Disruptive, Impulse-Control, and Conduct Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What Can Be Learned from White Matter Alterations in Antisocial Girls Willeke M
Menks WM, Raschle NM. J Neurol Neuromedicine (2017) 2(7): 16-20 Neuromedicine www.jneurology.com www.jneurology.com Journal of Neurology & Neuromedicine Mini Review Open Access What can be learned from white matter alterations in antisocial girls Willeke M. Menks1, Christina Stadler1 and Nora M. Raschle1 1Department of Child and Adolescent Psychiatry, University of Basel, Psychiatric University Hospital Basel, Switzerland. Article Info ABSTRACT Article Notes Antisocial behavior in youths constitutes a major public health problem Received: June 17, 2017 worldwide. Conduct disorder is a severe variant of antisocial behavior with higher Accepted: July 31, 2017 prevalence rates for boys (12%) as opposed to girls (7%). A better understanding *Correspondence: of the underlying neurobiological mechanisms of conduct disorder is warranted Dr. Willeke Menks, PhD to improve identification, diagnosis, or treatment. Functional and structural Department of Child and Adolescent Psychiatry (KJPK), neuroimaging studies have indicated several key brain regions within the limbic Psychiatric University Clinics Basel (UPK) system and prefrontal cortex that are altered in youths with conduct disorder. Schanzenstrasse 13, CH-4056 Basel, Switzerland Examining the structural connectivity, i.e. white matter fiber tracts connecting Tel. +41 61 265 89 76 these brain areas, may further inform about the underlying neural mechanisms. Fax +41 61 265 89 61 Diffusion tensor imaging (DTI) is a non-invasive technique that can evaluate the © 2017 Menks WM & Raschle NM. This article is distributed white matter integrity of fiber tracts throughout the brain. To date, DTI studies have under the terms of the Creative Commons Attribution 4.0 found several white matter tracts that are altered in youths with conduct disorder. -

2021 SEC Baseball SEC Overall Statistics (As of Jun 30, 2021) (All Games Sorted by Batting Avg)
2021 SEC Baseball SEC Overall Statistics (as of Jun 30, 2021) (All games Sorted by Batting avg) Team avg g ab r h 2b 3b hr rbi tb slg% bb hp so gdp ob% sf sh sb-att po a e fld% Ole Miss . 2 8 8 67 2278 478 656 109 985 437 1038 . 4 5 6 295 87 570 45 . 3 8 5343 44-65 1759 453 57 . 9 7 5 Vanderbilt . 2 8 5 67 2291 454 653 130 21 92 432 1101 . 4 8 1 301 53 620 41 . 3 7 8 17 33 92-104 1794 510 65 . 9 7 3 Auburn . 2 8 1 52 1828 363 514 101 986 344 891 . 4 8 7 230 34 433 33 . 3 6 8 21 16 32-50 1390 479 45 . 9 7 6 Florida . 2 7 9 59 2019 376 563 105 13 71 351 907 . 4 4 9 262 47 497 32 . 3 7 0 30 4 32-48 1569 528 68 . 9 6 9 Tennessee . 2 7 9 68 2357 475 657 134 12 98 440 1109 . 4 7 1 336 79 573 30 . 3 8 3 27 23 72-90 1844 633 59 . 9 7 7 Kentucky . 2 7 8 52 1740 300 484 86 10 62 270 776 . 4 4 6 176 63 457 28 . 3 6 2 21 16 78-86 1353 436 39 . 9 7 9 Mississippi State . 2 7 8 68 2316 476 644 122 13 75 437 1017 . 4 3 9 306 73 455 50 . 3 7 5 31 13 74-92 1811 515 60 . -

Motor, Emotional and Cognitive Empathic Abilities in Children with Autism and Conduct Disorder Danielle M.A
Motor, Emotional and Cognitive Empathic Abilities in Children with Autism and Conduct Disorder Danielle M.A. Bons1,2 Floor E. Scheepers1 [email protected] [email protected] +31 (0)488 – 469 611 Nanda N.J. Rommelse1,2 Jan K. Buitelaar1,2 [email protected] [email protected] +31 (0)24 351 2222 1Karakter child- and adolescent psychiatry 2Department of Psychiatry UMC St. Radboud University Centre Nijmegen, Zetten-Tiel P.O. Box 9101, 6500HB Nijmegen, The P.O. Box 104, 6670AC Zetten, The Netherlands Netherlands ABSTRACT repetitive patterns of behavior, interests and activities. This paper gives an overview of the studies that Children with conduct disorder (CD) show a pattern of investigated motor, emotional and cognitive empathy in behavior violating the basic rights of others and age- juveniles with autism or conduct disorder. Studies that appropriate norms and rules, which may develop in measured response to emotional faces with use of facial antisocial behavior in adulthood. At first sight these EMG, ECG, skin conductance, eye-tracking or emotion disorders appear to have little in common. However, lack of recognition are discussed. In autism facial mimicry and empathy is a core symptom in both ASD and CD. emotion recognition, as well as attention to the eyes, seem to be reduced. In conduct disorder facial mi micry seems to Empathy is assumed to consist out of three components: be impaired as well as recognition of fear and sad facial motor, emotional and cognitive empathy [5]. Motor expressions, and possibly associated with lack of attention empathy refers to unconsciously mirroring the facial to the eyes. -

