Personal Protective Equipment for Use in a Filovirus Disease Outbreak
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Year Ends with Even More Turmoil COVER STORY Protests for Racial Justice Spin out of Control, Rocking the Revere Community and the World
Paul Revere Charter Middle School and Magnet Center Friday, June 5, 2020 Volume 64, Issue 4 Year Ends With Even More Turmoil COVER STORY Protests for racial justice spin out of control, rocking the Revere community and the world. By NICO TROEDSSON On May 25, 2020, George Floyd, a 46-year-old African American man, died in Minne- apolis, Minnesota after a white officer knelt on George Floyd’s neck for over eight minutes, kill- ing him. Cellphone footage of this incident went viral, sparking protests across the U.S. where people came together in the hopes of ending police brutali- ty and the racial inequality that has infected some members of the police force. Some of these peaceful protests devolved into The National Guard protects the Seventh grader Anna Song studies on Zoom. Photo: Mary Shannon anarchy, as looters attacked Palisades Village. Photo: Arik Kraft small local businesses as well as big corporate shops, started fires, via Schoology to notify students and destroyed many neighbor- of the change: “Based on the Revere Perseveres hoods. current social issues affecting Faced with the school’s sudden closure, The civil unrest in Los An- the Westside of Los Angeles, we geles county has affected many will be canceling the Textbook/ Patriots make the switch to remote learning. Paul Revere students on many iPad collection, Locker clean out levels. Due to the chaos and vi- for the week of June 1st. We will By ARIK KRAFT olence in the streets, the school send you out the new schedule No one really knew on Friday the 13th of March that when has had to rethink end of the year tomorrow for collection. -

Disposable Hazmat Suit 29Th April LR
HYPASHIELD H z 5k Disposable Hazmat Suit y of Textile istr s in M SITRA MADE IN COVID 19 n CERTIFIEDo i INDIA t S a BARRIER o i u c t o h ss In A d h ia rc Textile Resea Product Brochure WILDCRAFT INDIA PVT. LTD. | HYPA SHIELD W95 - Guidebook for content creators and social feeds ENGINEERED FOR OUTDOORS An Enterprise Born out of Passion Incorporated in 1998, Wildcraft India Pvt. Ltd. (WIPL) is India’s foremost company in the manufacturing and distribution of head-to-toe products for trek-to-travel solutions, serving more than 3.5 million customers annually with sales in excess of USD I00 Million. Performance-led Quality Products Be it outdoor-friendly clothing, ergonomically designed gear, all-terrain footwear or all-purpose travelcase; Wildcraft has one mission – to engineer versatile, multi-functional, lightweight, weather-resilient products for the savvy backpacker in you. End-to-End Value Chain Management Wildcraft has a strong R&D team led by domain experts and a global network of vendors. Wildcraft employs 2500 stas across 2,00,000+ sq. ft. manufacturing facilities in North & South India with a capacity to produce 10 mn+ pieces per annum. Multi-Channel Distribution Wildcraft is equipped with an extended geo footprint of 200+ exclusive brand stores across 60+ cities with 5000+ retail points-of-sale across India. This also includes over 1000 points-of-sale across departmental stores & hypermarkets. Wildcraft also has a strategic partnership with Flipkart & Myntra. Serving the Nation Wildcraft salutes the 4th frontier of our country’s defence – the Medical fraternity. -

Sacanu Enterprises
+91-8048372628 Sacanu Enterprises https://www.indiamart.com/sacanuenterprises/ We “Sacanu Enterprises” are a Sole Proprietorship firm, engaged as the foremost Manufacturer of Hazmat Suit, PPE Wear, PVC Apron, etc About Us Established in the year 1999 at Taloja, Navi Mumbai, Thane, Maharashtra, we “Sacanu Enterprises” are a Sole Proprietorship firm, engaged as the foremost Manufacturer of Hazmat Suit, PPE Wear,Chemical Suit, Protective Clothing ,PVC Apron, etc. Our products are high in demand due to their premium quality and affordable prices. Furthermore, we ensure to timely deliver these products to our clients, through this we have gained