, 150 Motor Parkway, Suite 306, Hauppauge, NY 11788 (631) 435-1857 fax: (631) 231-4523 EBOLA VIRUS DISEASE Essential Information for Workers (Current as of October 27, 2014) What is Ebola? How does Ebola virus spread? Government and medical experts agree that Ebola virus is Ebola virus disease (EVD), also known as Ebola hemorrhagic spread by direct contact with an infectious SHUVRQ¶V skin, fever (EHF), is a usually fatal disease that can affect blood, or body fluids such as urine, saliva, sweat, feces, humans and some animals. It is caused by infection with the vomit, breast milk, or semen. (Body fluids may contain blood Ebola virus. The first case of Ebola in the U.S. was even if blood is not visible.) Ebola infection may occur via confirmed in September 2014. The first case of transmission liquid contact, splash contact, droplet contact, or hand of Ebola to a health care worker in the U.S. was confirmed in contact with your mouth or nose, with the mucous October 2014. membranes of the eye or eyelid, with punctures on the skin (scabs, scrapes, cuts, injections, etc.) or through sexual acts. Because the virus can survive on surfaces for several How dangerous is Ebola? days, people can also be infected by direct contact with Fifty to ninety per cent objects (like needles or bed sheets) that contain infectious of patients with Ebola blood or body fluids. -
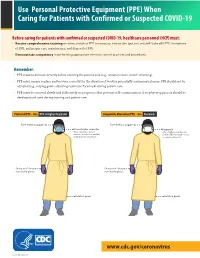
(PPE) When Caring for Patients with Confirmed Or Suspected COVID-19
Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19 Before caring for patients with confirmed or suspected COVID-19, healthcare personnel (HCP) must: • Receive comprehensive training on when and what PPE is necessary, how to don (put on) and doff (take off) PPE, limitations of PPE, and proper care, maintenance, and disposal of PPE. • Demonstrate competency in performing appropriate infection control practices and procedures. Remember: • PPE must be donned correctly before entering the patient area (e.g., isolation room, unit if cohorting). • PPE must remain in place and be worn correctly for the duration of work in potentially contaminated areas. PPE should not be adjusted (e.g., retying gown, adjusting respirator/facemask) during patient care. • PPE must be removed slowly and deliberately in a sequence that prevents self-contamination. A step-by-step process should be COVID-19developed and Personal used during Protective training and patientEquipment care. COVID-19 Personal Protective Equipment (PPE) for Healthcare Personnel (PPE) for Healthcare Personnel Preferred PPE – Use N95 or Higher Respirator Acceptable Alternative PPE – Use Facemask Face shield or goggles Face shield or goggles N95 or higher respirator Facemask When respirators are not N95 or higher respirators are available, use the best available preferred but facemasks are an alternative, like a facemask. acceptable alternative. One pair of clean, One pair of clean, non-sterile gloves non-sterile gloves Isolation gown Isolation gown cdc.gov/COVID19 cdc.gov/COVID19 CS 315838-A 03/20/2020 CS 315838-B 03/20/2020 www.cdc.gov/coronavirus CS 316124-A 06/03/2020 Donning (putting on the gear): More than one donning method may be acceptable. -

GUIDE to INFECTION CONTROL in the HOSPITAL Ebola Virus Disease
GUIDE TO INFECTION CONTROL IN THE HOSPITAL CHAPTER 61: Ebola Virus Disease Author S. Mehtar, MBBS, FRCPath, FCPath, MD Chapter Editor Gonzalo Bearman MD, MPH, FACP, FSHEA, FIDSA Topic Outline Key Issues Known Facts Suggested Practice General Principles Personal Protective Equipment for Healthcare Worker Personal Protective Equipment for Trained Observer Donning and Doffing Disinfection Healthcare Waste Management Suggested Practice in Under-Resourced Settings Summary Helpful Resources References Chapter last updated: February, 2018 KEY ISSUE The 2014 Ebola epidemic was the largest in history with 28,616 cases and 11,310 deaths recorded up to September 2016. There was widespread person-to-person transmission in multiple countries in West Africa, particularly affecting Guinea, Liberia, and Sierra Leone, but also Nigeria. Several countries in Europe and the United States received patients and healthcare workers who became infected with Ebola and were transported home for care. KNOWN FACTS • Ebola virus disease, previously known as Ebola hemorrhagic fever, is an uncommon and deadly disease caused by infection with a virus of the family Filoviridae, genus Ebolavirus. There are four identified Ebola virus species (Zaire, Sudan, Bundibugyo, and Tai Forest Ebola viruses) that cause disease in humans, Zaire being the most common and virulent and responsible for most of the outbreaks. • Ebola viruses are found in several West African countries. The first Ebola virus was discovered in 1976 near the Ebola River in what is now the Democratic Republic of the Congo. A second outbreak in Sudan occurred simultaneously. Since then, over 20 outbreaks have appeared sporadically in Africa but most of them were confined in rural forested areas. -

