Genetics and Functions of Herpes Simplex Virus Type-1 Membrane
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Novel 2-Herpesvirus of the Rhadinovirus 2 Lineage In
Downloaded from genome.cshlp.org on September 29, 2021 - Published by Cold Spring Harbor Laboratory Press Letter A Novel ␥2-Herpesvirus of the Rhadinovirus 2 Lineage in Chimpanzees Vincent Lacoste,1 Philippe Mauclère,1,2 Guy Dubreuil,3 John Lewis,4 Marie-Claude Georges-Courbot,3 andAntoine Gessain 1,5 1Unite´d’Epide´miologie et Physiopathologie des Virus Oncoge`nes, De´partement du SIDA et des Re´trovirus, Institut Pasteur, 75724 Paris Cedex 15, France; 2Centre Pasteur du Cameroun, BP 1274, Yaounde´, Cameroon; 3Centre International de Recherches Me´dicales, Franceville, Gabon; 4International Zoo Veterinary Group, Keighley, West Yorkshire BD21 1AG, UK Old World monkeys and, recently, African great apes have been shown, by serology and polymerase chain reaction (PCR), to harbor different ␥2-herpesviruses closely related to Kaposi’s sarcoma-associated Herpesvirus (KSHV). Although the presence of two distinct lineages of KSHV-like rhadinoviruses, RV1 and RV2, has been revealed in Old World primates (including African green monkeys, macaques, and, recently, mandrills), viruses belonging to the RV2 genogroup have not yet been identified from great apes. Indeed, the three yet known ␥2-herpesviruses in chimpanzees (PanRHV1a/PtRV1, PanRHV1b) and gorillas (GorRHV1) belong to the RV1 group. To investigate the putative existence of a new RV2 Rhadinovirus in chimpanzees and gorillas we have used the degenerate consensus primer PCR strategy for the Herpesviral DNA polymerase gene on 40 wild-caught animals. This study led to the discovery, in common chimpanzees, of a novel ␥2-herpesvirus belonging to the RV2 genogroup, termed Pan Rhadino-herpesvirus 2 (PanRHV2). Use of specific primers and internal oligonucleotide probes demonstrated the presence of this novel ␥2-herpesvirus in three wild-caught animals. -

Journal of Virology
JOURNAL OF VIROLOGY Volume 80 March 2006 No. 6 SPOTLIGHT Articles of Significant Interest Selected from This Issue by 2587–2588 the Editors STRUCTURE AND ASSEMBLY Crystal Structure of the Oligomerization Domain of the Haitao Ding, Todd J. Green, 2808–2814 Phosphoprotein of Vesicular Stomatitis Virus Shanyun Lu, and Ming Luo Subcellular Localization of Hepatitis C Virus Structural Yves Rouille´, Franc¸ois Helle, David 2832–2841 Proteins in a Cell Culture System That Efficiently Replicates Delgrange, Philippe Roingeard, the Virus Ce´cile Voisset, Emmanuelle Blanchard, Sandrine Belouzard, Jane McKeating, Arvind H. Patel, Geert Maertens, Takaji Wakita, Czeslaw Wychowski, and Jean Dubuisson A Small Loop in the Capsid Protein of Moloney Murine Marcy R. Auerbach, Kristy R. 2884–2893 Leukemia Virus Controls Assembly of Spherical Cores Brown, Artem Kaplan, Denise de Las Nueces, and Ila R. Singh Identification of the Nucleocapsid, Tegument, and Envelope Jyh-Ming Tsai, Han-Ching Wang, 3021–3029 Proteins of the Shrimp White Spot Syndrome Virus Virion Jiann-Horng Leu, Andrew H.-J. Wang, Ying Zhuang, Peter J. Walker, Guang-Hsiung Kou, and Chu-Fang Lo GENOME REPLICATION AND REGULATION OF VIRAL GENE EXPRESSION Epitope Mapping of Herpes Simplex Virus Type 2 gH/gL Tina M. Cairns, Marie S. Shaner, Yi 2596–2608 Defines Distinct Antigenic Sites, Including Some Associated Zuo, Manuel Ponce-de-Leon, with Biological Function Isabelle Baribaud, Roselyn J. Eisenberg, Gary H. Cohen, and J. Charles Whitbeck The ␣-TIF (VP16) Homologue (ETIF) of Equine Jens von Einem, Daniel 2609–2620 Herpesvirus 1 Is Essential for Secondary Envelopment Schumacher, Dennis J. O’Callaghan, and Virus Egress and Nikolaus Osterrieder Suppression of Viral RNA Recombination by a Host Chi-Ping Cheng, Elena Serviene, 2631–2640 Exoribonuclease and Peter D. -