a huge clients base in the Protective Equipment market. We wold like to introduce our self leading manufacturer of Personal Protective Equipment. We also partnered with PPS UK to get their entire product line to India exclusively. For over 30 years, the Sacanu`s product offering has evolved within the industry for its bespoke and quality designs. With three decades of protecting workers in hazardous environments our reputation for reliability and expertise makes us an leading industry specialist .Our customers rely on our innovative personal protective products whilst collaborating with industries, organisations and Governments we guarantee to supply the latest, technologically advanced products offering the highest level of protection. Continual improvement, global awareness and technological development means that we will always protect your staff, your clients and our environment About PPS... For -

Design of Seamless Knitted Radiation Shielding Garments with 3D Body Scanning Technology
Available online at www.sciencedirect.com ScienceDirect Procedia Technology 20 ( 2015 ) 123 – 132 The International Design Technology Conference, DesTech2015, 29th of June – 1st of July 2015, Geelong, Australia Design of Seamless Knitted Radiation Shielding Garments with 3D Body Scanning Technology Huda Ahmed Maghrabia,c, Arun Vijayana, Lijing Wanga*, Pradip Debb aSchool of Fashion & Textiles, RMIT University, Brunswick, Victoria 3056, Australia bSchool of Medical Sciences, RMIT University, Bundoora, Victoria 3083, Australia cDepartment of Textiles and Clothing, Umm Al-Qura University, Mecca 24382, Saudi Arabia Abstract Protective aprons for medical use shield against the effects of radiation. The aprons are universally tailored to fit both male and female bodies without due consideration to the differences that abound between masculine and feminine bodies. To date very little emphasis has been shown on the development of aprons to suit the needs of the female anatomy specifically the breast region as well as consideration of the body shape of pregnant women. This research reviews the needs to develop an X-ray protective garment that is specifically tailored for the female body. Protective aprons designed to fit the female physique incorporating curvature around specific parts of the body namely hip and breast regions as well as the suitability of the apron for use by pregnant women have been explored. Emphasis has been shown on the fit of the garment to impart improved wearer mobility. 3D body scanning technology was used to determine the fit of the developed designs and understand the significance of air gaps between the body and the garment. © 2015 The Authors. PublishedPublished by by Elsevier Elsevier Ltd. -
Wild: I'm to City, Residents N
VNS Device helps Kids get a kick out of reduce depression Ignition soccer camp SPORTS - Bl 75 cents WINNERS OF STATE AND NATIONAL AWARDS OF EXCELLENCE www.hometownlife .com BY SUE MASON lowing the raid. "But they were fed," he said. "All of the dogs "There are no signs of life-threatening inju STAFF WRITER "It's one of the worst cases I've seen, I don't were really nice, a couple were afraid of us." ries, and that's a good sign," Baron said. "So far know how they lived in there," said Dodson. , According to Dodson, the dogs — 15 it looks like they're in pretty good shape." Westland building officials are determining According to Westland Police Lt. Daniel Chihuahua, a pug-beagle mix, a Shar-pei and an The case is still under investigation. The what can done with a home in the 33000 block Karrick, Animal Control became aware of the English setter ~~ were never let outside. Animal women could face charges of animal cruelty, of Fernwood where two women had housed home after receiving information from another feces was throughout the house on floors, beds based on the condition of the home, as well has 18 dogs until the animals were removed from city department. The officer was denied admit and furniture. having too many unlicensed pets, Karrick said. the premises Thursday afternoon by Westland tance by the two women on Wednesday, so "Obviously, this has been going on for a long The city limits residents to a maximum of three police and animal control officers. -

