COVID-19 Airway Protection PPE Overview DOCUMENT INTENDED to PROVIDE INSIGHT BASED on CURRENTLY AVAILABLE INFORMATION for CONSIDERATION and NOT SPECIFIC ADVICE
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Learning About Masks
Learn more about MASKS Did you know ?? Some masks and respirators have How are types of masks different? exhalation valves. These are not acceptable during COVID because they can release viral particles in the air. Cloth Mask2,3 Procedure Mask1,2 N95 Respirator1,2 Pros Pros Pros • Keeps other safe by preventing • May offer some additional protection • Dense filter exhalation of viral particles if others don’t mask • Filters airborne particles and droplets • Washable and reusable • Medical grade certfied • Medical grade certfied • Easy to make on your own • Affordable and disposable Cons Cons Cons • Harder to breathe • Not designed for multiple uses • Less filtration • Healthcare providers need them • Healthcare providers need them • No airborne particle protection • Require training to wear properly • Susceptible to some droplets • Doesn’t filter airborne particles Affordability Affordability Affordability Reusability Reusability Reusability Protection Protection Protection Comfort level Comfort level Comfort level 2020 Emory University, created by Visual Medical Education. Updated July 30, 2020 The materials are intended solely for general educational and information purposes, are made available in the context of the public health emergency related to the coronavirus (COVID-19) and have not been subject to review that typically would occur in a non-emergent situation. The materials do not constitute the provision of medical, legal or other Creative Commons Attribution-NonCommercial-NoDerivs professional advice. EMORY UNIVERSITY AND EMORY HEALTHCARE MAKE NO WARRANTIES, EXPRESS OR IMPLIED AS TO THE MATERIALS, INCLUDING, WITHOUT LIMITATION, COMPLIANCE WITH QUALITY, REGULATORY, ACCREDITATION OR STANDARDS OF CARE. EMORY EXPRESSLY DISCLAIMS ANY WARRANTIES OF MERCHANTABILITY OR FITNESS FOR A PARTICULAR PURPOSE. -

Rationale for Mass Masking in Controlling the COVID-19 Pandemic
PERSPECTIVE published: 24 August 2021 doi: 10.3389/fpubh.2021.665708 Rationale for Mass Masking in Controlling the COVID-19 Pandemic Shing Yau Tam 1, Victor C. W. Tam 1, Helen K. W. Law 1, May Ling Khaw 2 and Shara W. Y. Lee 1* 1 Department of Health Technology and Informatics, Faculty of Health and Social Sciences, The Hong Kong Polytechnic University, Kowloon, China, 2 Tasmanian School of Medicine, University of Tasmania, Hobart, TAS, Australia The rapid spread of the coronavirus disease 2019 (COVID-19) into a global pandemic caught the world unprepared. Previously effective measures for containing disease outbreaks were overwhelmed, necessitating strict controls such as lockdowns or curfews. Among the disease control interventions, community mass masking was one of the highly controversial issues with differing opinions on its indications or effectiveness from different health authorities around the world. Regions where community mass masking was timely introduced were associated with lower transmission rates, and more effective disease control. In this article, we discuss the evidence on the effectiveness, and rationale for community mass masking to prevent the COVID-19 transmission. Areas for further research to define the role of mass masking in light of the COVID-19 pandemic will be suggested. This would help policy makers in formulating mass masking policies. Edited by: Bach Tran, Keywords: COVID-19, pandemic, public health, public health policy, face mask, infection control, mass masking Hanoi Medical University, Vietnam Reviewed by: Sukanta Sarkar, INTRODUCTION Indian Institute of Technology Ropar, India The coronavirus disease 2019 (COVID-19) is the result of infection by the novel severe Supa Pengpid, acute respiratory syndrome coronavirus 2 (SARS-CoV2), making this the third coronavirus to Mahidol University, Thailand have crossed species and cause severe disease in humans. -

Universal PPE Guidelines and Faqs (As of August 2, 2021)
