Elastomeric Half Face Respirator Use Document Type: Procedure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Respirator on / Respirator Off
Respirator On / Respirator Off When you put on a disposable respirator Position your respirator correctly and check the seal to protect yourself from COVID-19. Cup the respirator in your hand. Place your fingertips from both Place both hands over the Select other PPE items that do not Hold the respirator under your hands at the top of the metal respirator, take a quick breath in interfere with the fit or chin with the nose piece up. The nose clip (if present). Slide to check the seal. Breathe out. If performance of your respirator. top strap (on single or double fingertips down both sides of you feel a leak when breathing strap respirators) goes over the metal strip to mold the nose in or breathing out, there is not and rests at the top back of area to the shape of your nose. a proper seal. your head. The bottom strap is positioned around the neck and below the ears. X X X X X Do not use a respirator that Do not allow facial hair, jewelry, Do not crisscross the straps. Do not wear a respirator that Do not touch the front of the appears damaged or deformed, glasses, clothing, or anything does not have a proper seal. If respirator during or after use! no longer forms an effective else to prevent proper placement air leaks in or out, ask for help It may be contaminated. seal to the face, becomes wet or to come between your face or try a different size or model. or visibly dirty, or if breathing and the respirator. -

Informing the Use of N95 Respirators by the General Public to Reduce Wildfire Smoke Exposure
Informing the use of N95 respirators by the general public to reduce wildfire smoke exposure Kaitlyn Kelly A thesis submitted in partial fulfillment of the requirements for the degree of Master of Public Health University of Washington 2020 Committee: Tania Busch Isaksen Marc Beaudreau Marissa Baker Program Authorized to Offer Degree: Environmental and Occupational Health Sciences School of Public Health 1 ©Copyright 2020 Kaitlyn Kelly 2 University of Washington Abstract Informing the use of N95 respirators by the general public to reduce wildfire smoke exposure Kaitlyn Kelly Chair of the Supervisory Committee: Tania Busch Isaksen Department of Environmental and Occupational Health Sciences Climate change is increasing the frequency, intensity, and duration of wildfires. To reduce personal exposure to wildfire smoke and resulting adverse health effects, N95 respirators are increasingly used by the general public to filter out fine particles (PM2.5) present in smoke. When mandated in an occupational setting, the use of N95 masks requires medical clearance, proper training, and fit testing. This rigorous attention to training and proper respirator fit is generally, neither required or practiced by, the lay public. A literature resource summary was conducted to understand the current state-of-knowledge around the use of N95 respirators and training in occupational and other settings to inform novel use for the general public during wildfire smoke events. The goal of this study pilot was to assess the efficacy of training materials by quantifying the transference of knowledge from selected interventions into N95 respirator fit in a convenience sample of untrained, lay public. This is the first study to assess efficacy of N95 respirator training materials for the general public during wildfire smoke events. -

COVID-19 Guidance on the Reuse of Elastomeric (Half Mask) Respirators
COVID-19 Guidance on the Reuse of Elastomeric (Half Mask) Respirators This guidance is adapted for use in Manitoba from materials developed by McGill University Health Centre. CONTEXT Reusable respirators (specifically, reusable half-facepiece elastomeric respirators) are the standard respiratory protection device used in many industries and in certain healthcare settings and facilities. The durability and reusability of elastomeric respirators make them desirable for stockpiling for emergencies, where the need for large volumes of respirators can be anticipated. MATERIAL Elastomeric Half-Facepiece Respirators (EHFR) (see annex 1 to compare with other masks/respirators) are half-face, tight-fitting respirators made of synthetic or rubber material. These materials permit them to be repeatedly disinfected, cleaned, and reused. PROCEDURES Prior to first use all healthcare workers must be fit tested by Occupational Health and/or designate. FILTER ASSEMBLY INSTRUCTIONS 1. Align opening of cartridge/filter with filter attachment on facepiece. The alignment mark on the cartridge/filter should face the front of the facepiece. 2. Turn cartridge/filter clockwise one quarter until it is firmly seated and cannot be further turned. 3. Repeat for second filter. DONNING THE HALF-MASK (STANDARD SUSPENSION) 1. Perform hand hygiene. 2. Inspect the respirator to ensure it is in proper operating condition (not cracked, damaged, flaps are not torn or missing, straps not damaged, etc.). Jan. 4, 2021 COVID-19 Reusing and Disinfection of Elastomeric Respirators (half face respirator) 1 Adapted from McGill University Health Centre 3. Replace any damaged or defectives parts before use. 4. Adjust head cradle size as needed to fit comfortably on head. -