Tight-Fitting N95 Respirator Mask Training 8-12-20
Tight-fitting N95 Respirator Mask Training N95 Tight-fitting Respirator Mask Use Use during direct care activities that pose risk of exposure to airborne illness Use during Aerosol Generating Procedure (AGP) for coronavirus (COVID-19) positive, presumed-positive, and Person(s) Under investigation (PUI) Use during direct care of individual(s) coronavirus (COVID-19) positive, presumed-positive, and Person(s) Under investigation (PUI) when supply is plenty Employer Responsibilities Institute a respiratory protection plan that is readily available. Provide employees with medical evaluation and fit testing for N95 respirator masks Provide NIOSH and/or FDA approved N95 respirator mask as personal protective equipment (PPE) for employees involved in direct care that N95 may be needed Implement CDC and DDS guidance for optimizing PPE Provide training on use of N95 respirator mask use to employees Employee Responsibilities Participate in fit testing Remove facial hair prior to fit testing Obtain Medical evaluation (May be done at time of fit test my medical provider Understand N95 use Perform user seal check after donning N95 respirator mask Seek answers to any questions related to N95 use N95- Medical Evaluation Questionnaire filled out by a licensed healthcare provider giving clearance for the employee to wear an N95 respirator mask This must be completed prior to N95 fit testing If not approved for N95 mask use, report to management and Human Resources CDC FAQ regarding Medical Evaluation- https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/resps ource3medical.html#medicala Fit testing All N95 respirator mask wearers require fit testing for initial use of N95 respirator. -

Personal Protective Equipment for Use in a Filovirus Disease Outbreak
Personal protective equipment for use in a filovirus disease outbreak Rapid advice guideline Personal protective equipment for use in a filovirus disease outbreak Rapid advice guideline WHO Library Cataloguing-in-Publication Data Personal protective equipment for use in a filovirus disease outbreak: Rapid advice guideline. I.World Health Organization. ISBN 978 92 4 154972 1 Subject headings are available from WHO institutional repository © World Health Organization 2016 All rights reserved. Publications of the World Health Organization are available on the WHO website (http://www. who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (http://www.who.int/about/licensing/ copyright_form/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Fiber Integrity, Filtration Efficiency, and Dipole Charge Density
medRxiv preprint doi: https://doi.org/10.1101/2020.07.07.20148551; this version posted July 9, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. Assessment of N95 and K95 respirator decontamination: fiber integrity, filtration efficiency, and dipole charge density. Wonjun Yim1, Diyi Cheng1, Shiv Patel3, Rui Kui4, Ying Shirley Meng1,2, and Jesse V. Jokerst1,2,5* 1Department of Material Science and Engineering, 2Department of Nanoengineering, 3School of Medicine Simulation Training Center, 4Department of Structural Engineering, 5Department of Radiology, University of California San Diego, 9500 Gilman Drive, La Jolla, CA 92093, Unites States Abstract Personal protective equipment (PPE) including N95 respirators are critical for persons exposed to SARS-CoV-2. KN95 respirators and N95 decontamination protocols have been described as solutions to a lack of such PPE. However, there are a few materials science studies that characterize the charge distribution and physical changes accompanying disinfection treatments particularly heating. Here, we report the filtration efficiency, dipole charge density, and fiber integrity of pristine N95 and KN95 respirators before and after various decontamination methods. We found that the filter layer of N95 is 8-fold thicker than that of KN95, which explains its 10% higher filtration efficiency (97.03 %) versus KN95 (87.76 %) under pristines condition. After 60 minutes of 70 °C treatment, the filtration efficiency and dipole charge density of N95 became 97.16% and 12.48 μC/m2, while those of KN95 were 83.64% and 1.48 μC/m2; moreover, fit factor of N95 was 55 and that of KN95 was 2.7. -

How to Use Personal Protective Equipment: a Quick Reference Guide for Frontline Clinical Providers