Volume 2, Spring 2020
JOURNAL OF BEHAVIORAL SCIENCES Spring 2020 COLLEGE OF Saint Elizabeth Title: Fathering Emotions: The Relationship between Fathering and Emotional Development Author(s): Anthony J. Ferrer Abstract The study of child development is an ever growing and consistently important area of psychology. Research suggests that parenting starts as early as conception and that a developing fetus can be affected by maternal and parental bonding in addition to biological influences. However there is a lack of research regarding the effect fathering has on the child’s development and there is a surplus of research regarding the effect of mothers parenting on the child’s development. Currently research neglects families raised by single fathers, two fathers, and other cis-male and trans-male caregivers. This paper will provide an in-depth review of emotional development in children, “parenting”, and will highlight the limited literature on the effects of fathering on emotional development. Title: Brain Impairments in Maltreated Children Author(s): Carl C. Papandrea Abstract The purpose of this paper is to explore the brain development in typically developing and maltreated children as noted by neuroimaging technology. The use of magnetic resonance imaging (MRI) provides insight into how early experiences affect the developing brain, and provides biological implications for what practitioners identified through behavioral, psychological, and emotional terms. Neurobiological impairments have been seen in children who experience adverse childhood experiences, this paper reviews literature that identifies and explains these findings. Title: Common Personality Traits in Youth and Connection with Antisocial Personality Author(s): Carl C. Papandrea Abstract The purpose of this paper is to explore the links between common maladaptive personality traits in youth with conduct problems and their connection to Antisocial Personality Disorder. -

Conduct Disorder - Psychopathy
Conduct Disorder - Psychopathy Professor Jan Buitelaar Radboud University Nijmegen Medical Center Donders Institute for Brain, Cognition and Behavior Department of Cognitive Neuroscience, and Karakter Child and Adolescent Psychiatry University Center Nijmegen, The Netherlands Conflict of Interest Jan Buitelaar Speaker Advisory Board Research Support Involved in clinical trials Lilly ConflictX of interestX X X Janssen Cilag X X X Novartis X Organon X Medice X Shire X X X Pfizer X Otsuka/BMS X Servier X “I am not quite sure what I would call that expression, but I know that is what people look like just before you stab them” So what’s happening? Theories on why resting heart rate is low …. History Developmental Model of Aggression Prenatal smoking Prenatal alcohol Environmental Obstetric problems RISKS Abuse, neglect Parental rejection Inconsistent parenting, harsh discipline Parental psychopathology Insufficient parental supervision Poor neighborhood, deviant peer group Birth Childhood Adolescence Adulthood Temperament, IQ, Pro-social skills Arousal mechanisms Socialization GENES 1. Conditioning, sensitivity to punishment 2. Control mechanisms 3. Empathy, moral reasoning Taxonomy of aggression Psychopathic traits: 1. Callous-unemotional 2. Impulsivity 3. Narcissism Impulsive versus Instrumental aggression Early versus Late Onset Common Misconceptions about DBDs (1) • Disruptive behaviours refer to annoying problem behaviours that are just a matter of inadequate parenting Common Misconceptions about DBDs (1) • Disruptive behaviours refer -