EBOLA VIRUS DISEASE Essential Information for Workers
New York Committee for Occupational Safety and Health 61 Broadway Suite 1710, New York, NY 10006 email: [email protected] (212) 227-6440 fax: (212) 227-9854 website: www.nycosh.org Long Island office: NYSUT, 150 Motor Parkway, Suite 306, Hauppauge, NY 11788 (631) 435-1857 fax: (631) 231-4523 EBOLA VIRUS DISEASE Essential Information for Workers (Current as of October 27, 2014) What is Ebola? How does Ebola virus spread? Government and medical experts agree that Ebola virus is Ebola virus disease (EVD), also known as Ebola hemorrhagic spread by direct contact with an infectious SHUVRQ¶V skin, fever (EHF), is a usually fatal disease that can affect blood, or body fluids such as urine, saliva, sweat, feces, humans and some animals. It is caused by infection with the vomit, breast milk, or semen. (Body fluids may contain blood Ebola virus. The first case of Ebola in the U.S. was even if blood is not visible.) Ebola infection may occur via confirmed in September 2014. The first case of transmission liquid contact, splash contact, droplet contact, or hand of Ebola to a health care worker in the U.S. was confirmed in contact with your mouth or nose, with the mucous October 2014. membranes of the eye or eyelid, with punctures on the skin (scabs, scrapes, cuts, injections, etc.) or through sexual acts. Because the virus can survive on surfaces for several How dangerous is Ebola? days, people can also be infected by direct contact with Fifty to ninety per cent objects (like needles or bed sheets) that contain infectious of patients with Ebola blood or body fluids. -
COVID-19 O2 and Bag Guidelines Updated 4 14
Boston Medical Center Page: 1 COVID-19 Respiratory Guidelines Airway and Oxygenation Guidelines for Persons Under Investigation (PUI) or Confirmed Positive for COVID-19 ______________________________________________________________________________ Purpose: This interim guidance is for respiratory therapists and other healthcare staff caring for patients with confirmed infection with COVID 19, as well as persons under investigation for COVID-19 and is specific to that patient population only. Clinical Guidelines 1. Use of aerosol generating procedures: a. The use of aerosol generating procedures has been shown to significantly increase the risk of transmission of the virus via aerosolized particles and should therefore be limited or avoided where possible. When use of these procedures is unavoidable, airborne and contact precautions are required. This includes an N-95 respirator or PAPR, mask with visor, gown, hairnet and gloves x2. Aerosol generating procedures include the following: Mechanical ventilation • The use of active humidification is not advised. Ventilators will be set up using a dry circuit with a heat and moisture exchanger (HME) in line and a bacterial and viral filter placed at the exhalation valve. The HME must be changed every 3-4 days or as needed. Bacterial and viral filters should be changed every 4 hours, or earlier as needed. Respiratory Care Boston Medical Center Page: 2 COVID-19 Respiratory Guidelines • If the patient’s ventilatory requirements exceed the capability of an HME, active humidity must be used, keeping the bacterial and viral filter on the exhalation valve. Due to the effect of the additional moisture on the filter, it must be changed every 4 hours or as needed. -
(PPE) When Caring for Patients with Confirmed Or Suspected COVID-19
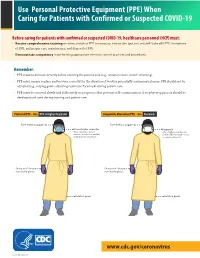
Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19 Before caring for patients with confirmed or suspected COVID-19, healthcare personnel (HCP) must: • Receive comprehensive training on when and what PPE is necessary, how to don (put on) and doff (take off) PPE, limitations of PPE, and proper care, maintenance, and disposal of PPE. • Demonstrate competency in performing appropriate infection control practices and procedures. Remember: • PPE must be donned correctly before entering the patient area (e.g., isolation room, unit if cohorting). • PPE must remain in place and be worn correctly for the duration of work in potentially contaminated areas. PPE should not be adjusted (e.g., retying gown, adjusting respirator/facemask) during patient care. • PPE must be removed slowly and deliberately in a sequence that prevents self-contamination. A step-by-step process should be COVID-19developed and Personal used during Protective training and patientEquipment care. COVID-19 Personal Protective Equipment (PPE) for Healthcare Personnel (PPE) for Healthcare Personnel Preferred PPE – Use N95 or Higher Respirator Acceptable Alternative PPE – Use Facemask Face shield or goggles Face shield or goggles N95 or higher respirator Facemask When respirators are not N95 or higher respirators are available, use the best available preferred but facemasks are an alternative, like a facemask. acceptable alternative. One pair of clean, One pair of clean, non-sterile gloves non-sterile gloves Isolation gown Isolation gown cdc.gov/COVID19 cdc.gov/COVID19 CS 315838-A 03/20/2020 CS 315838-B 03/20/2020 www.cdc.gov/coronavirus CS 316124-A 06/03/2020 Donning (putting on the gear): More than one donning method may be acceptable. -

