Balancing the Risk – Strategies for Respiratory Protection During a Pandemic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Respirator on / Respirator Off
Respirator On / Respirator Off When you put on a disposable respirator Position your respirator correctly and check the seal to protect yourself from COVID-19. Cup the respirator in your hand. Place your fingertips from both Place both hands over the Select other PPE items that do not Hold the respirator under your hands at the top of the metal respirator, take a quick breath in interfere with the fit or chin with the nose piece up. The nose clip (if present). Slide to check the seal. Breathe out. If performance of your respirator. top strap (on single or double fingertips down both sides of you feel a leak when breathing strap respirators) goes over the metal strip to mold the nose in or breathing out, there is not and rests at the top back of area to the shape of your nose. a proper seal. your head. The bottom strap is positioned around the neck and below the ears. X X X X X Do not use a respirator that Do not allow facial hair, jewelry, Do not crisscross the straps. Do not wear a respirator that Do not touch the front of the appears damaged or deformed, glasses, clothing, or anything does not have a proper seal. If respirator during or after use! no longer forms an effective else to prevent proper placement air leaks in or out, ask for help It may be contaminated. seal to the face, becomes wet or to come between your face or try a different size or model. or visibly dirty, or if breathing and the respirator. -

COVID-19 Guidance on the Reuse of Elastomeric (Half Mask) Respirators
COVID-19 Guidance on the Reuse of Elastomeric (Half Mask) Respirators This guidance is adapted for use in Manitoba from materials developed by McGill University Health Centre. CONTEXT Reusable respirators (specifically, reusable half-facepiece elastomeric respirators) are the standard respiratory protection device used in many industries and in certain healthcare settings and facilities. The durability and reusability of elastomeric respirators make them desirable for stockpiling for emergencies, where the need for large volumes of respirators can be anticipated. MATERIAL Elastomeric Half-Facepiece Respirators (EHFR) (see annex 1 to compare with other masks/respirators) are half-face, tight-fitting respirators made of synthetic or rubber material. These materials permit them to be repeatedly disinfected, cleaned, and reused. PROCEDURES Prior to first use all healthcare workers must be fit tested by Occupational Health and/or designate. FILTER ASSEMBLY INSTRUCTIONS 1. Align opening of cartridge/filter with filter attachment on facepiece. The alignment mark on the cartridge/filter should face the front of the facepiece. 2. Turn cartridge/filter clockwise one quarter until it is firmly seated and cannot be further turned. 3. Repeat for second filter. DONNING THE HALF-MASK (STANDARD SUSPENSION) 1. Perform hand hygiene. 2. Inspect the respirator to ensure it is in proper operating condition (not cracked, damaged, flaps are not torn or missing, straps not damaged, etc.). Jan. 4, 2021 COVID-19 Reusing and Disinfection of Elastomeric Respirators (half face respirator) 1 Adapted from McGill University Health Centre 3. Replace any damaged or defectives parts before use. 4. Adjust head cradle size as needed to fit comfortably on head. -
COVID-19 O2 and Bag Guidelines Updated 4 14
Boston Medical Center Page: 1 COVID-19 Respiratory Guidelines Airway and Oxygenation Guidelines for Persons Under Investigation (PUI) or Confirmed Positive for COVID-19 ______________________________________________________________________________ Purpose: This interim guidance is for respiratory therapists and other healthcare staff caring for patients with confirmed infection with COVID 19, as well as persons under investigation for COVID-19 and is specific to that patient population only. Clinical Guidelines 1. Use of aerosol generating procedures: a. The use of aerosol generating procedures has been shown to significantly increase the risk of transmission of the virus via aerosolized particles and should therefore be limited or avoided where possible. When use of these procedures is unavoidable, airborne and contact precautions are required. This includes an N-95 respirator or PAPR, mask with visor, gown, hairnet and gloves x2. Aerosol generating procedures include the following: Mechanical ventilation • The use of active humidification is not advised. Ventilators will be set up using a dry circuit with a heat and moisture exchanger (HME) in line and a bacterial and viral filter placed at the exhalation valve. The HME must be changed every 3-4 days or as needed. Bacterial and viral filters should be changed every 4 hours, or earlier as needed. Respiratory Care Boston Medical Center Page: 2 COVID-19 Respiratory Guidelines • If the patient’s ventilatory requirements exceed the capability of an HME, active humidity must be used, keeping the bacterial and viral filter on the exhalation valve. Due to the effect of the additional moisture on the filter, it must be changed every 4 hours or as needed. -
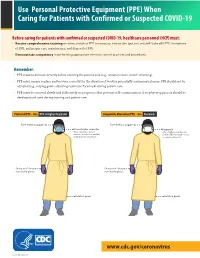
(PPE) When Caring for Patients with Confirmed Or Suspected COVID-19
Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19 Before caring for patients with confirmed or suspected COVID-19, healthcare personnel (HCP) must: • Receive comprehensive training on when and what PPE is necessary, how to don (put on) and doff (take off) PPE, limitations of PPE, and proper care, maintenance, and disposal of PPE. • Demonstrate competency in performing appropriate infection control practices and procedures. Remember: • PPE must be donned correctly before entering the patient area (e.g., isolation room, unit if cohorting). • PPE must remain in place and be worn correctly for the duration of work in potentially contaminated areas. PPE should not be adjusted (e.g., retying gown, adjusting respirator/facemask) during patient care. • PPE must be removed slowly and deliberately in a sequence that prevents self-contamination. A step-by-step process should be COVID-19developed and Personal used during Protective training and patientEquipment care. COVID-19 Personal Protective Equipment (PPE) for Healthcare Personnel (PPE) for Healthcare Personnel Preferred PPE – Use N95 or Higher Respirator Acceptable Alternative PPE – Use Facemask Face shield or goggles Face shield or goggles N95 or higher respirator Facemask When respirators are not N95 or higher respirators are available, use the best available preferred but facemasks are an alternative, like a facemask. acceptable alternative. One pair of clean, One pair of clean, non-sterile gloves non-sterile gloves Isolation gown Isolation gown cdc.gov/COVID19 cdc.gov/COVID19 CS 315838-A 03/20/2020 CS 315838-B 03/20/2020 www.cdc.gov/coronavirus CS 316124-A 06/03/2020 Donning (putting on the gear): More than one donning method may be acceptable. -