Behavioral Addictions in Bipolar Disorders: a Systematic Review 77
European Neuropsychopharmacology (2019) 29, 76–97 www.elsevier.com/locate/euroneuro Behavioral addictions in bipolar disorders: A systematic review a a, ∗∗ a a a C Varo , A Murru , E Salagre , E Jiménez , B Solé , a b ,c d, e a L Montejo , AF Carvalho , B Stubbs , I Grande , a a, ∗ a A Martínez-Arán , E Vieta , M Reinares a Bipolar Disorders and Depressive Unit, Hospital Clinic, Institute of Neurosciences, University of Barcelona, IDIBAPS, CIBERSAM, Barcelona, Catalonia, Spain b Department of Psychiatry, University of Toronto, Toronto, ON, Canada c Centre for Addiction and Mental Health (CAMH), Toronto, ON, Canada d Physiotherapy Department, South London and Maudsley NHS Foundation Trust, Denmark Hill, London SE5 8AZ, United Kingdom e Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, De Crespigny Park, London, Box SE5 8AF, United Kingdom Received 17 July 2018; received in revised form 18 September 2018; accepted 23 October 2018 KEYWORDS Abstract Bipolar disorder; Clinical and epidemiological research suggests that behavioral addictions (BA) are associated Behavioral addictions; with a wide range of psychiatric disorders. However, the relationship between BA and bipo- Comorbidity; lar disorders (BD) has not been thoroughly explored. The aim of this systematic review was Prevalence; to critically summarize and evaluate the current available evidence regarding a possible asso- Treatment ciation between BA and BD. A systematic review of major electronic databases according to PRISMA guidelines was conducted from inception to 31st December 2017. We sought quanti- tative studies data concerning prevalence of comorbidity, features and treatment related to BA-BD comorbidity. Data were narratively synthesized. -

Kleptomania: Clinical Characteristics and Treatment
S11 Cleptomania: características clínicas e tratamento Kleptomania: clinical characteristics and treatment Jon E Grant,1 Brian L Odlaug1 Resumo Objetivos: A cleptomania, um transtorno incapacitante pertencente ao grupo de transtornos de controle dos impulsos, caracte- riza-se pelo furto repetitivo e incontrolável de itens que são de pequena utilidade para a pessoa acometida. Apesar de seu histórico relativamente longo, a cleptomania continua sendo pouco entendida pelo público geral, pelos clínicos e pelos que dela sofrem. Método: Este artigo revisa a literatura sobre o que se sabe a respeito das características clínicas, histórico familiar, neurobiologia e opções de tratamento para indivíduos com cleptomania. Resultados: A cleptomania geralmente tem seu início no final da adolescência ou no início da vida adulta, e parece ser mais comum em mulheres. A comorbidade psiquiátrica ao longo da vida com outros transtornos de controle de impulsos (20-46%), de uso de substâncias (23-50%) e de humor (45-100%) é freqüente. Indivíduos com cleptomania sofrem de prejuízo significativo em sua capacidade de funcionamento social e ocupacional. A cleptomania pode responder ao tratamento com terapia cognitivo-comportamental e com várias farmacoterapias (lítio, antiepilépticos e antagonistas de opióides). Conclusões: A cleptomania é um transtorno incapacitante que resulta em uma vergonha intensa, bem como problemas legais, sociais, familiares e ocupacionais. São necessários estudos de tratamento em ampla escala. Descritores: Transtornos do controle de impulso; Farmacoterapia; Comorbidade; Roubo; Características de estudos [Tipo de publicação] Abstract Objectives: Kleptomania, a disabling impulse control disorder, is characterized by the repetitive and uncontrollable theft of items that are of little use to the afflicted person. -

The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic Criteria for Research
The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic criteria for research World Health Organization Geneva The World Health Organization is a specialized agency of the United Nations with primary responsibility for international health matters and public health. Through this organization, which was created in 1948, the health professions of some 180 countries exchange their knowledge and experience with the aim of making possible the attainment by all citizens of the world by the year 2000 of a level of health that will permit them to lead a socially and economically productive life. By means of direct technical cooperation with its Member States, and by stimulating such cooperation among them, WHO promotes the development of comprehensive health services, the prevention and control of diseases, the improvement of environmental conditions, the development of human resources for health, the coordination and development of biomedical and health services research, and the planning and implementation of health programmes. These broad fields of endeavour encompass a wide variety of activities, such as developing systems of primary health care that reach the whole population of Member countries; promoting the health of mothers and children; combating malnutrition; controlling malaria and other communicable diseases including tuberculosis and leprosy; coordinating the global strategy for the prevention and control of AIDS; having achieved the eradication of smallpox, promoting mass immunization against a number of other -

Baseball/Softball
SAMPLE SITUTATIONS Situation Enter for batter Enter for runner Hit (single, double, triple, home run) 1B or 2B or 3B or HR Hit to location (LF, CF, etc.) 3B 9 or 2B RC or 1B 6 Bunt single 1B BU Walk, intentional walk or hit by pitch BB or IBB or HP Ground out or unassisted ground out 63 or 43 or 3UA Fly out, pop out, line out 9 or F9 or P4 or L6 Pop out (bunt) P4 BU Line out with assist to another player L6 A1 Foul out FF9 or PF2 Foul out (bunt) FF2 BU or PF2 BU Strikeouts (swinging or looking) KS or KL Strikeout, Fouled bunt attempt on third strike K BU Reaching on an error E5 Fielder’s choice FC 4 46 Double play 643 GDP X Double play (on strikeout) KS/L 24 DP X Double play (batter reaches 1B on FC) FC 554 GDP X Double play (on lineout) L63 DP X Triple play 543 TP X (for two runners) Sacrifi ce fl y F9 SF RBI + Sacrifi ce bunt 53 SAC BU + Sacrifi ce bunt (error on otherwise successful attempt) E2T SAC BU + Sacrifi ce bunt (no error, lead runner beats throw to base) FC 5 SAC BU + Sacrifi ce bunt (lead runner out attempting addtional base) FC 5 SAC BU + 35 Fielder’s choice bunt (one on, lead runner out) FC 5 BU (no sacrifi ce) 56 Fielder’s choice bunt (two on, lead runner out) FC 5 BU (no sacrifi ce) 5U (for lead runner), + (other runner) Catcher or batter interference CI or BI Runner interference (hit by batted ball) 1B 4U INT (awarded to closest fi elder)* Dropped foul ball E9 DF Muff ed throw from SS by 1B E3 A6 Batter advances on throw (runner out at home) 1B + T + 72 Stolen base SB Stolen base and advance on error SB E2 Caught stealing -
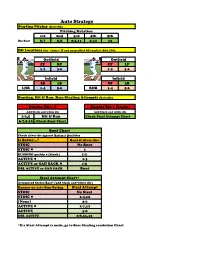
Auto Strategy Starting Pitcher (Roll 2D6) Pitching Rotation 1St 2Nd 3Rd 4Th 5Th Die Roll 6,7 5,8 2-4,11 9,12 10
Auto Strategy Starting Pitcher (Roll 2D6) Pitching Rotation 1st 2nd 3rd 4th 5th Die Roll 6,7 5,8 2-4,11 9,12 10 Hit Locations (for "choice" IF and unspecified OF results) (Roll 1D6) Outfield Outfield CF RF CF LF LHB 1-2 3-6 RHB 1-2 3-6 Infield Infield 2B 1B SS 3B LHB 1-4 5-6 RHB 1-4 5-6 Bunting, Hit & Run, Base Stealing Attempts (Roll 3D6) Decider Die = l Decider Die = [blank] Add black and white die Add black and white die 2-3,5 Hit & Run Check Steal Attempt Chart 6-7,9-10 Check Bunt Chart Bunt Chart Check silver die against Batter's Qualities Is Batter…? Bunt if silver die= STOIC No Bunt STOIC l 1 RUNNING quality = [blank] 1-2 ACTIVE l 1-3 ACTIVE or SAD SACK l 1-5 DBL ACTIVE or SAD SACK Bunt Steal Attempt Chart* Attempted Stolen Base? (add black and white die) Runner on 1st's Run Rating Steal Attempt STOIC No Steal STOIC l 2-4,12 [None] 2-6 ACTIVE l 2-7,12 ACTIVE 3-8 DBL ACTIVE 2-8,11,12 *If a Steal Attempt is made, go to Base Stealing resolution Chart Base Stealing Resolution (Roll 3D6) Base Stealing Chart Roll 3 die: Add black and white die and 2 Runner Safe? check total on Steal Chart (left). 3 Runner Safe? Use silver die for Runner Safe? Chart 4 Runner Safe? 5 Stolen Base 6 Runner Safe? 7 Stolen Base 8 Runner Safe? 9 Caught Stealing 10 Runner Safe? 11 Stolen Base 12 Runner Safe? Runner Safe? Chart Use this chart to resolve Runner Safe? results on Base Stealing Chart If silver die is less than or equal to number below, then runner is SAFE Catcher Defence Ratings Is Runner...? Gold Gold l [Blank] Iron l Iron STOIC CS CS CS 1 2 STOIC l CS CS 1 2 3 [blank] 1 2 3 4 5 ACTIVE l 2 3 4 5 SB ACTIVE 3 4 5 SB SB DBL ACTIVE 4 5 SB SB SB CS = Caught Stealing SB = Stolen Base 2-6-6 Roll - Runner Out at First Base Roll one die against Runner on 1st's Run Rating Is Runner...? Pickoff CS STOIC 1-6* STOIC l 1-2 3-6 [blank] 1-3 4-6 ACTIVE l 1-4 5-6 ACTIVE 1-5 6 DBL ACTIVE 1-6* * On a '6,' roll DECIDER DIE: l=Pickoff/[Blank]=Caught Stealing HMB Auto Strategy Notes David Gambrill, Toronto, ON First off, let me start by saying I am a Johnny-come-lately baseball fan. -
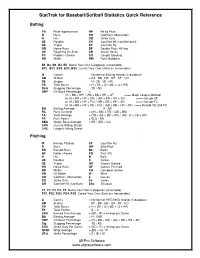
Stattrak for Baseball/Softball Statistics Quick Reference
StatTrak for Baseball/Softball Statistics Quick Reference Batting PA Plate Appearances HP Hit by Pitch R Runs CO Catcher's Obstruction H Hits SO Strike Outs 2B Doubles SH Sacrifice Hit (sacrifice bunt) 3B Triples SF Sacrifice Fly HR Home Runs DP Double Plays Hit Into OE Reaching On-Error SB Stolen Bases FC Fielder’s Choice CS Caught Stealing BB Walks RBI Runs Batted In B1, B2, B3, B4, B5 Name Your Own Categories (renamable) BS1, BS2, BS3, BS4, BS5 Create Your Own Statistics (renamable) G Games = Number of Batting records in database AB At Bats = PA - BB - HP - SH - SF - CO 1B Singles = H - 2B - 3B - HR TB Total Bases = H + 2B + (2 x 3B) + (3 x HR) SLG Slugging Percentage = TB / AB OBP On-Base Percentage = (H + BB + HP) / (AB + BB + HP + SF) <=== Major League Method or (H + BB + HP + OE) / (AB + BB + HP + SF) <=== Include OE or (H + BB + HP + FC) / (AB + BB + HP + SF) <=== Include FC or (H + BB + HP + OE + FC) / (AB + BB + HP + SF) <=== Include OE and FC BA Batting Average = H / AB RC Runs Created = ((H + BB) x TB) / (AB + BB) TA Total Average = (TB + SB + BB + HP) / (AB - H + CS + DP) PP Pure Power = SLG - BA SBA Stolen Base Average = SB / (SB + CS) CHS Current Hitting Streak LHS Longest Hitting Streak Pitching IP Innings Pitched SF Sacrifice Fly R Runs WP Wild Pitch ER Earned-Runs Bk Balks BF Batters Faced PO Pick Offs H Hits B Balls 2B Doubles S Strikes 3B Triples GS Games Started HR Home Runs GF Games Finished BB Walks CG Complete Games HB Hit Batter W Wins CO Catcher's Obstruction L Losses SO Strike Outs Sv Saves SH Sacrifice Hit -

NFCA Home Plate: ATEC: Beyond the Basics of Scoring Fastpitch Softball
NFCA Home Plate: ATEC: Beyond the Basics of Scoring Fastpitch Softball by Jeri Findlay Published by National Fastpitch Coaches Association Copyright 1999. All Right Reserved Introduction Basic Guidelines and Scorer Responsibilities Proving A Box Score Percentages and Averages Cumulative Performance Records Called and Forfeited Games Offense: Statistics Offense: Hits Offense: Extra Base Hits Offense: Game Ending Hits Offense: Fielder's Choice Offense: Sacrifices Offense: Runs Batted In (RBI) Offense: Batting Out of Order Offense: Strikeouts Offense: Stolen Bases Offense: Caught Stealing (Unsuccessful Attempt) Defense: Statistics Defense: Errors Defense: Putouts Defense: Assists Defense: Double Play/Triple Play Defense: Throw Outs Pitching: Statistics Pitching: Earned Runs Pitching: Charging Runs Scored (When Relief Pitchers Are Used) Pitching: Strikeouts Pitching: Bases On Balls Pitching: Wild Pitches/Passed Balls Pitching: Winning and Losing Pitcher Pitching: Saves Scoring The Tie-Breaker Some images Copyright www.arttoday.com Web design by Ray Foster. Reproduction of material from any NFCA Home Plate pages without written permission is strictly prohibited. Copyright ©1999 National Fastpitch Coaches Association. NFCA, 409 Vandiver Drive, Suite 5-202, Columbia, MO 65202 TELEPHONE (573) 875-3033 | FAX (573) 875-2924 | EMAIL http://www.nfca.org/indexscoringfp.lasso [1/27/2002 2:21:41 AM] NFCA Homeplate: ATEC: Beyond The Basics of Scoring Fastpitch Softball TABLE OF CONTENTS Introduction Introduction Basic Guidelines and Scorer - - - - - - - - - - - - - - - - - - - - - - - Responsibilities Proving A Box Score Published by: National Softball Coaches Association Percentages and Averages Written by Jeri Findlay, Head Softball Coach, Ball State University Cumulative Performance Records Introduction Called and Forfeited Games Scoring in the game of fastpitch softball seems to be as diversified as the people Offense: Statistics playing it.