COVID-19 Respiratory Guidelines 1 Airway and Oxygenation Guidelines for Persons Under Investigation (PUI) Or Confirmed Posi
COVID-19 Respiratory Guidelines 1 Airway and Oxygenation Guidelines for Persons Under Investigation (PUI) or Confirmed Positive for COVID-19 4/14/2020 Purpose: This interim guidance is for respiratory therapists and other healthcare staff caring for patients with confirmed infection with COVID 19, as well as persons under investigation for COVID-19 and is specific to that patient population only. Clinical Guidelines: 1. Use of aerosol generating procedures: a. The use of aerosol generating procedures has been shown to significantly increase the risk of transmission of the virus via aerosolized particles and should therefore be limited or avoided where possible. When use of these procedures is unavoidable, airborne and contact precautions are required. This includes an N-95 respirator or PAPR, mask with visor, gown, hairnet and gloves x2. Aerosol generating procedures include the following: Mechanical ventilation a. The use of active humidification is not advised. Ventilators will be set up using a dry circuit with a heat and moisture exchanger (HME) in line and a bacterial and viral filter placed at the exhalation valve. The HME must be changed every 3-4 days or as needed. Bacterial and viral filters should be changed every 4 hours, or earlier as needed. b. If the patient’s ventilatory requirements exceed the capability of an HME, active humidity must be used, keeping the bacterial and viral filter on the exhalation valve. Due to the effect of the additional moisture on the filter, it must be changed every 4 hours or as needed. Oxygen administration a. The following items are ok to use on this patient population: o Nasal cannula, with or without pendant, flows up to 15 lpm. -
Guidance for the Selection and Use of PPE in the Healthcare Setting
Guidance for the Selection and Use of Personal Protective Equipment (PPE) in Healthcare Settings 1 PPE Use in Healthcare Settings: Program Goal Improve personnel safety in the healthcare environment through appropriate use of PPE. PPE Use in Healthcare Settings The goal of this program is to improve personnel safety in the healthcare environment through appropriate use of PPE. 2 PPE Use in Healthcare Settings: Program Objectives • Provide information on the selection and use of PPE in healthcare settings • Practice how to safely don and remove PPE PPE Use in Healthcare Settings The objectives of this program are to provide information on the selection and use of PPE in healthcare settings and to allow time for participants to practice the correct way to don and remove PPE. 3 Personal Protective Equipment Definition “specialized clothing or equipment worn by an employee for protection against infectious materials” (OSHA) PPE Use in Healthcare Settings Personal protective equipment, or PPE, as defined by the Occupational Safety and Health Administration, or OSHA, is “specialized clothing or equipment, worn by an employee for protection against infectious materials.” 4 Regulations and Recommendations for PPE • OSHA issues workplace health and safety regulations. Regarding PPE, employers must: – Provide appropriate PPE for employees – Ensure that PPE is disposed or reusable PPE is cleaned, laundered, repaired and stored after use • OSHA also specifies circumstances for which PPE is indicated • CDC recommends when, what and how to use PPE PPE Use in Healthcare Settings OSHA issues regulations for workplace health and safety. These regulations require use of PPE in healthcare settings to protect healthcare personnel from exposure to bloodborne pathogens and Mycobacterium tuberculosis. -
Mouthbit Respirators
Mouthbit Respirators 7900 SERIES MOUTHBIT RESPIRATORS 7902 7904 North 7900 Series mouthbit respirators offer a quick and economical method to escape non-IDLH emergency situations. Use the respirator as a “visitors escape device” or issue individual respirators to employees as a safety precaution against a potential chemical leak. Model 7902 acid gas mouthbit is designed for emergency use at pulp and paper mills, water treatment plants, pools and spas, chemical plants and other facilities that may have accidental exposure to chlorine, chlorine dioxide, sulfur dioxide or hydrogen sulfide. Model 7902 ammonia mouthbit is designed for emergency use where ammonia may be used, such as refrigeration. 79BAG FEATURE FUNCTION BENEFIT Silicone mouthpiece • Softer and more pliable • More comfortable to wear for longer periods when the • No latex allergens escape route may be several minutes • Hypoallergenic Mouthpiece has a wider opening • More natural feel • No need to bite down or grip hard to hold the respirator in place Soft textured mouthpiece • Will not slip • More secure grip Mouthpiece is removable • Facilitates periodic cleaning of mouthpiece, such as after • Uses feel more comfortable knowing the mouthpiece training or when dispensed to Facility visitors has been sanitized Large, soft and flexible nose pads • Stays firmly on the nose without pressure • More secure are held on a balanced spring • Holds firmly without pinching • More comfortable Wider nose clip • Fits a variety of facial types • Fits most, if not all of your workers – know -