How to Use Personal Protective Equipment: A Quick Reference Guide for Frontline Clinical Providers Frontline clinical providers should wear the following personal protective equipment (PPE) when treating individuals confirmed or suspected to be infected with COVID-19. N95 RESPIRATOR GOWN GLOVES FACE SHIELD/ EYE PROTECTION How to properly use protective equipment PPE TYPE DONNING PPE REMOVING PPE • Secure ties or elastic band at middle of • Front of respirator is contaminated – N95 RESPIRATOR head and neck DO NOT TOUCH! • Fit flexible band to nose bridge • Grasp ONLY bottom then top ties/elastics (AS AVAILABLE) • Fit snug to face and below chin and remove • Fit-check respirator • Discard in waste container • Gown front and sleeves are contaminated! • Unfasten neck, then waist ties • Remove gown using a peeling motion; • Fully cover torso from neck to knees, arms pull gown from each shoulder toward the GOWN to end of wrist, and wrap around the back same hand • Fasten in back at neck and waist • Gown will turn inside out • Hold removed gown away from body, roll into a bundle and discard into waste or linen receptacle • Outside of gloves are contaminated! • Grasp outside of glove with opposite • U se non-sterile for isolation gloved hand; peel off GLOVES Select according to hand size • • Hold removed glove in gloved hand • Extend to cover wrist of isolation gown • Slide fingers of ungloved hand under remaining glove at wrist • Outside of goggles or face shield are contaminated! FACE SHIELD / • Put on face and adjust to fit • To remove, handle by “clean” head band EYE PROTECTION or ear pieces • Place in designated receptacle for reprocessing or in waste container Wash hands or use an alcohol-based hand sanitizer immediately after removing all PPE! N95 Respirator Usage and Care N95 respirators must only be used by a single wearer. -

Information on Ebola October 17, 2014
Information on Ebola October 17, 2014 This letter is for informational purposes only. The description of medical and other health-related subjects is no substitute for professional medical advice. Although the authors of this letter have taken great care to ensure that the information corresponds to the current state of knowledge at the time of first publication, this does not release the reader from the responsibility to make his/her own, informed decisions after consultation with trained medical personnel. The products discussed below are solely intended for use by qualified professionals. This informational letter contains basic information on Ebola and links to additional references. Please keep yourself up-to-date on the current situation by reading the web pages listed in this document. Current information on the Ebola virus as well as behavioral recommendations can be found on the following websites: United States Centers for Disease Control and Prevention (CDC) http://www.cdc.gov/vhf/Ebola/about.html World Health Organization (WHO): http://www.who.int/mediacentre/factsheets/fs103/en/ European Centre for Disease Prevention and Control: http://www.ecdc.europa.eu/en/healthtopics/Ebola_marburg_fevers/information- travellers/Pages/information- travellers.aspx Robert Koch Institute (RKI): http://www.rki.de/DE/Content/InfAZ/E/Ebola/Uebersicht.html#doc5045280bodyText3 National Institute for Occupational Safety and Health (NIOSH): http://www.cdc.gov/niosh/ The following information about Ebola is based on the information provided by the above-mentioned institutions. What is Ebola? Ebola is a rare, often fatal virus originating in tropical Africa and associated with symptoms of hemorrhagic fever. This means both internal and external bleeding (hemorrhages) of the body. -
N95 Respirators and Respiratory Protection Program
N95 Respirators and Respiratory Protection Program Residential Care Facilities General Information Like other personal protective equipment (PPE), the selection of a respirator type must take into consideration the nature of the exposure and risk involved. The Michigan Occupational Safety and Health Administration (MIOSHA) requires that employers ensure employees have been trained on when PPE is necessary, what PPE is necessary, how to don/doff/adjust and wear PPE, the limitations of the PPE, and the proper care/maintenance/useful life and disposal of the PPE.1 It is important to refer to the manufacturer’s instructions for information specific to the respirator being used by an employee(s). A copy of the instructions may be added to a procedure and/or training materials to document information specific to the respirator(s) used at your facility. Ensure the respirator is FDA approved. Respirator Trusted-Source Information, CDC/NIOSH, provides a list of approved filtering facepiece