HS and Product Codes
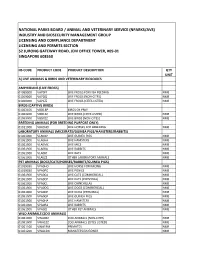
NATIONAL PARKS BOARD / ANIMAL AND VETERINARY SERVICE (NPARKS/AVS) INDUSTRY AND BIOSECURITY MANAGEMENT GROUP LICENSING AND COMPLIANCE DEPARTMENT LICENSING AND PERMITS SECTION 52 JURONG GATEWAY ROAD, JEM OFFICE TOWER, #09-01 SINGAPORE 608550 HS CODE PRODUCT CODE PRODUCT DESCRIPTION QTY UNIT A) LIVE ANIMALS & BIRDS AND VETERINARY BIOLOGICS AMPHIBIANS (LIVE FROGS) 01069000 VAP0FF LIVE FROGS FOR FISH FEEDING NMB 01069000 VAP0ZZ LIVE FROGS (NON-CITES) NMB 01069000 VAP1ZZ LIVE FROGS (CITES LISTED) NMB BIRDS (CAPTIVE BIRDS) 01063100 VBD1BP BIRDS OF PREY 01063200 VBD1ZZ LIVE BIRDS (CITES LISTED) NMB 01063900 VBD0ZZ LIVE BIRDS (NON-CITES) NMB BREEDING ANIMALS (FOR BREEDING PURPOSE ONLY) 01011000 VBA0HO LIVE HORSES FOR BREEDING NMB LABORATORY ANIMALS (MICE/RATS/GUINEA PIGS/HAMSTERS/RABBITS) 01061900 VLA0GP LIVE GUINEA PIGS NMB 01061900 VLA0HA LIVE HAMSTERS NMB 01061900 VLA0MC LIVE MICE NMB 01061900 VLA0RA LIVE RABBITS NMB 01061900 VLA0RT LIVE RATS NMB 01061900 VLA0ZZ OTHER LABORATORY ANIMALS NMB PET ANIMALS (DOGS/CATS/HORSES/RABBITS/GUINEA PIGS) 01019030 VPA0HO LIVE HORSE FOR RACING NMB 01019030 VPA0PO LIVE PONIES NMB 01061900 VPA0CA LIVE CATS (COMMERCIAL) NMB 01061900 VPA0CP LIVE CATS (PERSONAL) NMB 01061900 VPA0CL LIVE CHINCHILLAS NMB 01061900 VPA0DG LIVE DOGS (COMMERCIAL) NMB 01061900 VPA0DP LIVE DOGS (PERSONAL) NMB 01061900 VPA0GP LIVE GUINEA PIGS NMB 01061900 VPA0HA LIVE HAMSTERS NMB 01061900 VPA0RA LIVE RABBITS NMB 01061900 VPA0ZZ OTHER PET ANIMALS NMB WILD ANIMALS (ZOO ANIMALS) 01061900 VWA0ZZ ZOO ANIMALS (NON-CITES) NMB 01061900 VWA1ZZ ZOO ANIMALS (CITES LISTED) NMB 01061100 VWA1PM PRIMATES NMB 01061200 VWA1DG MANATEES/DUGONGS NMB 01061200 VWA1WD WHALES/DOLPHINS NMB VETERINARY VACCINES 30023000 VVC0ZZ VETERINARY VACCINE - VETERINARY BIOLOGICS 30029000 VVP0B0COWRUMB COWDRIA RUMINANTIUM - 30029000 VVP0B2AERHYDB AEROMONAS HYDROPHILA - 30029000 VVP0B2ANAMARB ANAPLASMA MARGINALE - 30029000 VVP0B2BORBURB BORRELIA BURGDORFERI - 30029000 VVP0B2CAMFETV CAMPYLOBACTER FETUS SUBSP. -

Viral Diversity Among Different Bat Species That Share a Common Habitatᰔ Eric F
JOURNAL OF VIROLOGY, Dec. 2010, p. 13004–13018 Vol. 84, No. 24 0022-538X/10/$12.00 doi:10.1128/JVI.01255-10 Copyright © 2010, American Society for Microbiology. All Rights Reserved. Metagenomic Analysis of the Viromes of Three North American Bat Species: Viral Diversity among Different Bat Species That Share a Common Habitatᰔ Eric F. Donaldson,1†* Aimee N. Haskew,2 J. Edward Gates,2† Jeremy Huynh,1 Clea J. Moore,3 and Matthew B. Frieman4† Department of Epidemiology, University of North Carolina, Chapel Hill, North Carolina 275991; University of Maryland Center for Environmental Science, Appalachian Laboratory, Frostburg, Maryland 215322; Department of Biological Sciences, Oakwood University, Huntsville, Alabama 358963; and Department of Microbiology and Immunology, University of Maryland at Baltimore, Baltimore, Maryland 212014 Received 11 June 2010/Accepted 24 September 2010 Effective prediction of future viral zoonoses requires an in-depth understanding of the heterologous viral population in key animal species that will likely serve as reservoir hosts or intermediates during the next viral epidemic. The importance of bats as natural hosts for several important viral zoonoses, including Ebola, Marburg, Nipah, Hendra, and rabies viruses and severe acute respiratory syndrome-coronavirus (SARS-CoV), has been established; however, the large viral population diversity (virome) of bats has been partially deter- mined for only a few of the ϳ1,200 bat species. To assess the virome of North American bats, we collected fecal, oral, urine, and tissue samples from individual bats captured at an abandoned railroad tunnel in Maryland that is cohabitated by 7 to 10 different bat species. Here, we present preliminary characterization of the virome of three common North American bat species, including big brown bats (Eptesicus fuscus), tricolored bats (Perimyotis subflavus), and little brown myotis (Myotis lucifugus). -

Virus Entry: What Has Ph Got to Do with It?
TURNING POINTS Virus entry: What has pH got to do with it? Ari Helenius After several years of working on membrane For almost two years, the virus entry path- Over the following months, we validated proteins using the Semliki Forest virus (SFV) as way and mechanism of host penetration con- all the predictions of our pH hypothesis. For a model, I decided in 1976 to focus my research tinued to elude us. However, in the spring example, we could demonstrate a membrane on the mechanisms by which animal viruses of 1978, I had the chance to participate in a fusion reaction in vitro by simply mixing such as SFV enter and infect their host cells. Dahlem Conference in Berlin called ‘Transport liposomes and SFV, and briefly dropping the pH I had just moved from Finland with the lab of of Macromolecules in Cellular Systems’. It was to 6 or below. Moreover, when we added acidic Kai Simons to the newly founded European an opportune time for a meeting on this topic: medium to cells, we could ‘fool’ surface-bound Molecular Biology Laboratory (EMBL) in pathways of vesicle transport were being dis- viruses into fusing with the plasma membrane; Heidelberg, Germany. I was eager to tackle a covered, receptor-mediated trafficking pro- the entry block caused by weak bases was challenging problem — and one that did not cesses were beginning to be described, and the bypassed and the cells became infected. require work with detergents. important role of clathrin-coated vesicles was Joined by Judy White, Mark Marsh and Relying almost exclusively on electron finally properly appreciated. -

2020 Taxonomic Update for Phylum Negarnaviricota (Riboviria: Orthornavirae), Including the Large Orders Bunyavirales and Mononegavirales
Archives of Virology https://doi.org/10.1007/s00705-020-04731-2 VIROLOGY DIVISION NEWS 2020 taxonomic update for phylum Negarnaviricota (Riboviria: Orthornavirae), including the large orders Bunyavirales and Mononegavirales Jens H. Kuhn1 · Scott Adkins2 · Daniela Alioto3 · Sergey V. Alkhovsky4 · Gaya K. Amarasinghe5 · Simon J. Anthony6,7 · Tatjana Avšič‑Županc8 · María A. Ayllón9,10 · Justin Bahl11 · Anne Balkema‑Buschmann12 · Matthew J. Ballinger13 · Tomáš Bartonička14 · Christopher Basler15 · Sina Bavari16 · Martin Beer17 · Dennis A. Bente18 · Éric Bergeron19 · Brian H. Bird20 · Carol Blair21 · Kim R. Blasdell22 · Steven B. Bradfute23 · Rachel Breyta24 · Thomas Briese25 · Paul A. Brown26 · Ursula J. Buchholz27 · Michael J. Buchmeier28 · Alexander Bukreyev18,29 · Felicity Burt30 · Nihal Buzkan31 · Charles H. Calisher32 · Mengji Cao33,34 · Inmaculada Casas35 · John Chamberlain36 · Kartik Chandran37 · Rémi N. Charrel38 · Biao Chen39 · Michela Chiumenti40 · Il‑Ryong Choi41 · J. Christopher S. Clegg42 · Ian Crozier43 · John V. da Graça44 · Elena Dal Bó45 · Alberto M. R. Dávila46 · Juan Carlos de la Torre47 · Xavier de Lamballerie38 · Rik L. de Swart48 · Patrick L. Di Bello49 · Nicholas Di Paola50 · Francesco Di Serio40 · Ralf G. Dietzgen51 · Michele Digiaro52 · Valerian V. Dolja53 · Olga Dolnik54 · Michael A. Drebot55 · Jan Felix Drexler56 · Ralf Dürrwald57 · Lucie Dufkova58 · William G. Dundon59 · W. Paul Duprex60 · John M. Dye50 · Andrew J. Easton61 · Hideki Ebihara62 · Toufc Elbeaino63 · Koray Ergünay64 · Jorlan Fernandes195 · Anthony R. Fooks65 · Pierre B. H. Formenty66 · Leonie F. Forth17 · Ron A. M. Fouchier48 · Juliana Freitas‑Astúa67 · Selma Gago‑Zachert68,69 · George Fú Gāo70 · María Laura García71 · Adolfo García‑Sastre72 · Aura R. Garrison50 · Aiah Gbakima73 · Tracey Goldstein74 · Jean‑Paul J. Gonzalez75,76 · Anthony Grifths77 · Martin H. Groschup12 · Stephan Günther78 · Alexandro Guterres195 · Roy A. -

A Persistent Giant Algal Virus, with a Unique Morphology, Encodes An
bioRxiv preprint doi: https://doi.org/10.1101/2020.07.30.228163; this version posted January 13, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 A persistent giant algal virus, with a unique morphology, encodes an 2 unprecedented number of genes involved in energy metabolism 3 4 Romain Blanc-Mathieu1,2, Håkon Dahle3, Antje Hofgaard4, David Brandt5, Hiroki 5 Ban1, Jörn Kalinowski5, Hiroyuki Ogata1 and Ruth-Anne Sandaa6* 6 7 1: Institute for Chemical Research, Kyoto University, Gokasho, Uji, 611-0011, Japan 8 2: Laboratoire de Physiologie Cellulaire & Végétale, CEA, Univ. Grenoble Alpes, 9 CNRS, INRA, IRIG, Grenoble, France 10 3: Department of Biological Sciences and K.G. Jebsen Center for Deep Sea Research, 11 University of Bergen, Bergen, Norway 12 4: Department of Biosciences, University of Oslo, Norway 13 5: Center for Biotechnology, Universität Bielefeld, Bielefeld, 33615, Germany 14 6: Department of Biological Sciences, University of Bergen, Bergen, Norway 15 *Corresponding author: Ruth-Anne Sandaa, +47 55584646, [email protected] 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.07.30.228163; this version posted January 13, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 16 Abstract 17 Viruses have long been viewed as entities possessing extremely limited metabolic 18 capacities. -

Formation of Influenza Virus Particles Lacking Hemagglutinin on the Viral Envelope Asit K
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Papers in Veterinary and Biomedical Science Veterinary and Biomedical Sciences, Department of 1986 Formation of Influenza Virus Particles Lacking Hemagglutinin on the Viral Envelope Asit K. Pattnaik University of Nebraska-Lincoln, [email protected] Donald J. Brown University of California at Los Angeles Debi P. Nayak University of California at Los Angeles Follow this and additional works at: http://digitalcommons.unl.edu/vetscipapers Part of the Biochemistry, Biophysics, and Structural Biology Commons, Cell and Developmental Biology Commons, Immunology and Infectious Disease Commons, Medical Sciences Commons, Veterinary Microbiology and Immunobiology Commons, and the Veterinary Pathology and Pathobiology Commons Pattnaik, Asit K.; Brown, Donald J.; and Nayak, Debi P., "Formation of Influenza Virus Particles Lacking Hemagglutinin on the Viral Envelope" (1986). Papers in Veterinary and Biomedical Science. 198. http://digitalcommons.unl.edu/vetscipapers/198 This Article is brought to you for free and open access by the Veterinary and Biomedical Sciences, Department of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Papers in Veterinary and Biomedical Science by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. JOURNAL OF VIROLOGY, Dec. 1986, p. 994-1001 Vol. 60, No.3 0022-S38X1861120994-08 $02.00/0 Copyright © 1986, American Society for Microbiology Formation of Influenza Virus Particles -

The LUCA and Its Complex Virome in Another Recent Synthesis, We Examined the Origins of the Replication and Structural Mart Krupovic , Valerian V
PERSPECTIVES archaea that form several distinct, seemingly unrelated groups16–18. The LUCA and its complex virome In another recent synthesis, we examined the origins of the replication and structural Mart Krupovic , Valerian V. Dolja and Eugene V. Koonin modules of viruses and posited a ‘chimeric’ scenario of virus evolution19. Under this Abstract | The last universal cellular ancestor (LUCA) is the most recent population model, the replication machineries of each of of organisms from which all cellular life on Earth descends. The reconstruction of the four realms derive from the primordial the genome and phenotype of the LUCA is a major challenge in evolutionary pool of genetic elements, whereas the major biology. Given that all life forms are associated with viruses and/or other mobile virion structural proteins were acquired genetic elements, there is no doubt that the LUCA was a host to viruses. Here, by from cellular hosts at different stages of evolution giving rise to bona fide viruses. projecting back in time using the extant distribution of viruses across the two In this Perspective article, we combine primary domains of life, bacteria and archaea, and tracing the evolutionary this recent work with observations on the histories of some key virus genes, we attempt a reconstruction of the LUCA virome. host ranges of viruses in each of the four Even a conservative version of this reconstruction suggests a remarkably complex realms, along with deeper reconstructions virome that already included the main groups of extant viruses of bacteria and of virus evolution, to tentatively infer archaea. We further present evidence of extensive virus evolution antedating the the composition of the virome of the last universal cellular ancestor (LUCA; also LUCA. -

Where Do We Stand After Decades of Studying Human Cytomegalovirus?
microorganisms Review Where do we Stand after Decades of Studying Human Cytomegalovirus? 1, 2, 1 1 Francesca Gugliesi y, Alessandra Coscia y, Gloria Griffante , Ganna Galitska , Selina Pasquero 1, Camilla Albano 1 and Matteo Biolatti 1,* 1 Laboratory of Pathogenesis of Viral Infections, Department of Public Health and Pediatric Sciences, University of Turin, 10126 Turin, Italy; [email protected] (F.G.); gloria.griff[email protected] (G.G.); [email protected] (G.G.); [email protected] (S.P.); [email protected] (C.A.) 2 Complex Structure Neonatology Unit, Department of Public Health and Pediatric Sciences, University of Turin, 10126 Turin, Italy; [email protected] * Correspondence: [email protected] These authors contributed equally to this work. y Received: 19 March 2020; Accepted: 5 May 2020; Published: 8 May 2020 Abstract: Human cytomegalovirus (HCMV), a linear double-stranded DNA betaherpesvirus belonging to the family of Herpesviridae, is characterized by widespread seroprevalence, ranging between 56% and 94%, strictly dependent on the socioeconomic background of the country being considered. Typically, HCMV causes asymptomatic infection in the immunocompetent population, while in immunocompromised individuals or when transmitted vertically from the mother to the fetus it leads to systemic disease with severe complications and high mortality rate. Following primary infection, HCMV establishes a state of latency primarily in myeloid cells, from which it can be reactivated by various inflammatory stimuli. Several studies have shown that HCMV, despite being a DNA virus, is highly prone to genetic variability that strongly influences its replication and dissemination rates as well as cellular tropism. In this scenario, the few currently available drugs for the treatment of HCMV infections are characterized by high toxicity, poor oral bioavailability, and emerging resistance. -

How Influenza Virus Uses Host Cell Pathways During Uncoating
cells Review How Influenza Virus Uses Host Cell Pathways during Uncoating Etori Aguiar Moreira 1 , Yohei Yamauchi 2 and Patrick Matthias 1,3,* 1 Friedrich Miescher Institute for Biomedical Research, 4058 Basel, Switzerland; [email protected] 2 Faculty of Life Sciences, School of Cellular and Molecular Medicine, University of Bristol, Bristol BS8 1TD, UK; [email protected] 3 Faculty of Sciences, University of Basel, 4031 Basel, Switzerland * Correspondence: [email protected] Abstract: Influenza is a zoonotic respiratory disease of major public health interest due to its pan- demic potential, and a threat to animals and the human population. The influenza A virus genome consists of eight single-stranded RNA segments sequestered within a protein capsid and a lipid bilayer envelope. During host cell entry, cellular cues contribute to viral conformational changes that promote critical events such as fusion with late endosomes, capsid uncoating and viral genome release into the cytosol. In this focused review, we concisely describe the virus infection cycle and highlight the recent findings of host cell pathways and cytosolic proteins that assist influenza uncoating during host cell entry. Keywords: influenza; capsid uncoating; HDAC6; ubiquitin; EPS8; TNPO1; pandemic; M1; virus– host interaction Citation: Moreira, E.A.; Yamauchi, Y.; Matthias, P. How Influenza Virus Uses Host Cell Pathways during 1. Introduction Uncoating. Cells 2021, 10, 1722. Viruses are microscopic parasites that, unable to self-replicate, subvert a host cell https://doi.org/10.3390/ for their replication and propagation. Despite their apparent simplicity, they can cause cells10071722 severe diseases and even pose pandemic threats [1–3]. -

Topics in Viral Immunology Bruce Campell Supervisory Patent Examiner Art Unit 1648 IS THIS METHOD OBVIOUS?
Topics in Viral Immunology Bruce Campell Supervisory Patent Examiner Art Unit 1648 IS THIS METHOD OBVIOUS? Claim: A method of vaccinating against CPV-1 by… Prior art: A method of vaccinating against CPV-2 by [same method as claimed]. 2 HOW ARE VIRUSES CLASSIFIED? Source: Seventh Report of the International Committee on Taxonomy of Viruses (2000) Edited By M.H.V. van Regenmortel, C.M. Fauquet, D.H.L. Bishop, E.B. Carstens, M.K. Estes, S.M. Lemon, J. Maniloff, M.A. Mayo, D. J. McGeoch, C.R. Pringle, R.B. Wickner Virology Division International Union of Microbiological Sciences 3 TAXONOMY - HOW ARE VIRUSES CLASSIFIED? Example: Potyvirus family (Potyviridae) Example: Herpesvirus family (Herpesviridae) 4 Potyviruses Plant viruses Filamentous particles, 650-900 nm + sense, linear ssRNA genome Genome expressed as polyprotein 5 Potyvirus Taxonomy - Traditional Host range Transmission (fungi, aphids, mites, etc.) Symptoms Particle morphology Serology (antibody cross reactivity) 6 Potyviridae Genera Bymovirus – bipartite genome, fungi Rymovirus – monopartite genome, mites Tritimovirus – monopartite genome, mites, wheat Potyvirus – monopartite genome, aphids Ipomovirus – monopartite genome, whiteflies Macluravirus – monopartite genome, aphids, bulbs 7 Potyvirus Taxonomy - Molecular Polyprotein cleavage sites % similarity of coat protein sequences Genomic sequences – many complete genomic sequences, >200 coat protein sequences now available for comparison 8 Coat Protein Sequence Comparison (RNA) 9 Potyviridae Species Bymovirus – 6 species Rymovirus – 4-5 species Tritimovirus – 2 species Potyvirus – 85 – 173 species Ipomovirus – 1-2 species Macluravirus – 2 species 10 Higher Order Virus Taxonomy Nature of genome: RNA or DNA; ds or ss (+/-); linear, circular (supercoiled?) or segmented (number of segments?) Genome size – 11-383 kb Presence of envelope Morphology: spherical, filamentous, isometric, rod, bacilliform, etc.