Universal PPE Guidelines and FAQs (as of August 2, 2021) Guidance was issued on July 27, 2021, by the Centers for Disease Control and Prevention (CDC) that raises concerns of increased COVID-19 transmission due to the Delta variant. As a result, in alignment with the CDC, Nebraska Medicine is making modifications to the Universal PPE Guidelines to support the increasing numbers of COVID-19 cases in the community. Vaccination remains the most effective way to prevent transmission of disease and is the only way to prevent severe illness with risk of hospitalization and death. Guidance will be updated and/or expanded based on the level of community spread of COVID- 19, the proportion of the population that is fully vaccinated, the rapidly evolving science on COVID-19 vaccines, the understanding of COVID-19 variants and employee health data related to COVID-19 exposure. For the purposes of this document, people are considered fully vaccinated after receiving the full series of the following COVID-19 vaccines: Pfizer/BioNTech, Astrazeneca-SK Bio, Serum Institute of India, Johnson and Johnson (J&J/Janseen), Moderna, Novavax, Sinovac, and Sinopharm Key Points Applicable for ALL Nebraska Medicine Sites: Regardless of vaccination status: o Masks will be required in all clinical settings. o Masks will be required whenever a colleague is indoors in the presence of a patient and/or visitor. o Masks must be doffed and discarded when leaving a droplet/contact precautions isolation room. A new mask must be donned by the colleague immediately after leaving this type of isolation. When masks are used for droplet precautions, the mask becomes contaminated during patient encounters via large droplet particle transmission. -

Informing the Use of N95 Respirators by the General Public to Reduce Wildfire Smoke Exposure
Informing the use of N95 respirators by the general public to reduce wildfire smoke exposure Kaitlyn Kelly A thesis submitted in partial fulfillment of the requirements for the degree of Master of Public Health University of Washington 2020 Committee: Tania Busch Isaksen Marc Beaudreau Marissa Baker Program Authorized to Offer Degree: Environmental and Occupational Health Sciences School of Public Health 1 ©Copyright 2020 Kaitlyn Kelly 2 University of Washington Abstract Informing the use of N95 respirators by the general public to reduce wildfire smoke exposure Kaitlyn Kelly Chair of the Supervisory Committee: Tania Busch Isaksen Department of Environmental and Occupational Health Sciences Climate change is increasing the frequency, intensity, and duration of wildfires. To reduce personal exposure to wildfire smoke and resulting adverse health effects, N95 respirators are increasingly used by the general public to filter out fine particles (PM2.5) present in smoke. When mandated in an occupational setting, the use of N95 masks requires medical clearance, proper training, and fit testing. This rigorous attention to training and proper respirator fit is generally, neither required or practiced by, the lay public. A literature resource summary was conducted to understand the current state-of-knowledge around the use of N95 respirators and training in occupational and other settings to inform novel use for the general public during wildfire smoke events. The goal of this study pilot was to assess the efficacy of training materials by quantifying the transference of knowledge from selected interventions into N95 respirator fit in a convenience sample of untrained, lay public. This is the first study to assess efficacy of N95 respirator training materials for the general public during wildfire smoke events. -

Mask Use in the Context of COVID-19 Interim Guidance 1 December 2020
Mask use in the context of COVID-19 Interim guidance 1 December 2020 This document, which is an update of the guidance published patients wear the following types of mask/respirator in on 5 June 2020, includes new scientific evidence relevant to addition to other personal protective equipment that are the use of masks for reducing the spread of SARS-CoV-2, the part of standard, droplet and contact precautions: virus that causes COVID-19, and practical considerations. It medical mask in the absence of aerosol contains updated evidence and guidance on the following: generating procedures (AGPs) • mask management; respirator, N95 or FFP2 or FFP3 standards, or • SARS-CoV-2 transmission; equivalent in care settings for COVID-19 • masking in health facilities in areas with community, patients where AGPs are performed; these may cluster and sporadic transmission; be used by health workers when providing care • mask use by the public in areas with community and to COVID-19 patients in other settings if they cluster transmission; are widely available and if costs is not an issue. • alternatives to non-medical masks for the public; • In areas of