COVID-19 Respiratory Guidelines 1 Airway and Oxygenation Guidelines for Persons Under Investigation (PUI) Or Confirmed Posi
COVID-19 Respiratory Guidelines 1 Airway and Oxygenation Guidelines for Persons Under Investigation (PUI) or Confirmed Positive for COVID-19 4/14/2020 Purpose: This interim guidance is for respiratory therapists and other healthcare staff caring for patients with confirmed infection with COVID 19, as well as persons under investigation for COVID-19 and is specific to that patient population only. Clinical Guidelines: 1. Use of aerosol generating procedures: a. The use of aerosol generating procedures has been shown to significantly increase the risk of transmission of the virus via aerosolized particles and should therefore be limited or avoided where possible. When use of these procedures is unavoidable, airborne and contact precautions are required. This includes an N-95 respirator or PAPR, mask with visor, gown, hairnet and gloves x2. Aerosol generating procedures include the following: Mechanical ventilation a. The use of active humidification is not advised. Ventilators will be set up using a dry circuit with a heat and moisture exchanger (HME) in line and a bacterial and viral filter placed at the exhalation valve. The HME must be changed every 3-4 days or as needed. Bacterial and viral filters should be changed every 4 hours, or earlier as needed. b. If the patient’s ventilatory requirements exceed the capability of an HME, active humidity must be used, keeping the bacterial and viral filter on the exhalation valve. Due to the effect of the additional moisture on the filter, it must be changed every 4 hours or as needed. Oxygen administration a. The following items are ok to use on this patient population: o Nasal cannula, with or without pendant, flows up to 15 lpm. -
Guidance for the Selection and Use of PPE in the Healthcare Setting
Guidance for the Selection and Use of Personal Protective Equipment (PPE) in Healthcare Settings 1 PPE Use in Healthcare Settings: Program Goal Improve personnel safety in the healthcare environment through appropriate use of PPE. PPE Use in Healthcare Settings The goal of this program is to improve personnel safety in the healthcare environment through appropriate use of PPE. 2 PPE Use in Healthcare Settings: Program Objectives • Provide information on the selection and use of PPE in healthcare settings • Practice how to safely don and remove PPE PPE Use in Healthcare Settings The objectives of this program are to provide information on the selection and use of PPE in healthcare settings and to allow time for participants to practice the correct way to don and remove PPE. 3 Personal Protective Equipment Definition “specialized clothing or equipment worn by an employee for protection against infectious materials” (OSHA) PPE Use in Healthcare Settings Personal protective equipment, or PPE, as defined by the Occupational Safety and Health Administration, or OSHA, is “specialized clothing or equipment, worn by an employee for protection against infectious materials.” 4 Regulations and Recommendations for PPE • OSHA issues workplace health and safety regulations. Regarding PPE, employers must: – Provide appropriate PPE for employees – Ensure that PPE is disposed or reusable PPE is cleaned, laundered, repaired and stored after use • OSHA also specifies circumstances for which PPE is indicated • CDC recommends when, what and how to use PPE PPE Use in Healthcare Settings OSHA issues regulations for workplace health and safety. These regulations require use of PPE in healthcare settings to protect healthcare personnel from exposure to bloodborne pathogens and Mycobacterium tuberculosis. -
Mouthbit Respirators
Mouthbit Respirators 7900 SERIES MOUTHBIT RESPIRATORS 7902 7904 North 7900 Series mouthbit respirators offer a quick and economical method to escape non-IDLH emergency situations. Use the respirator as a “visitors escape device” or issue individual respirators to employees as a safety precaution against a potential chemical leak. Model 7902 acid gas mouthbit is designed for emergency use at pulp and paper mills, water treatment plants, pools and spas, chemical plants and other facilities that may have accidental exposure to chlorine, chlorine dioxide, sulfur dioxide or hydrogen sulfide. Model 7902 ammonia mouthbit is designed for emergency use where ammonia may be used, such as refrigeration. 79BAG FEATURE FUNCTION BENEFIT Silicone mouthpiece • Softer and more pliable • More comfortable to wear for longer periods when the • No latex allergens escape route may be several minutes • Hypoallergenic Mouthpiece has a wider opening • More natural feel • No need to bite down or grip hard to hold the respirator in place Soft textured mouthpiece • Will not slip • More secure grip Mouthpiece is removable • Facilitates periodic cleaning of mouthpiece, such as after • Uses feel more comfortable knowing the mouthpiece training or when dispensed to Facility visitors has been sanitized Large, soft and flexible nose pads • Stays firmly on the nose without pressure • More secure are held on a balanced spring • Holds firmly without pinching • More comfortable Wider nose clip • Fits a variety of facial types • Fits most, if not all of your workers – know -