North American Buyers Guide 2013
NORTH AMERICAN BUYERS GUIDE 2013 www.whitesdiving.com www.whitesdiving.com CONTENTS HAZMAT PS DRYSUIT WHAT ARE POlyTEX SEALS? ____________________________________ 19 (PUBLIC SAFETY HAZMAT DIVER) ________________________________ 3 MK0 UNDERGARMENT ___________________________________________ 20 HAZMAT COM DRYSUIT MK1 UNDERGARMENT ___________________________________________ 21 (COMMERCIAL HAZMAT DIVER) __________________________________ 4 MK2 ONE PIECE UNDERGARMENT ______________________________ 22 PRO COM DRYSUIT (GENERAL PURPOSE COMMERCIAL DIVER) ______________________ 5 MK2 JACKET UNDERGARMENT _________________________________ 23 ENVIRO DRYSUIT _________________________________________________ 6 THERMAL FUSION UNDERGARMENT ____________________________ 24 ENVIRO HYBRID DRYSUIT ________________________________________ 7 HOODS - NEOPRENE _____________________________________________ 25 FUSION S.A.R. DRYSUIT HOODS - POLYTEX & CAPS ______________________________________ 26 (DIVE OR SURFACE/SWIMMER) ___________________________________ 8 GLOVES - NEOPRENE ____________________________________________ 27 FUSION L.E.* DRYSUIT (DIVE OR SURFACE/SWIMMER) ___________________________________ 9 GLOVES - COMMERCIAL _________________________________________ 28 KODIAK 360 S.A.R. DRYSUIT ____________________________________ 10 GLOVES & LINERS _______________________________________________ 29 KODIAK 360 L.E.* ________________________________________________ 11 GLOVES - RING SYSTEMS ________________________________________ 30 MOSS* S.A.R. DRYSUIT FOOTWEAR -

Development of Level D Hazmat Shirt Designs for Covid-19 Pandemic Medical Personnel
Proceedings of the International Joint Conference on Science, Technology, Art and Humanities (IJCSTAH 2020) Development of Level D Hazmat Shirt Designs for Covid-19 Pandemic Medical Personnel Inty Nahari 1*, Deny Arifiana 2, Sri Dwiyanti 3, Irma Russanti 4, Mein Kharnolis5 1,2,3,4,5 Department of Home Economics Universitas Negeri Surabaya Surabaya, Indonesia E-mail: *[email protected] ABSTRACT The presence of COVID-19 uncertain of impact on learning activities, including the State Vocational School in Indonesia, to prevent the spread-impact of COVID-19, and learning remains effective one of them is doing distance learning. The problem is that not all teachers can do learning online, including applying m-learning. This study aims to analyze the differences and increase the: 1) ability of teachers to prepare and organize materials-media learning to m-learning, 2) ability of teachers to utilize m-learning for learning, 3) ability of teachers to implement m-learning, after the teacher participated in the training and implementation of m- learning. The research method uses a quantitative approach to the method of quasi-experimental. The sample of 40 High School Vocational Teachers 7 in Surabaya, the determination using the technique of stratified random sampling. The technique of data analysis using t-test and test gain. The results of the research shows there is: 1) A difference and increase significantly the ability of teachers to develop and organize teaching materials-media to m-learning, from the average of 45.00 to be 78.50; 2) A difference and increase significant in the ability of teachers to use m-learning to learning, from 40 to 75.50; 3) A difference significantly and increase in the ability of teachers to implement m-learning, from the average of 35.60 to 72.10. -
Spacesuits Have Been Created, but We Want to Go Further