GUIDE to INFECTION CONTROL in the HOSPITAL Ebola Virus Disease
GUIDE TO INFECTION CONTROL IN THE HOSPITAL CHAPTER 61: Ebola Virus Disease Author S. Mehtar, MBBS, FRCPath, FCPath, MD Chapter Editor Gonzalo Bearman MD, MPH, FACP, FSHEA, FIDSA Topic Outline Key Issues Known Facts Suggested Practice General Principles Personal Protective Equipment for Healthcare Worker Personal Protective Equipment for Trained Observer Donning and Doffing Disinfection Healthcare Waste Management Suggested Practice in Under-Resourced Settings Summary Helpful Resources References Chapter last updated: February, 2018 KEY ISSUE The 2014 Ebola epidemic was the largest in history with 28,616 cases and 11,310 deaths recorded up to September 2016. There was widespread person-to-person transmission in multiple countries in West Africa, particularly affecting Guinea, Liberia, and Sierra Leone, but also Nigeria. Several countries in Europe and the United States received patients and healthcare workers who became infected with Ebola and were transported home for care. KNOWN FACTS • Ebola virus disease, previously known as Ebola hemorrhagic fever, is an uncommon and deadly disease caused by infection with a virus of the family Filoviridae, genus Ebolavirus. There are four identified Ebola virus species (Zaire, Sudan, Bundibugyo, and Tai Forest Ebola viruses) that cause disease in humans, Zaire being the most common and virulent and responsible for most of the outbreaks. • Ebola viruses are found in several West African countries. The first Ebola virus was discovered in 1976 near the Ebola River in what is now the Democratic Republic of the Congo. A second outbreak in Sudan occurred simultaneously. Since then, over 20 outbreaks have appeared sporadically in Africa but most of them were confined in rural forested areas. -

Tight-Fitting N95 Respirator Mask Training 8-12-20
Tight-fitting N95 Respirator Mask Training N95 Tight-fitting Respirator Mask Use Use during direct care activities that pose risk of exposure to airborne illness Use during Aerosol Generating Procedure (AGP) for coronavirus (COVID-19) positive, presumed-positive, and Person(s) Under investigation (PUI) Use during direct care of individual(s) coronavirus (COVID-19) positive, presumed-positive, and Person(s) Under investigation (PUI) when supply is plenty Employer Responsibilities Institute a respiratory protection plan that is readily available. Provide employees with medical evaluation and fit testing for N95 respirator masks Provide NIOSH and/or FDA approved N95 respirator mask as personal protective equipment (PPE) for employees involved in direct care that N95 may be needed Implement CDC and DDS guidance for optimizing PPE Provide training on use of N95 respirator mask use to employees Employee Responsibilities Participate in fit testing Remove facial hair prior to fit testing Obtain Medical evaluation (May be done at time of fit test my medical provider Understand N95 use Perform user seal check after donning N95 respirator mask Seek answers to any questions related to N95 use N95- Medical Evaluation Questionnaire filled out by a licensed healthcare provider giving clearance for the employee to wear an N95 respirator mask This must be completed prior to N95 fit testing If not approved for N95 mask use, report to management and Human Resources CDC FAQ regarding Medical Evaluation- https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/resps ource3medical.html#medicala Fit testing All N95 respirator mask wearers require fit testing for initial use of N95 respirator. -

Personal Protective Equipment for Use in a Filovirus Disease Outbreak
Personal protective equipment for use in a filovirus disease outbreak Rapid advice guideline Personal protective equipment for use in a filovirus disease outbreak Rapid advice guideline WHO Library Cataloguing-in-Publication Data Personal protective equipment for use in a filovirus disease outbreak: Rapid advice guideline. I.World Health Organization. ISBN 978 92 4 154972 1 Subject headings are available from WHO institutional repository © World Health Organization 2016 All rights reserved. Publications of the World Health Organization are available on the WHO website (http://www. who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (http://www.who.int/about/licensing/ copyright_form/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned.