Guidance for the Selection and Use of PPE in the Healthcare Setting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Eye Protection Health Alert Final 11 25 08.Pub
HEALTH ALERT! Keeping an Eye On Eye Protection More than 2,000 workplace eye injuries occur EVERY DAY in the United States. A vast majority of employers provide eye protection at no cost to their employees, however 94% of eyewear being used by workers is not appropriate for the job being done and about 40% of the workers receive no eye safety training on where and what type of eyewear should be used. “90% of occupational eye injuries could have been prevented if the victim was wearing proper eye and face protection” (Prevent Blindness America) The Bureau of Labor Statistics reported that 36,680 non-fatal work-related eye injuries occurred in private industry workplaces in 2004 at an estimated expense of $300 million in lost production time, medical expenses, and worker’s compensation costs. Fast Facts on Eye Injuries Eye Protection Safety Plan 9 69% of all reported facial injuries 9 Engineering Controls ~ Machine occurred to the eye. guarding, welding curtains, appropriate visible signage. 9 Nearly 70% of non-fatal eye injuries were caused by flying or falling objects 9 Administrative Controls ~ Prohibit access or sparks striking the eye. to work zones for non-workers and workers without proper safety equipment. 9 Males 25-44 years of age are at highest risk for eye injuries. 9 Personal Protective Equipment ~ Use of fitted, job specific, ANSI certified 9 The majority of eye injuries occur in protective eyewear and facewear. welders, cutters, solderers and braziers, followed by construction laborers. 9 Cleaning & Maintenance ~ Ensure proper cleaning of lens and face shields with appropriate materials and store properly to prevent damage. -

Learning About Masks
Learn more about MASKS Did you know ?? Some masks and respirators have How are types of masks different? exhalation valves. These are not acceptable during COVID because they can release viral particles in the air. Cloth Mask2,3 Procedure Mask1,2 N95 Respirator1,2 Pros Pros Pros • Keeps other safe by preventing • May offer some additional protection • Dense filter exhalation of viral particles if others don’t mask • Filters airborne particles and droplets • Washable and reusable • Medical grade certfied • Medical grade certfied • Easy to make on your own • Affordable and disposable Cons Cons Cons • Harder to breathe • Not designed for multiple uses • Less filtration • Healthcare providers need them • Healthcare providers need them • No airborne particle protection • Require training to wear properly • Susceptible to some droplets • Doesn’t filter airborne particles Affordability Affordability Affordability Reusability Reusability Reusability Protection Protection Protection Comfort level Comfort level Comfort level 2020 Emory University, created by Visual Medical Education. Updated July 30, 2020 The materials are intended solely for general educational and information purposes, are made available in the context of the public health emergency related to the coronavirus (COVID-19) and have not been subject to review that typically would occur in a non-emergent situation. The materials do not constitute the provision of medical, legal or other Creative Commons Attribution-NonCommercial-NoDerivs professional advice. EMORY UNIVERSITY AND EMORY HEALTHCARE MAKE NO WARRANTIES, EXPRESS OR IMPLIED AS TO THE MATERIALS, INCLUDING, WITHOUT LIMITATION, COMPLIANCE WITH QUALITY, REGULATORY, ACCREDITATION OR STANDARDS OF CARE. EMORY EXPRESSLY DISCLAIMS ANY WARRANTIES OF MERCHANTABILITY OR FITNESS FOR A PARTICULAR PURPOSE. -

TIN CAS Number
Common Name: TIN CAS Number: 7440-31-5 RTK Substance number: 1858 DOT Number: None Date: January 1986 Revision: April 2001 ------------------------------------------------------------------------- ------------------------------------------------------------------------- HAZARD SUMMARY WORKPLACE EXPOSURE LIMITS * Tin can affect you when breathed in. OSHA: The legal airborne permissible exposure limit * Contact can irritate the skin and eyes. (PEL) is 2 mg/m3 averaged over an 8-hour * Breathing Tin can irritate the nose, throat and lungs workshift. causing coughing, wheezing and/or shortness of breath. * Tin can cause nausea, vomiting, diarrhea and abdominal NIOSH: The recommended airborne exposure limit is pain, headache, fatigue and tremors. 2 mg/m3 averaged over a 10-hour workshift. * Tin can cause "spots" to appear on chest x-ray with normal lung function (stannosis). ACGIH: The recommended airborne exposure limit is 3 * Tin may damage the liver and kidneys. 2 mg/m averaged over an 8-hour workshift. * High exposure can affect the nervous system. WAYS OF REDUCING EXPOSURE IDENTIFICATION * Where possible, enclose operations and use local exhaust Tin is a soft, white, silvery metal or a grey-green powder. It ventilation at the site of chemical release. If local exhaust is found in alloys, Babbitt and similar metal types, and is used ventilation or enclosure is not used, respirators should be as a protective coating and in glass bottle and can worn. manufacturing. * Wear protective work clothing. * Wash thoroughly immediately after exposure to Tin. REASON FOR CITATION * Post hazard and warning information in the work area. In * Tin is on the Hazardous Substance List because it is addition, as part of an ongoing education and training regulated by OSHA and cited by ACGIH and NIOSH. -

Rationale for Mass Masking in Controlling the COVID-19 Pandemic
PERSPECTIVE published: 24 August 2021 doi: 10.3389/fpubh.2021.665708 Rationale for Mass Masking in Controlling the COVID-19 Pandemic Shing Yau Tam 1, Victor C. W. Tam 1, Helen K. W. Law 1, May Ling Khaw 2 and Shara W. Y. Lee 1* 1 Department of Health Technology and Informatics, Faculty of Health and Social Sciences, The Hong Kong Polytechnic University, Kowloon, China, 2 Tasmanian School of Medicine, University of Tasmania, Hobart, TAS, Australia The rapid spread of the coronavirus disease 2019 (COVID-19) into a global pandemic caught the world unprepared. Previously effective measures for containing disease outbreaks were overwhelmed, necessitating strict controls such as lockdowns or curfews. Among the disease control interventions, community mass masking was one of the highly controversial issues with differing opinions on its indications or effectiveness from different health authorities around the world. Regions where community mass masking was timely introduced were associated with lower transmission rates, and more effective disease control. In this article, we discuss the evidence on the effectiveness, and rationale for community mass masking to prevent the COVID-19 transmission. Areas for further research to define the role of mass masking in light of the COVID-19 pandemic will be suggested. This would help policy makers in formulating mass masking policies. Edited by: Bach Tran, Keywords: COVID-19, pandemic, public health, public health policy, face mask, infection control, mass masking Hanoi Medical University, Vietnam Reviewed by: Sukanta Sarkar, INTRODUCTION Indian Institute of Technology Ropar, India The coronavirus disease 2019 (COVID-19) is the result of infection by the novel severe Supa Pengpid, acute respiratory syndrome coronavirus 2 (SARS-CoV2), making this the third coronavirus to Mahidol University, Thailand have crossed species and cause severe disease in humans. -
Personal Protective Equipment (PPE) Guide
Personal Protective Equipment (PPE) Guide Volume 1: General PPE February 2003 F417-207-000 This guide is designed to be used by supervisors, lead workers, managers, employers, and anyone responsible for the safety and health of employees. Employees are also encouraged to use information in this guide to analyze their own jobs, be aware of work place hazards, and take active responsibility for their own safety. Photos and graphic illustrations contained within this document were provided courtesy of the Occupational Safety and Health Administration (OSHA), Oregon OSHA, United States Coast Guard, EnviroWin Safety, Microsoft Clip Gallery (Online), and the Washington State Department of Labor and Industries. TABLE OF CONTENTS (If viewing this pdf document on the computer, you can place the cursor over the section headings below until a hand appears and then click. You can also use the Adobe Acrobat Navigation Pane to jump directly to the sections.) How To Use This Guide.......................................................................................... 4 A. Introduction.........................................................................................6 B. What you are required to do ..............................................................8 1. Do a Hazard Assessment for PPE and document it ........................................... 8 2. Select and provide appropriate PPE to your employees................................... 10 3. Provide training to your employees and document it ........................................ 11 -
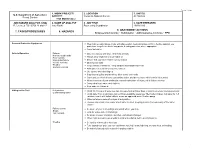
7. Tasks/Procedures 8. Hazards 9. Abatement
FS-6700-7 (11/99) 1. WORK PROJECT/ 2. LOCATION 3. UNIT(S) U.S. Department of Agriculture ACTIVITY Coconino National Forest All Districts Forest Service Trail Maintenance JOB HAZARD ANALYSIS (JHA) 4. NAME OF ANALYST 5. JOB TITLE 6. DATE PREPARED References-FSH 6709.11 and 12 Amy Racki Partnership Coordinator 10/28/2013 9. ABATEMENT ACTIONS 7. TASKS/PROCEDURES 8. HAZARDS Engineering Controls * Substitution * Administrative Controls * PPE Personal Protective Equipment Wear helmet, work gloves, boots with slip-resistant heels and soles with firm, flexible support, eye protection, long sleeve shirts, long pants, hearing protection where appropriate Carry first aid kit Vehicle Operation Fatigue Drive defensively and slow. Watch for animals Narrow, rough roads Always wear seatbelts and turn lights on Poor visibility Mechanical failure Ensure that you have reliable communication Vehicle Accients Obey speed limits Weather Keep vehicles maintained. Keep windows and windshield clean Animals on Road Anticipate careless actions by other drivers Use spotter when backing up Stay clear of gullies and trenches, drive slowly over rocks. Carry and use chock blocks, use parking brake, and do not leave vehicle while it is running Inform someone of your destination and estimated time of return, call in if plans change Carry extra food, water, and clothing Stop and rest if fatigued Hiking on the Trail Dehydration Drink 12-15 quarts of water per day, increase fluid on hotter days or during extremely strenuous activity Contaminated water Drink -

Healthcare Reform in Russia: Problems and William Tompson Prospects
OECD Economics Department Working Papers No. 538 Healthcare Reform in Russia: Problems and William Tompson Prospects https://dx.doi.org/10.1787/327014317703 Unclassified ECO/WKP(2006)66 Organisation de Coopération et de Développement Economiques Organisation for Economic Co-operation and Development 15-Jan-2007 ___________________________________________________________________________________________ _____________ English text only ECONOMICS DEPARTMENT Unclassified ECO/WKP(2006)66 HEALTHCARE REFORM IN RUSSIA: PROBLEMS AND PROSPECTS ECONOMICS DEPARTMENT WORKING PAPERS No. 538 By William Tompson All Economics Department Working Papers are available through OECD's website at www.oecd.org/eco/working_papers text only English JT03220416 Document complet disponible sur OLIS dans son format d'origine Complete document available on OLIS in its original format ECO/WKP(2006)66 ABSTRACT/RÉSUMÉ Healthcare Reform in Russia: Problems and Prospects This paper examines the prospects for reform of Russia’s healthcare system. It begins by exploring a number of fundamental imbalances that characterise the current half-reformed system of healthcare provision before going on to assess the government’s plans for going ahead with healthcare reform over the medium term. The challenges it faces include strengthening primary care provision and reducing the current over-reliance on tertiary care; restructuring the incentives facing healthcare providers; and completing the reform of the system of mandatory medical insurance. This paper relates to the OECD Economic Survey of the Russian Federation 2006 (www.oecd.org/eco/surveys/russia). JEL classification: I11, I12, I18 Keywords: Russia; healthcare; health insurance; competition; primary care; hospitalisation; pharmaceuticals; single payer; ***************** La reforme du système de santé en Russie: problèmes et perspectives La présente étude analyse les perspectives de réforme du système de santé en Russie. -

July 23, 2021 the Musicrow Weekly Friday, July 23, 2021
July 23, 2021 The MusicRow Weekly Friday, July 23, 2021 Taylor Swift’s Fearless (Taylor’s Version) SIGN UP HERE (FREE!) Will Not Be Submitted For Grammy, CMA Award Consideration If you were forwarded this newsletter and would like to receive it, sign up here. THIS WEEK’S HEADLINES Fearless (Taylor’s Version) Will Not Be Submitted For Grammy, CMA Awards NSAI Sets Nashville Songwriter Awards For September Big Loud Records Ups 5, Adds 2 To Promotion Team Dylan Schneider Signs With BBR Music Group Taylor Swift will not be submitting Fearless (Taylor’s Version), the re- recorded version of her 2008 studio album that released earlier this year, Dan + Shay Have Good for Grammy or CMA Awards consideration. Things In Store For August “After careful consideration, Taylor Swift will not be submitting Fearless (Taylor’s Version) in any category at this year’s upcoming Grammy and Scotty McCreery Shares CMA Awards,” says a statement provided to MusicRow from a Republic Details Of New Album Records spokesperson. “Fearless has already won four Grammys including album of the year, as well as the CMA Award for album of the Chris DeStefano Renews year in 2009/2010 and remains the most awarded country album of all With Sony Music Publishing time.” Natalie Hemby Announces The statement goes on to share that Swift’s ninth studio album, Evermore, New Album released in December of 2020, will be submitted to the Grammys for consideration in all eligible categories. Niko Moon’s Good Time Slated For August Release Evermore arrived only five months after the surprise release of Folklore, Swift’s groundbreaking eighth studio album. -

Five Keys to Safer Food Manual
FIVE KEYS TO SAFER FOOD MANUAL DEPARTMENT OF FOOD SAFETY, ZOONOSES AND FOODBORNE DISEASES FIVE KEYS TO SAFER FOOD MANUAL DEPARTMENT OF FOOD SAFETY, ZOONOSES AND FOODBORNE DISEASES INTRODUCTION Food safety is a significant public health issue nsafe food has been a human health problem since history was first recorded, and many food safety Uproblems encountered today are not new. Although governments all over the world are doing their best to improve the safety of the food supply, the occurrence of foodborne disease remains a significant health issue in both developed and developing countries. It has been estimated that each year 1.8 million people die as a result of diarrhoeal diseases and most of these cases can be attributed to contaminated food or water. Proper food preparation can prevent most foodborne diseases. More than 200 known diseases are transmitted through food.1 The World Health Organization (WHO) has long been aware of the need to educate food handlers about their responsibilities for food safety. In the early 1990s, WHO developed the Ten Golden Rules for Safe Food Preparation, which were widely translated and reproduced. However, it became obvious that something simpler and more generally applicable was needed. After nearly a year of consultation with food safety expertsandriskcommunicators, WHOintroducedtheFive KeystoSaferFoodposterin2001.TheFive Keys toSaferFoodposterincorporatesallthemessagesoftheTen Golden Rules for Safe Food Preparation under simpler headings that are more easily remembered and also provides more details on the reasoning behind the suggested measures. The Five Keys to Safer Food Poster The core messages of the Five Keys to Safer Food are: (1) keep clean; (2) separate raw and cooked; (3) cook thoroughly; (4) keep food at safe temperatures; and (5) use safe water and raw materials. -

Respirator on / Respirator Off
Respirator On / Respirator Off When you put on a disposable respirator Position your respirator correctly and check the seal to protect yourself from COVID-19. Cup the respirator in your hand. Place your fingertips from both Place both hands over the Select other PPE items that do not Hold the respirator under your hands at the top of the metal respirator, take a quick breath in interfere with the fit or chin with the nose piece up. The nose clip (if present). Slide to check the seal. Breathe out. If performance of your respirator. top strap (on single or double fingertips down both sides of you feel a leak when breathing strap respirators) goes over the metal strip to mold the nose in or breathing out, there is not and rests at the top back of area to the shape of your nose. a proper seal. your head. The bottom strap is positioned around the neck and below the ears. X X X X X Do not use a respirator that Do not allow facial hair, jewelry, Do not crisscross the straps. Do not wear a respirator that Do not touch the front of the appears damaged or deformed, glasses, clothing, or anything does not have a proper seal. If respirator during or after use! no longer forms an effective else to prevent proper placement air leaks in or out, ask for help It may be contaminated. seal to the face, becomes wet or to come between your face or try a different size or model. or visibly dirty, or if breathing and the respirator. -

Universal PPE Guidelines and Faqs (As of August 2, 2021)
Universal PPE Guidelines and FAQs (as of August 2, 2021) Guidance was issued on July 27, 2021, by the Centers for Disease Control and Prevention (CDC) that raises concerns of increased COVID-19 transmission due to the Delta variant. As a result, in alignment with the CDC, Nebraska Medicine is making modifications to the Universal PPE Guidelines to support the increasing numbers of COVID-19 cases in the community. Vaccination remains the most effective way to prevent transmission of disease and is the only way to prevent severe illness with risk of hospitalization and death. Guidance will be updated and/or expanded based on the level of community spread of COVID- 19, the proportion of the population that is fully vaccinated, the rapidly evolving science on COVID-19 vaccines, the understanding of COVID-19 variants and employee health data related to COVID-19 exposure. For the purposes of this document, people are considered fully vaccinated after receiving the full series of the following COVID-19 vaccines: Pfizer/BioNTech, Astrazeneca-SK Bio, Serum Institute of India, Johnson and Johnson (J&J/Janseen), Moderna, Novavax, Sinovac, and Sinopharm Key Points Applicable for ALL Nebraska Medicine Sites: Regardless of vaccination status: o Masks will be required in all clinical settings. o Masks will be required whenever a colleague is indoors in the presence of a patient and/or visitor. o Masks must be doffed and discarded when leaving a droplet/contact precautions isolation room. A new mask must be donned by the colleague immediately after leaving this type of isolation. When masks are used for droplet precautions, the mask becomes contaminated during patient encounters via large droplet particle transmission. -

New Information from MSA Safety Works Regarding EPA Lead Requirements for Remodelers
New Information from MSA Safety Works Regarding EPA Lead Requirements for Remodelers Safety Products for Remodelers for Lead Exposure Protection during Renovation, Repair and Painting Renovation of older structures can create hazardous lead dust and Personal Protective Equipment chips within those environments by disturbing lead-based paint. In • Eyewear (MSA recommends ANSI-compliant safety glasses or response to the need to help prevent lead poisoning, in 2008 the U.S. goggles - see below) Environmental Protection Agency (EPA) issued a rule requiring use of • Painters’ hats lead-safe practices, as common renovation activities such as sanding, • Gloves cutting, and demolition can create serious lead exposure hazards. • Coveralls • Disposable shoe covers As of April 22, 2010, the EPA requires that contractors performing • N-100-rated disposable respirators (MSA recommends renovation activities that disturb lead-based paint in pre-1978-built P-100 rated respirators – see below) homes, child-care facilities, and schools must be certified and must follow specific work practices aimed at preventing lead contamination. The “eyewear” referred to by the EPA comprises safety glasses or Contractors must document compliance with this requirement and goggles compliant to the latest American National Standards Institute provide certification to customers when asked to do so. Z87.1 standard. If remodelers remove lead paint with chemical strippers, chemical splash goggles (ANSI-compliant goggles with Contractors performing work in homes, child-care