respirators and counterfeit respirators. KN95 respirators are not approved by the FDA; the N95 respirator is the current required PPE for healthcare personnel (HCP) caring for suspected or positive COVID-19 patients. The following is general information regarding N95 respirators. Follow the instructions that are provided with the respirator. Manufacturer instructions (including seal checks) for many NIOSH approved disposable respirators are located at: NIOSH-Approved Particulate Filtering Facepiece Respirators, CDC/NIOSH. What is an N95 respirator? The N95 filtering facepiece respirator (FFR) is a type of respirator which removes particles from the air that are breathed through it. These respirators filter out at least 95% of very small (0.3 micron) particles. -
COVID-19 Airway Protection PPE Overview DOCUMENT INTENDED to PROVIDE INSIGHT BASED on CURRENTLY AVAILABLE INFORMATION for CONSIDERATION and NOT SPECIFIC ADVICE
COVID-19 airway protection PPE overview DOCUMENT INTENDED TO PROVIDE INSIGHT BASED ON CURRENTLY AVAILABLE INFORMATION FOR CONSIDERATION AND NOT SPECIFIC ADVICE Update: May 6, 2020 CONFIDENTIAL AND PROPRIETARY Any use of this material without specific permission of McKinsey & Company is strictly prohibited Current as of May 4, 2020 COVID-19 is, first and foremost, Solving the humanitarian a humanitarian challenge. challenge is the top priority. Thousands of health professionals Much remains to be done globally are heroically battling the virus, to prepare, respond, and recover, putting their own lives at risk. from protecting populations at risk Governments and industry are to supporting affected patients, working together to understand families, and communities to and address the challenge, support developing a vaccine. To address victims and their families and this crisis, responses must be communities, and search for informed by evidence and based treatments and a vaccine. on partnership among various stakeholders and sectors, including the medical-product industry and regulatory/compliance agencies. DOCUMENT INTENDED TO PROVIDE INSIGHT BASED ON CURRENTLY AVAILABLE INFORMATION FOR CONSIDERATION AND NOT SPECIFIC ADVICE McKinsey & Company 2 Current as of May 4, 2020 These materials are preliminary and non- The insights and concepts included in Particularly in light of rapidly evolving exhaustive and are being made available these materials have not been validated or conditions, these materials are provided on a non-exclusive basis solely for independently verified. References to “as is” without any representation or information purposes in response to the specific products or organizations are warranty, and all liability is expressly urgent need for measures to address the solely for illustration and do not constitute disclaimed for any loss or damage of any COVID-19 crisis. -

Fact Sheet for Healthcare Personnel
FACT SHEET FOR HEALTHCARE PERSONNEL Coronavirus Disease 2019 Battelle Decontamination System for Decontaminating Compatible N95 Respirators January 21, 2021 (COVID-19) You have been given a decontaminated N95 What do I need to know about the emergency use of respirator that has been decontaminated using a the Battelle Decontamination System and decontamination system that is authorized to decontaminated N95 respirators? decontaminate compatible N95 respirators for multiple- user reuse by healthcare personnel (HCP) in a • The Battelle Decontamination System has been healthcare setting (i.e., HCP may receive a different authorized for emergency use to decontaminate respirator following decontamination than the one they compatible N95 respirators for multiple-user reuse had previously used) to help prevent HCP exposure to by HCP during the COVID-19 pandemic to prevent pathogenic biologic airborne particulates during the wearer exposure to pathogenic biological airborne COVID-19 pandemic. particulates, including SARS-CoV-2. o Compatible N95 respirators are either This Fact Sheet informs you of the significant known and authorized NIOSH-approved filtering facepiece potential risks and benefits of the emergency use of respirators (FFRs) or respirators that are decontaminated, compatible N95 respirators. These authorized and listed in Exhibit 1 to FDA’s compatible N95 respirators have been decontaminated emergency use authorization (EUA) for non- using the Battelle CCDS Critical Care Decontamination NIOSH-approved imported FFRs that are not System™ (hereafter referred to as “decontaminated manufactured in China, and that do not have N95 respirators” and “Battelle Decontamination exhalation valves or a duck-billed design, and do System" throughout this Fact Sheet). not contain cellulose-based materials or antimicrobial agents.