known or suspected community or cluster • exhalation valves on respirators and non-medical masks; SARS-CoV-2 transmission WHO advises the following: • mask use during vigorous intensity physical activity; universal masking for all persons (staff, patients, visitors, service providers and others) within the • essential parameters to be considered when health facility (including primary, secondary manufacturing non-medical masks (Annex). and tertiary care levels; outpatient care; and Key points long-term care facilities) wearing of masks by inpatients when physical • The World Health Organization (WHO) advises the use distancing of at least 1 metre cannot be of masks as part of a comprehensive package of maintained or when patients are outside of their prevention and control measures to limit the spread of care areas. -

EBOLA VIRUS DISEASE Essential Information for Workers
New York Committee for Occupational Safety and Health 61 Broadway Suite 1710, New York, NY 10006 email: [email protected] (212) 227-6440 fax: (212) 227-9854 website: www.nycosh.org Long Island office: NYSUT, 150 Motor Parkway, Suite 306, Hauppauge, NY 11788 (631) 435-1857 fax: (631) 231-4523 EBOLA VIRUS DISEASE Essential Information for Workers (Current as of October 27, 2014) What is Ebola? How does Ebola virus spread? Government and medical experts agree that Ebola virus is Ebola virus disease (EVD), also known as Ebola hemorrhagic spread by direct contact with an infectious SHUVRQ¶V skin, fever (EHF), is a usually fatal disease that can affect blood, or body fluids such as urine, saliva, sweat, feces, humans and some animals. It is caused by infection with the vomit, breast milk, or semen. (Body fluids may contain blood Ebola virus. The first case of Ebola in the U.S. was even if blood is not visible.) Ebola infection may occur via confirmed in September 2014. The first case of transmission liquid contact, splash contact, droplet contact, or hand of Ebola to a health care worker in the U.S. was confirmed in contact with your mouth or nose, with the mucous October 2014. membranes of the eye or eyelid, with punctures on the skin (scabs, scrapes, cuts, injections, etc.) or through sexual acts. Because the virus can survive on surfaces for several How dangerous is Ebola? days, people can also be infected by direct contact with Fifty to ninety per cent objects (like needles or bed sheets) that contain infectious of patients with Ebola blood or body fluids. -
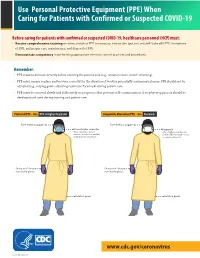
(PPE) When Caring for Patients with Confirmed Or Suspected COVID-19
Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19 Before caring for patients with confirmed or suspected COVID-19, healthcare personnel (HCP) must: • Receive comprehensive training on when and what PPE is necessary, how to don (put on) and doff (take off) PPE, limitations of PPE, and proper care, maintenance, and disposal of PPE. • Demonstrate competency in performing appropriate infection control practices and procedures. Remember: • PPE must be donned correctly before entering the patient area (e.g., isolation room, unit if cohorting). • PPE must remain in place and be worn correctly for the duration of work in potentially contaminated areas. PPE should not be adjusted (e.g., retying gown, adjusting respirator/facemask) during patient care. • PPE must be removed slowly and deliberately in a sequence that prevents self-contamination. A step-by-step process should be COVID-19developed and Personal used during Protective training and patientEquipment care. COVID-19 Personal Protective Equipment (PPE) for Healthcare Personnel (PPE) for Healthcare Personnel Preferred PPE – Use N95 or Higher Respirator Acceptable Alternative PPE – Use Facemask Face shield or goggles Face shield or goggles N95 or higher respirator Facemask When respirators are not N95 or higher respirators are available, use the best available preferred but facemasks are an alternative, like a facemask. acceptable alternative. One pair of clean, One pair of clean, non-sterile gloves non-sterile gloves Isolation gown Isolation gown cdc.gov/COVID19 cdc.gov/COVID19 CS 315838-A 03/20/2020 CS 315838-B 03/20/2020 www.cdc.gov/coronavirus CS 316124-A 06/03/2020 Donning (putting on the gear): More than one donning method may be acceptable. -
Guidance for the Selection and Use of PPE in the Healthcare Setting
Guidance for the Selection and Use of Personal Protective Equipment (PPE) in Healthcare Settings 1 PPE Use in Healthcare Settings: Program Goal Improve personnel safety in the healthcare environment through appropriate use of PPE. PPE Use in Healthcare Settings The goal of this program is to improve personnel safety in the healthcare environment through appropriate use of PPE. 2 PPE Use in Healthcare Settings: Program Objectives • Provide information on the selection and use of PPE in healthcare settings • Practice how to safely don and remove PPE PPE Use in Healthcare Settings The objectives of this program are to provide information on the selection and use of PPE in healthcare settings and to allow time for participants to practice the correct way to don and remove PPE. 3 Personal Protective Equipment Definition “specialized clothing or equipment worn by an employee for protection against infectious materials” (OSHA) PPE Use in Healthcare Settings Personal protective equipment, or PPE, as defined by the Occupational Safety and Health Administration, or OSHA, is “specialized clothing or equipment, worn by an employee for protection against infectious materials.” 4 Regulations and Recommendations for PPE • OSHA issues workplace health and safety regulations. Regarding PPE, employers must: – Provide appropriate PPE for employees – Ensure that PPE is disposed or reusable PPE is cleaned, laundered, repaired and stored after use • OSHA also specifies circumstances for which PPE is indicated • CDC recommends when, what and how to use PPE PPE Use in Healthcare Settings OSHA issues regulations for workplace health and safety. These regulations require use of PPE in healthcare settings to protect healthcare personnel from exposure to bloodborne pathogens and Mycobacterium tuberculosis. -

Manufacturers of Surgical Masks; Health Care Personnel; Hospital Purchasing Departments; Authorized Distributors and Authorized Importers; and Any Other Stakeholders
August 5, 2020 To: Manufacturers of Surgical Masks; Health Care Personnel; Hospital Purchasing Departments; Authorized Distributors and Authorized Importers; and Any Other Stakeholders The U.S. Food and Drug Administration (FDA) is issuing this Emergency Use Authorization (EUA) in response to concerns relating to the insufficient supply and availability of disposable, single-use surgical masks1,2 (hereafter also referred to as “surgical masks”) for use in healthcare settings by health care personnel (HCP)3 as personal protective equipment (PPE)4 to provide a physical barrier to fluids and particulate materials to prevent HCP exposure to respiratory droplets and large particles during surgical mask shortages resulting from the Coronavirus Disease 2019 (COVID-19) pandemic, pursuant to section 564 of the Federal, Food, Drug, and Cosmetic Act (the Act) (21 U.S.C. 360bbb-3). On February 4, 2020, pursuant to Section 564(b)(1)(C) of the Act, the Secretary of the Department of Health and Human Services (HHS) determined that there is a public health emergency that has a significant potential to affect national security or the health and security of United States citizens living abroad, and that involves the virus that causes COVID-19.5 1 A surgical mask is a mask that covers the user’s nose and mouth and provides a physical barrier to fluids and particulate materials. Surgical masks are generally regulated by FDA as Class II devices under 21 CFR 878.4040 – Surgical apparel. 2 FDA-cleared surgical face masks, non-surgical face masks, surgical masks with antimicrobial/antiviral agent, and all particulate filtering facepiece respirators are not within the scope of this authorization. -

Respiratory Infection Control: Respirators Versus Surgical Masks
FactSheet Respiratory Infection Control: Respirators Versus Surgical Masks It is important that employers and workers understand the significant differences between these two types of personal protective equipment. The decision whether or not to require workers to use either surgical masks or respirators must be based upon a hazard analysis of the workers’ specific work environments and the different protective properties of each type of personal protective equipment. The use of surgical masks or respirators is one practice that may reduce the risk of infectious disease transmission between infected and noninfected persons. Since there is limited historical information on the effectiveness of surgical masks and respirators for the control of influenza during any previous pandemics, the effectiveness of surgical masks and respirators has been inferred on the basis of the mode of influenza transmission, particle size and professional judgment. To offer protection, both surgical masks and respirators need to be worn correctly and consistently. If used properly, surgical masks and respirators both have a role in preventing who have influenza‑like symptoms. These different types of exposures. During an influenza generally include those workers who work in pandemic, surgical masks and respirators need occupations classified as very high exposure to be used in conjunction with interventions that risk or high exposure risk to pandemic influenza. are known to prevent the spread of infection, For additional information on very high and such as engineering and administrative controls high exposure risk occupations, please refer to (e.g., installing sneeze guards, teleworking) OSHA’s Guidance on Preparing Workplaces for and work practices (e.g., cough etiquette, hand an Influenza Pandemic at www.osha.gov/SLTC/ hygiene, and avoiding large gatherings). -
Face Masks, Eyewear and N95 Respirators Every Protection Level and Preference Choose the Right Mask for Every Procedure
Face masks, eyewear and N95 respirators Every protection level and preference Choose the right mask for every procedure Different procedures require different levels of protection, and ASTM standards make it easy for your staff to get the ideal face mask for any procedure-and for every preference. Measuring fluid resistance, filtration and breathability, ASTM categorizes masks into three levels ASTM Level 1 ASTM Level 2 ASTM Level 3 For procedures producing For procedures producing For procedures producing low amounts of fluid, spray light to moderate amounts moderate to heavy amounts and/or aerosols. of fluid, spray and/or aerosols. of fluid, spray and/or aerosols. Fluid Fluid resistance Fluid resistance resistance LEVEL 1 LEVEL 2 LEVEL 3 2 Medline To meet ASTM F2100-19 standards, our masks undergo a series of tests for particle filtration (PFE), bacterial filtration (BFE), differential pressure or breathability (∆P) and fluid resistance. Level 1 Level 2 Level 3 Low fluids Light to moderate fluids Moderate to high fluids PFE at 0.1 micron ≥95% ≥98% ≥98% ASTM F2299 BFE at 3.0 micron ≥95% ≥98% ≥98% ASTM F2101 Delta P (∆P) mm H 0/cm2 2 <5 <6 <6 MIL-M-36954C Fluid resistance ≥80 mm Hg (mmHg) ≥80 mm Hg ≥120 mm Hg ≥160 mm Hg Flammability Class 1 Class 1 Class 1 How small is a micron? Fluid resistance Tests penetration resistance to While an actual micron is not visible to the human eye, synthetic blood at three protection this magnified diagram demonstrates particulate size levels—80 mm Hg, 120 mm Hg and by comparing a micron to other common substances. -

GUIDE to INFECTION CONTROL in the HOSPITAL Ebola Virus Disease
GUIDE TO INFECTION CONTROL IN THE HOSPITAL CHAPTER 61: Ebola Virus Disease Author S. Mehtar, MBBS, FRCPath, FCPath, MD Chapter Editor Gonzalo Bearman MD, MPH, FACP, FSHEA, FIDSA Topic Outline Key Issues Known Facts Suggested Practice General Principles Personal Protective Equipment for Healthcare Worker Personal Protective Equipment for Trained Observer Donning and Doffing Disinfection Healthcare Waste Management Suggested Practice in Under-Resourced Settings Summary Helpful Resources References Chapter last updated: February, 2018 KEY ISSUE The 2014 Ebola epidemic was the largest in history with 28,616 cases and 11,310 deaths recorded up to September 2016. There was widespread person-to-person transmission in multiple countries in West Africa, particularly affecting Guinea, Liberia, and Sierra Leone, but also Nigeria. Several countries in Europe and the United States received patients and healthcare workers who became infected with Ebola and were transported home for care. KNOWN FACTS • Ebola virus disease, previously known as Ebola hemorrhagic fever, is an uncommon and deadly disease caused by infection with a virus of the family Filoviridae, genus Ebolavirus. There are four identified Ebola virus species (Zaire, Sudan, Bundibugyo, and Tai Forest Ebola viruses) that cause disease in humans, Zaire being the most common and virulent and responsible for most of the outbreaks. • Ebola viruses are found in several West African countries. The first Ebola virus was discovered in 1976 near the Ebola River in what is now the Democratic Republic of the Congo. A second outbreak in Sudan occurred simultaneously. Since then, over 20 outbreaks have appeared sporadically in Africa but most of them were confined in rural forested areas.