How to Use Personal Protective Equipment: a Quick Reference Guide for Frontline Clinical Providers
How to Use Personal Protective Equipment: A Quick Reference Guide for Frontline Clinical Providers Frontline clinical providers should wear the following personal protective equipment (PPE) when treating individuals confirmed or suspected to be infected with COVID-19. N95 RESPIRATOR GOWN GLOVES FACE SHIELD/ EYE PROTECTION How to properly use protective equipment PPE TYPE DONNING PPE REMOVING PPE • Secure ties or elastic band at middle of • Front of respirator is contaminated – N95 RESPIRATOR head and neck DO NOT TOUCH! • Fit flexible band to nose bridge • Grasp ONLY bottom then top ties/elastics (AS AVAILABLE) • Fit snug to face and below chin and remove • Fit-check respirator • Discard in waste container • Gown front and sleeves are contaminated! • Unfasten neck, then waist ties • Remove gown using a peeling motion; • Fully cover torso from neck to knees, arms pull gown from each shoulder toward the GOWN to end of wrist, and wrap around the back same hand • Fasten in back at neck and waist • Gown will turn inside out • Hold removed gown away from body, roll into a bundle and discard into waste or linen receptacle • Outside of gloves are contaminated! • Grasp outside of glove with opposite • U se non-sterile for isolation gloved hand; peel off GLOVES Select according to hand size • • Hold removed glove in gloved hand • Extend to cover wrist of isolation gown • Slide fingers of ungloved hand under remaining glove at wrist • Outside of goggles or face shield are contaminated! FACE SHIELD / • Put on face and adjust to fit • To remove, handle by “clean” head band EYE PROTECTION or ear pieces • Place in designated receptacle for reprocessing or in waste container Wash hands or use an alcohol-based hand sanitizer immediately after removing all PPE! N95 Respirator Usage and Care N95 respirators must only be used by a single wearer. -

Choosing the Best Escape Respirator for Your Emergency Response Plan
Choosing the Best Escape Respirator for Your Emergency Response Plan Many industrial disasters have resulted from a false sense of security in SOPs and fail-safes. 2 1 0 2 - 6 3 0 7 5 - D THE THREE-LEGGED STOOL OF 3. Emergency response plan: Protect Acquiring the correct type and quantity of HAZARDOUS MATERIAL RISK MANAGEMENT plant and human assets by providing a escape respirators is just as much a part According to OSHA's 29 CFR 1910.110 means of escape/response in the event of risk management as trying to prevent Appendix C (Compliance Guidelines and legs 1 and 2 fail. Depending on the risk the release of the hazard in the first place. Recommendations for Process Safety and hazard, this can range from a Management), personnel working with any simple evacuation plan to a complex PERFORMING A PROCESS HAZARD hazardous process should be protected emergency response scenario including ANALYSIS by at least three lines of defense. These escape respirators, escape refuge If you're interested in strengthening the lines of defense must operate in unison to chambers/ safe zones, hazmat (or fire) third leg of your organizations hazardous provide an effective hazard control plan. control teams, and search and-rescue material risk management plan, the first You can think of this approach as the procedures. step is to perform a process hazard analysis "three-legged stool" of hazardous material (PHA) to make sure you understand the risk management, which includes the If these three elements are not operating risks in the workplace and the conse - following three lines of defense or legs: together, then the likelihood of a disaster quences that will result if your SOPs and or fatality is exponentially higher. -

