Personal Respiratory Protection
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

BFS 2005 Respiratory Protection Program
Bureau of Forensic Services Issue Date: Revision: Respiratory Protection Program 3/26/2007 1.0 Table of Contents Page #: 1 of 31 Issued by: Lance Gima, Chief 1. Introduction…………………………………………………….. 2 2. Responsibilities………………………………… …………….. 3 3. Definitions……………………………………………………. 5 4. Classification, Description and Limitations of Respirators……. 8 5. Selection of Respirators……………………………………….. 10 6. Use of Respirators……………………………………………… 13 7. Maintenance of Respirators……………………………………. 16 8. Special Issues…..………………………………………………. 18 9. Medical Evaluation…………………………………………….. 19 10. Program Evaluation……………………………………………. 20 Appendix A: Decision Logic for Respirator Selection…………….. 21 Appendix B: Respirator Change-out Schedules…………………… 24 Appendix C: SCBA Monthly Inspection Form……………………. 29 Appendix D: Manufacturer’s Safety Advisory Notices …………... 31 +++ALL PRINTER COPIES ARE UNCONTROLLED+++ Official document location: M:Safety Manual\respprot2007.pdf Bureau of Forensic Services Issue Date: Revision: Respiratory Protection Program 3/26/2007 1.0 Introduction Section 1.0 Page #: 2 of 31 Issued by: Lance Gima, Chief 1. INTRODUCTION Scope This program sets forth accepted practices for respirator users, and provides information and guidance on proper selection, use and maintenance of respirators. Purpose The purpose of this program is to ensure that the Bureau of Forensic Services Respiratory Protection Program provides guidance to all employees using respiratory protection. This program applies to all job related respiratory hazards encountered both in the field and in the laboratory with the exception of clandestine drug labs. Respiratory Protection requirements for response to clandestine drug labs are found in the BFS/BNE Clandestine Laboratory Manual for Instruction and Procedure. Permissible Practice When working in an environment containing harmful dusts, fumes, sprays, mist, fogs, smokes, vapors or gases, the primary method of protection for employees will be engineering control. -

Informing the Use of N95 Respirators by the General Public to Reduce Wildfire Smoke Exposure
Informing the use of N95 respirators by the general public to reduce wildfire smoke exposure Kaitlyn Kelly A thesis submitted in partial fulfillment of the requirements for the degree of Master of Public Health University of Washington 2020 Committee: Tania Busch Isaksen Marc Beaudreau Marissa Baker Program Authorized to Offer Degree: Environmental and Occupational Health Sciences School of Public Health 1 ©Copyright 2020 Kaitlyn Kelly 2 University of Washington Abstract Informing the use of N95 respirators by the general public to reduce wildfire smoke exposure Kaitlyn Kelly Chair of the Supervisory Committee: Tania Busch Isaksen Department of Environmental and Occupational Health Sciences Climate change is increasing the frequency, intensity, and duration of wildfires. To reduce personal exposure to wildfire smoke and resulting adverse health effects, N95 respirators are increasingly used by the general public to filter out fine particles (PM2.5) present in smoke. When mandated in an occupational setting, the use of N95 masks requires medical clearance, proper training, and fit testing. This rigorous attention to training and proper respirator fit is generally, neither required or practiced by, the lay public. A literature resource summary was conducted to understand the current state-of-knowledge around the use of N95 respirators and training in occupational and other settings to inform novel use for the general public during wildfire smoke events. The goal of this study pilot was to assess the efficacy of training materials by quantifying the transference of knowledge from selected interventions into N95 respirator fit in a convenience sample of untrained, lay public. This is the first study to assess efficacy of N95 respirator training materials for the general public during wildfire smoke events. -

EBOLA VIRUS DISEASE Essential Information for Workers
New York Committee for Occupational Safety and Health 61 Broadway Suite 1710, New York, NY 10006 email: [email protected] (212) 227-6440 fax: (212) 227-9854 website: www.nycosh.org Long Island office: NYSUT, 150 Motor Parkway, Suite 306, Hauppauge, NY 11788 (631) 435-1857 fax: (631) 231-4523 EBOLA VIRUS DISEASE Essential Information for Workers (Current as of October 27, 2014) What is Ebola? How does Ebola virus spread? Government and medical experts agree that Ebola virus is Ebola virus disease (EVD), also known as Ebola hemorrhagic spread by direct contact with an infectious SHUVRQ¶V skin, fever (EHF), is a usually fatal disease that can affect blood, or body fluids such as urine, saliva, sweat, feces, humans and some animals. It is caused by infection with the vomit, breast milk, or semen. (Body fluids may contain blood Ebola virus. The first case of Ebola in the U.S. was even if blood is not visible.) Ebola infection may occur via confirmed in September 2014. The first case of transmission liquid contact, splash contact, droplet contact, or hand of Ebola to a health care worker in the U.S. was confirmed in contact with your mouth or nose, with the mucous October 2014. membranes of the eye or eyelid, with punctures on the skin (scabs, scrapes, cuts, injections, etc.) or through sexual acts. Because the virus can survive on surfaces for several How dangerous is Ebola? days, people can also be infected by direct contact with Fifty to ninety per cent objects (like needles or bed sheets) that contain infectious of patients with Ebola blood or body fluids. -

Evaluation of Occupational Exposures to Illicit Drugs at Controlled Substances Laboratories
Evaluation of Occupational Exposures to Illicit Drugs at Controlled Substances Laboratories HHE Report No. 2018-0090-3366 January 2020 Authors: Kendra R. Broadwater, MPH, CIH David A. Jackson, MD Jessica F. Li, MSPH Analytical Support: Bureau Veritas North America Desktop Publisher: Aja Powers Editor: Cheryl Hamilton Industrial Hygiene Field Assistance: Karl Feldmann Logistics: Donnie Booher, Kevin Moore Medical Field and Analytic Assistance: Krishna Surasi, Marie de Perio Keywords: North American Industry Classification System (NAICS) 922120 (Police Protection), Maryland, Forensic Laboratory, Forensic Scientist, Forensic Chemist, Law Enforcement, Illicit Drug, Cocaine, Fentanyl, Heroin, Opioid, Methamphetamine Disclaimer The Health Hazard Evaluation Program investigates possible health hazards in the workplace under the authority of the Occupational Safety and Health Act of 1970 [29 USC 669a(6)]. The Health Hazard Evaluation Program also provides, upon request, technical assistance to federal, state, and local agencies to investigate occupational health hazards and to prevent occupational disease or injury. Regulations guiding the Program can be found in Title 42, Code of Federal Regulations, Part 85; Requests for Health Hazard Evaluations [42 CFR Part 85]. Availability of Report Copies of this report have been sent to the employer, employees, and union at the laboratories. The state and local health departments and the Occupational Safety and Health Administration Regional Office have also received a copy. This report is not copyrighted and may be freely reproduced. Recommended Citation NIOSH [2020]. Evaluation of occupational exposures to illicit drugs at controlled substances laboratories. By Broadwater KR, Jackson DA, Li JF. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Health Hazard Evaluation Report 2018-0090-3366, https://www.cdc.gov/niosh/hhe/reports/pdfs/2018-0090-3366.pdf. -
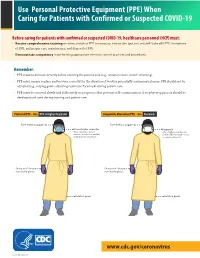
(PPE) When Caring for Patients with Confirmed Or Suspected COVID-19
Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19 Before caring for patients with confirmed or suspected COVID-19, healthcare personnel (HCP) must: • Receive comprehensive training on when and what PPE is necessary, how to don (put on) and doff (take off) PPE, limitations of PPE, and proper care, maintenance, and disposal of PPE. • Demonstrate competency in performing appropriate infection control practices and procedures. Remember: • PPE must be donned correctly before entering the patient area (e.g., isolation room, unit if cohorting). • PPE must remain in place and be worn correctly for the duration of work in potentially contaminated areas. PPE should not be adjusted (e.g., retying gown, adjusting respirator/facemask) during patient care. • PPE must be removed slowly and deliberately in a sequence that prevents self-contamination. A step-by-step process should be COVID-19developed and Personal used during Protective training and patientEquipment care. COVID-19 Personal Protective Equipment (PPE) for Healthcare Personnel (PPE) for Healthcare Personnel Preferred PPE – Use N95 or Higher Respirator Acceptable Alternative PPE – Use Facemask Face shield or goggles Face shield or goggles N95 or higher respirator Facemask When respirators are not N95 or higher respirators are available, use the best available preferred but facemasks are an alternative, like a facemask. acceptable alternative. One pair of clean, One pair of clean, non-sterile gloves non-sterile gloves Isolation gown Isolation gown cdc.gov/COVID19 cdc.gov/COVID19 CS 315838-A 03/20/2020 CS 315838-B 03/20/2020 www.cdc.gov/coronavirus CS 316124-A 06/03/2020 Donning (putting on the gear): More than one donning method may be acceptable. -

GUIDE to INFECTION CONTROL in the HOSPITAL Ebola Virus Disease
GUIDE TO INFECTION CONTROL IN THE HOSPITAL CHAPTER 61: Ebola Virus Disease Author S. Mehtar, MBBS, FRCPath, FCPath, MD Chapter Editor Gonzalo Bearman MD, MPH, FACP, FSHEA, FIDSA Topic Outline Key Issues Known Facts Suggested Practice General Principles Personal Protective Equipment for Healthcare Worker Personal Protective Equipment for Trained Observer Donning and Doffing Disinfection Healthcare Waste Management Suggested Practice in Under-Resourced Settings Summary Helpful Resources References Chapter last updated: February, 2018 KEY ISSUE The 2014 Ebola epidemic was the largest in history with 28,616 cases and 11,310 deaths recorded up to September 2016. There was widespread person-to-person transmission in multiple countries in West Africa, particularly affecting Guinea, Liberia, and Sierra Leone, but also Nigeria. Several countries in Europe and the United States received patients and healthcare workers who became infected with Ebola and were transported home for care. KNOWN FACTS • Ebola virus disease, previously known as Ebola hemorrhagic fever, is an uncommon and deadly disease caused by infection with a virus of the family Filoviridae, genus Ebolavirus. There are four identified Ebola virus species (Zaire, Sudan, Bundibugyo, and Tai Forest Ebola viruses) that cause disease in humans, Zaire being the most common and virulent and responsible for most of the outbreaks. • Ebola viruses are found in several West African countries. The first Ebola virus was discovered in 1976 near the Ebola River in what is now the Democratic Republic of the Congo. A second outbreak in Sudan occurred simultaneously. Since then, over 20 outbreaks have appeared sporadically in Africa but most of them were confined in rural forested areas. -

Tight-Fitting N95 Respirator Mask Training 8-12-20
Tight-fitting N95 Respirator Mask Training N95 Tight-fitting Respirator Mask Use Use during direct care activities that pose risk of exposure to airborne illness Use during Aerosol Generating Procedure (AGP) for coronavirus (COVID-19) positive, presumed-positive, and Person(s) Under investigation (PUI) Use during direct care of individual(s) coronavirus (COVID-19) positive, presumed-positive, and Person(s) Under investigation (PUI) when supply is plenty Employer Responsibilities Institute a respiratory protection plan that is readily available. Provide employees with medical evaluation and fit testing for N95 respirator masks Provide NIOSH and/or FDA approved N95 respirator mask as personal protective equipment (PPE) for employees involved in direct care that N95 may be needed Implement CDC and DDS guidance for optimizing PPE Provide training on use of N95 respirator mask use to employees Employee Responsibilities Participate in fit testing Remove facial hair prior to fit testing Obtain Medical evaluation (May be done at time of fit test my medical provider Understand N95 use Perform user seal check after donning N95 respirator mask Seek answers to any questions related to N95 use N95- Medical Evaluation Questionnaire filled out by a licensed healthcare provider giving clearance for the employee to wear an N95 respirator mask This must be completed prior to N95 fit testing If not approved for N95 mask use, report to management and Human Resources CDC FAQ regarding Medical Evaluation- https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/resps ource3medical.html#medicala Fit testing All N95 respirator mask wearers require fit testing for initial use of N95 respirator. -

Personal Protective Equipment for Use in a Filovirus Disease Outbreak
Personal protective equipment for use in a filovirus disease outbreak Rapid advice guideline Personal protective equipment for use in a filovirus disease outbreak Rapid advice guideline WHO Library Cataloguing-in-Publication Data Personal protective equipment for use in a filovirus disease outbreak: Rapid advice guideline. I.World Health Organization. ISBN 978 92 4 154972 1 Subject headings are available from WHO institutional repository © World Health Organization 2016 All rights reserved. Publications of the World Health Organization are available on the WHO website (http://www. who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (http://www.who.int/about/licensing/ copyright_form/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Fiber Integrity, Filtration Efficiency, and Dipole Charge Density
medRxiv preprint doi: https://doi.org/10.1101/2020.07.07.20148551; this version posted July 9, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. Assessment of N95 and K95 respirator decontamination: fiber integrity, filtration efficiency, and dipole charge density. Wonjun Yim1, Diyi Cheng1, Shiv Patel3, Rui Kui4, Ying Shirley Meng1,2, and Jesse V. Jokerst1,2,5* 1Department of Material Science and Engineering, 2Department of Nanoengineering, 3School of Medicine Simulation Training Center, 4Department of Structural Engineering, 5Department of Radiology, University of California San Diego, 9500 Gilman Drive, La Jolla, CA 92093, Unites States Abstract Personal protective equipment (PPE) including N95 respirators are critical for persons exposed to SARS-CoV-2. KN95 respirators and N95 decontamination protocols have been described as solutions to a lack of such PPE. However, there are a few materials science studies that characterize the charge distribution and physical changes accompanying disinfection treatments particularly heating. Here, we report the filtration efficiency, dipole charge density, and fiber integrity of pristine N95 and KN95 respirators before and after various decontamination methods. We found that the filter layer of N95 is 8-fold thicker than that of KN95, which explains its 10% higher filtration efficiency (97.03 %) versus KN95 (87.76 %) under pristines condition. After 60 minutes of 70 °C treatment, the filtration efficiency and dipole charge density of N95 became 97.16% and 12.48 μC/m2, while those of KN95 were 83.64% and 1.48 μC/m2; moreover, fit factor of N95 was 55 and that of KN95 was 2.7. -

How to Use Personal Protective Equipment: a Quick Reference Guide for Frontline Clinical Providers
How to Use Personal Protective Equipment: A Quick Reference Guide for Frontline Clinical Providers Frontline clinical providers should wear the following personal protective equipment (PPE) when treating individuals confirmed or suspected to be infected with COVID-19. N95 RESPIRATOR GOWN GLOVES FACE SHIELD/ EYE PROTECTION How to properly use protective equipment PPE TYPE DONNING PPE REMOVING PPE • Secure ties or elastic band at middle of • Front of respirator is contaminated – N95 RESPIRATOR head and neck DO NOT TOUCH! • Fit flexible band to nose bridge • Grasp ONLY bottom then top ties/elastics (AS AVAILABLE) • Fit snug to face and below chin and remove • Fit-check respirator • Discard in waste container • Gown front and sleeves are contaminated! • Unfasten neck, then waist ties • Remove gown using a peeling motion; • Fully cover torso from neck to knees, arms pull gown from each shoulder toward the GOWN to end of wrist, and wrap around the back same hand • Fasten in back at neck and waist • Gown will turn inside out • Hold removed gown away from body, roll into a bundle and discard into waste or linen receptacle • Outside of gloves are contaminated! • Grasp outside of glove with opposite • U se non-sterile for isolation gloved hand; peel off GLOVES Select according to hand size • • Hold removed glove in gloved hand • Extend to cover wrist of isolation gown • Slide fingers of ungloved hand under remaining glove at wrist • Outside of goggles or face shield are contaminated! FACE SHIELD / • Put on face and adjust to fit • To remove, handle by “clean” head band EYE PROTECTION or ear pieces • Place in designated receptacle for reprocessing or in waste container Wash hands or use an alcohol-based hand sanitizer immediately after removing all PPE! N95 Respirator Usage and Care N95 respirators must only be used by a single wearer. -

Information on Ebola October 17, 2014
Information on Ebola October 17, 2014 This letter is for informational purposes only. The description of medical and other health-related subjects is no substitute for professional medical advice. Although the authors of this letter have taken great care to ensure that the information corresponds to the current state of knowledge at the time of first publication, this does not release the reader from the responsibility to make his/her own, informed decisions after consultation with trained medical personnel. The products discussed below are solely intended for use by qualified professionals. This informational letter contains basic information on Ebola and links to additional references. Please keep yourself up-to-date on the current situation by reading the web pages listed in this document. Current information on the Ebola virus as well as behavioral recommendations can be found on the following websites: United States Centers for Disease Control and Prevention (CDC) http://www.cdc.gov/vhf/Ebola/about.html World Health Organization (WHO): http://www.who.int/mediacentre/factsheets/fs103/en/ European Centre for Disease Prevention and Control: http://www.ecdc.europa.eu/en/healthtopics/Ebola_marburg_fevers/information- travellers/Pages/information- travellers.aspx Robert Koch Institute (RKI): http://www.rki.de/DE/Content/InfAZ/E/Ebola/Uebersicht.html#doc5045280bodyText3 National Institute for Occupational Safety and Health (NIOSH): http://www.cdc.gov/niosh/ The following information about Ebola is based on the information provided by the above-mentioned institutions. What is Ebola? Ebola is a rare, often fatal virus originating in tropical Africa and associated with symptoms of hemorrhagic fever. This means both internal and external bleeding (hemorrhages) of the body. -
Elastomeric Respirators Effectiveness and Use
Elastomeric Respirators Effectiveness and Use Presented by Nicolas Smit Advocacy • https://twitter.com/ppetoheros • https://correcttheoversight.com/success-stories-news • https://www.northernontariobusiness.com/regional-news/sudbury/sudbury- engineer-urging-mining-industry-to-donate-respirators-2273156 • https://www.ola.org/en/legislative-business/committees/finance-economic- affairs/parliament-42/transcripts/committee-transcript-2020-jul-13#P547_134915 • https://www.sudbury.com/local-news/with-ongoing-n95-shortage-sudburian- advocating-for-donations-of-elastomeric-respirators-2910127 What are elastomeric respirators? • They are tight fitting respirators made of synthetic or natural rubber material, can be repeatedly used, disinfected, stored, and re-used. • They are equipped with replaceable filter cartridges or flexible, disc or pancake-style filters, which are not housed in a cartridge body. • They may also have sealing surfaces and adjustable straps that accommodate a better fit. • Elastomeric respirators have the same basic requirements for an OSHA-approved respiratory protection program as filtering facepiece respirators such as N95s, including medical evaluation, training, and fit testing. However, they have additional maintenance requirements which also include cleaning and disinfection of the face piece components such as straps, valves, and valve covers. Hierarchy of Controls for COVID-19 Prevention https://www.ccohs.ca/bestpractice/resources/1089-COVID-19---Hierarchy-of-Controls-(1).pdf N95 vs Half Face vs Full Face Different