Science and Innovation A Boeing/Teaching Channel Partnership EXTREME BIOSUITS Student Handbook Science and Innovation Extreme Biosuits Student Handbook Engineering Design Process Step 1 Identify the Need or Problem Describe the engineering design challenge to be solved. Include the limits and constraints, customer description, and an explanation of why solving this challenge is important. Step 2 Research Criteria and Constraints Research how others have solved this or similar problems, and discover what materials have been used. Be sure to thoroughly research the limitations and design requirements for success. Step 3 Brainstorm Possible Solutions Use your knowledge and creativity to generate as many solutions as possible. During this brainstorming stage, do not reject any ideas. Step 4 Select the Best Solution Each team member presents their solution ideas to the team. Team members annotate how each solution does or does not meet each design requirement. The team then agrees on a solution, or combination of solutions, that best meets the design requirements. Step 5 Construct a Prototype Develop an operating version of the solution. Step 6 Test Test your solution. Annotate the results from each test to share with your team. Step 7 Present Results Present the results from each test to the team. Step 8 Redesign Determine a redesign to address failure points and/or design improvements. The design process involves multiple iterations and redesigns. Redesign is based on the data from your tests, your team discussions as to the next steps to improve the design, and the engineering design process Steps 1 through 7. Once your team is confident of a prototype solution, you present the results to the client. -

Informing the Use of N95 Respirators by the General Public to Reduce Wildfire Smoke Exposure
Informing the use of N95 respirators by the general public to reduce wildfire smoke exposure Kaitlyn Kelly A thesis submitted in partial fulfillment of the requirements for the degree of Master of Public Health University of Washington 2020 Committee: Tania Busch Isaksen Marc Beaudreau Marissa Baker Program Authorized to Offer Degree: Environmental and Occupational Health Sciences School of Public Health 1 ©Copyright 2020 Kaitlyn Kelly 2 University of Washington Abstract Informing the use of N95 respirators by the general public to reduce wildfire smoke exposure Kaitlyn Kelly Chair of the Supervisory Committee: Tania Busch Isaksen Department of Environmental and Occupational Health Sciences Climate change is increasing the frequency, intensity, and duration of wildfires. To reduce personal exposure to wildfire smoke and resulting adverse health effects, N95 respirators are increasingly used by the general public to filter out fine particles (PM2.5) present in smoke. When mandated in an occupational setting, the use of N95 masks requires medical clearance, proper training, and fit testing. This rigorous attention to training and proper respirator fit is generally, neither required or practiced by, the lay public. A literature resource summary was conducted to understand the current state-of-knowledge around the use of N95 respirators and training in occupational and other settings to inform novel use for the general public during wildfire smoke events. The goal of this study pilot was to assess the efficacy of training materials by quantifying the transference of knowledge from selected interventions into N95 respirator fit in a convenience sample of untrained, lay public. This is the first study to assess efficacy of N95 respirator training materials for the general public during wildfire smoke events. -

EBOLA VIRUS DISEASE Essential Information for Workers
New York Committee for Occupational Safety and Health 61 Broadway Suite 1710, New York, NY 10006 email: [email protected] (212) 227-6440 fax: (212) 227-9854 website: www.nycosh.org Long Island office: NYSUT, 150 Motor Parkway, Suite 306, Hauppauge, NY 11788 (631) 435-1857 fax: (631) 231-4523 EBOLA VIRUS DISEASE Essential Information for Workers (Current as of October 27, 2014) What is Ebola? How does Ebola virus spread? Government and medical experts agree that Ebola virus is Ebola virus disease (EVD), also known as Ebola hemorrhagic spread by direct contact with an infectious SHUVRQ¶V skin, fever (EHF), is a usually fatal disease that can affect blood, or body fluids such as urine, saliva, sweat, feces, humans and some animals. It is caused by infection with the vomit, breast milk, or semen. (Body fluids may contain blood Ebola virus. The first case of Ebola in the U.S. was even if blood is not visible.) Ebola infection may occur via confirmed in September 2014. The first case of transmission liquid contact, splash contact, droplet contact, or hand of Ebola to a health care worker in the U.S. was confirmed in contact with your mouth or nose, with the mucous October 2014. membranes of the eye or eyelid, with punctures on the skin (scabs, scrapes, cuts, injections, etc.) or through sexual acts. Because the virus can survive on surfaces for several How dangerous is Ebola? days, people can also be infected by direct contact with Fifty to ninety per cent objects (like needles or bed sheets) that contain infectious of patients with Ebola blood or body fluids. -
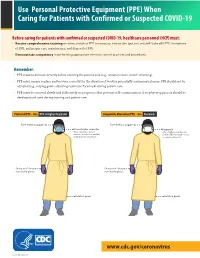
(PPE) When Caring for Patients with Confirmed Or Suspected COVID-19
Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19 Before caring for patients with confirmed or suspected COVID-19, healthcare personnel (HCP) must: • Receive comprehensive training on when and what PPE is necessary, how to don (put on) and doff (take off) PPE, limitations of PPE, and proper care, maintenance, and disposal of PPE. • Demonstrate competency in performing appropriate infection control practices and procedures. Remember: • PPE must be donned correctly before entering the patient area (e.g., isolation room, unit if cohorting). • PPE must remain in place and be worn correctly for the duration of work in potentially contaminated areas. PPE should not be adjusted (e.g., retying gown, adjusting respirator/facemask) during patient care. • PPE must be removed slowly and deliberately in a sequence that prevents self-contamination. A step-by-step process should be COVID-19developed and Personal used during Protective training and patientEquipment care. COVID-19 Personal Protective Equipment (PPE) for Healthcare Personnel (PPE) for Healthcare Personnel Preferred PPE – Use N95 or Higher Respirator Acceptable Alternative PPE – Use Facemask Face shield or goggles Face shield or goggles N95 or higher respirator Facemask When respirators are not N95 or higher respirators are available, use the best available preferred but facemasks are an alternative, like a facemask. acceptable alternative. One pair of clean, One pair of clean, non-sterile gloves non-sterile gloves Isolation gown Isolation gown cdc.gov/COVID19 cdc.gov/COVID19 CS 315838-A 03/20/2020 CS 315838-B 03/20/2020 www.cdc.gov/coronavirus CS 316124-A 06/03/2020 Donning (putting on the gear): More than one donning method may be acceptable. -

GUIDE to INFECTION CONTROL in the HOSPITAL Ebola Virus Disease
GUIDE TO INFECTION CONTROL IN THE HOSPITAL CHAPTER 61: Ebola Virus Disease Author S. Mehtar, MBBS, FRCPath, FCPath, MD Chapter Editor Gonzalo Bearman MD, MPH, FACP, FSHEA, FIDSA Topic Outline Key Issues Known Facts Suggested Practice General Principles Personal Protective Equipment for Healthcare Worker Personal Protective Equipment for Trained Observer Donning and Doffing Disinfection Healthcare Waste Management Suggested Practice in Under-Resourced Settings Summary Helpful Resources References Chapter last updated: February, 2018 KEY ISSUE The 2014 Ebola epidemic was the largest in history with 28,616 cases and 11,310 deaths recorded up to September 2016. There was widespread person-to-person transmission in multiple countries in West Africa, particularly affecting Guinea, Liberia, and Sierra Leone, but also Nigeria. Several countries in Europe and the United States received patients and healthcare workers who became infected with Ebola and were transported home for care. KNOWN FACTS • Ebola virus disease, previously known as Ebola hemorrhagic fever, is an uncommon and deadly disease caused by infection with a virus of the family Filoviridae, genus Ebolavirus. There are four identified Ebola virus species (Zaire, Sudan, Bundibugyo, and Tai Forest Ebola viruses) that cause disease in humans, Zaire being the most common and virulent and responsible for most of the outbreaks. • Ebola viruses are found in several West African countries. The first Ebola virus was discovered in 1976 near the Ebola River in what is now the Democratic Republic of the Congo. A second outbreak in Sudan occurred simultaneously. Since then, over 20 outbreaks have appeared sporadically in Africa but most of them were confined in rural forested areas.