OSHA's Respiratory Protection Standard 29 CFR 1910.134
OSHA’s Respiratory Protection Standard 29 CFR 1910.134 This program is intended to be a resource for instructors of occupational safety and health and is not a substitute for any of the provisions of the Occupational Safety and Health Act of 1970 or for any standards issued by the U.S. Department of Labor’s Occupational Safety and Health Administration (OSHA). OSHA’s Office of Training and Education wishes to acknowledge 3M Occupational Health and Safety Division, MSA, North Safety Products and TSI for contributing some of the graphics used in this program. Appearance of their products does not imply endorsement by the U.S. Department of Labor. Scope This standard applies to: • General Industry (Part 1910), • Shipyards (Part 1915), • Marine Terminals (Part 1917), • Longshoring (Part 1918), and • Construction (Part 1926). Organization of Standard (a) Permissible practice (k) Training and information (b) Definitions (l) Program evaluation (c) Respirator program (m) Recordkeeping (d) Selection of respirators (n) Dates (e) Medical evaluation (o) Appendices (mandatory) (f) Fit testing A: Fit Testing Procedures (g) Use of respirators B-1: User Seal Checks (h) Maintenance and care B-2: Cleaning Procedures (i) Breathing air quality and use C: Medical Questionnaire (j) Identification of filters, cartridges, D: Information for Employees and canisters Wearing Respirators When Not Required Under the Standard Permissible Practice • The primary means to control occupational diseases caused by breathing contaminated air is through the use of feasible -

Respiratory Protection
Respiratory Protection The Occupational Safety and Health Administration (OSHA) construction industry regulations relating to respiratory protection (29 CFR 1926.103) are actually found under the general industry regulations applicable to respiratory protection in 29 CFR 1910.134. Those provisions mandate respiratory protection if engineering controls are not feasible or are ineffective. OSHA requires methods such as substituting less toxic materials or ventilating the work area to prevent atmospheric contamination. When engineering controls fail to reduce employee exposures to harmful contaminants below the permissible exposure limit (PEL) of a contaminant, respiratory protection and accompanying program elements must be put in place. Written Respiratory Protection Program The OSHA respiratory standard requires contractors to develop and implement a written respiratory protection program for situations in which PELs of airborne contaminants could be exceeded or when the employer requires use of respirators by workers. See also the chapter on Confined Spaces. The written program also must address voluntary respirator use; respirator selection; medical evaluations; fit-testing; use of respirators; user seal checks; maintenance and care of respirators; identification of filters, cartridges and canisters; employee training; and program evaluation. The standard requires the respiratory program to be administered by a program administrator and updated to reflect the changing workplace conditions that affect respirator use. The standard sets out several mandatory components within the aforementioned program categories including fit testing, seal-check and cleaning procedures in addition to a medical evaluation questionnaire and voluntary-use procedures that are compiled in appendices to §1910.134. Many of the elements listed may not need to change for each project. -

YNHHS/YM PPE Policy for COVID-19 Prevention
YNHHS/YM PPE Policy for COVID-19 Prevention Note: This supersedes other COVID-19 respiratory protection and PPE policies, including SBARs. Effective date: March 1, 2021 Background: The proper use of personal protective equipment (PPE) in conjunction with infection prevention behaviors such as physical barriers, social distancing and hand hygiene prevents the transmission of COVID-19. Scope: These guidelines apply to all settings. This PPE policy does not provide comprehensive guidance for COVID testing or patient/work flows to ensure social distancing. Definitions: Cloth Mask—Any mask constructed from textiles or fabrics which covers the mouth and nose and is intended to limit the spread of respiratory secretions. For the purposes of this policy, gaiters, bandanas and cloth masks with exhalation valves are not included as their level of protection is low. Face mask – A facility-provided mask that is well fitted and cover both mouth and nose. Face masks with exhalation valves are not included in this definition for the purpose of this policy. Surgical mask – A commercially produced face mask regulated by the FDA for performing surgical procedures. These masks provide fluid resistance and have ASTM ratings of 2 or 3. Respirator – A facility-provided device which snugly covers both mouth and nose, with a filtration level of at least 95% of particulate materials. These include N95 respirators, elastomeric respirators, PAPRs, and CAPRs. N95 Respirator – A facility-provided disposable respirator that has a filtration level of 95% of particulate materials. Elastomeric Respirator – A facility-provided reusable respirator which has replaceable filters, cartridges, and/or canisters and a filtration level of at least 95%.