I VASCULAR BIOCHEMISTRY of VITAMIN
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Uneven Distribution of Cobamide Biosynthesis and Dependence in Bacteria Predicted By
bioRxiv preprint doi: https://doi.org/10.1101/342006; this version posted June 8, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. 1 Uneven distribution of cobamide biosynthesis and dependence in bacteria predicted by 2 comparative genomics 3 4 Running title: Cobamide biosynthesis predictions 5 6 Amanda N. Shelton1, Erica C. Seth1, Kenny C. Mok1, Andrew W. Han2, Samantha N. Jackson3,4, 7 David R. Haft3, Michiko E. Taga1* 8 9 1 Department of Plant & Microbial Biology, University of California, Berkeley, Berkeley, CA, 10 USA 11 2 Second Genome, Inc., South San Francisco, CA, USA 12 3 J. Craig Venter Institute, Rockville, MD, USA 13 4 Current address: Department of Biological & Environmental Engineering, Cornell University, 14 Ithaca, NY, USA 15 16 * Address correspondence to Michiko E. Taga, [email protected] 17 18 19 -- 20 Abstract 21 22 The vitamin B12 family of cofactors known as cobamides are essential for a variety of microbial 23 metabolisms. We used comparative genomics of 11,000 bacterial species to analyze the extent 1 bioRxiv preprint doi: https://doi.org/10.1101/342006; this version posted June 8, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. 24 and distribution of cobamide production and use across bacteria. -
PDF Document Created by Pdffiller
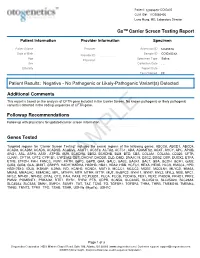
Patient: 1234567843314948-COtGx0053 CLIA ID#: 11D2066426 Larry Hung, MD, Laboratory Director GxTM Carrier Screen Testing Report Patient Information Provider Information Specimen Patient Name Haley Papevies Provider Harbin Clinic Women's Accession ID 1234567843314948 Center Cartersville Date of Birth Apr 16, 1998 Sample ID COtGx0053XX Provider ID 1124488556 Age 19 Specimen Type Saliva Physician Vicki Yates Sex female Collection Date Jul 20, 2017 Ethnicity Report Date Aug 5, 2017 Test Ordered CF Patient Results: Negative - No Pathogenic or Likely-Pathogenic Variant(s) Detected Additional Comments This report is based on the analysis of CFTR gene included in the Carrier Screen. No known pathogenic or likely pathogenic variant(s) detected in the coding sequences of CFTR gene. Followup Recommendations Follow up with physicians for updated carrier screen information. The sequencing for CFTR gene was carried out with the other genes included in the Carrier Screen Testing (listed below). The analysis of the other genes in the Carrier Screen could be ordered through your physicians. Genes Tested Targeted regions for “Carrier Screen Testing” includes the exonic regions of the following genes: ABCC8, ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACSF3, ACTA2, ACTC1, ADA, ADAMTS2, AGXT, AHCY, APC, APOB, ARG1, ASL, ASPA, ASS1, ATP7B, AUH, BCKDHA, BBS2, BCKDHB, BLM, BTD, CBS, COL3A1, COL4A3, CD320, CFTR, CLRN1, CPT1A, CPT2, CYP1B1, CYP21A2, DBT, DHCR7, DHDDS, DLD, DMD, DNAJC19, DSC2, DSG2, DSP, DUOX2, ETFA, ETFB, ETFDH, FAH, FANCC, FBN1, -

Supplement 1 Overview of Dystonia Genes
Supplement 1 Overview of genes that may cause dystonia in children and adolescents Gene (OMIM) Disease name/phenotype Mode of inheritance 1: (Formerly called) Primary dystonias (DYTs): TOR1A (605204) DYT1: Early-onset generalized AD primary torsion dystonia (PTD) TUBB4A (602662) DYT4: Whispering dystonia AD GCH1 (600225) DYT5: GTP-cyclohydrolase 1 AD deficiency THAP1 (609520) DYT6: Adolescent onset torsion AD dystonia, mixed type PNKD/MR1 (609023) DYT8: Paroxysmal non- AD kinesigenic dyskinesia SLC2A1 (138140) DYT9/18: Paroxysmal choreoathetosis with episodic AD ataxia and spasticity/GLUT1 deficiency syndrome-1 PRRT2 (614386) DYT10: Paroxysmal kinesigenic AD dyskinesia SGCE (604149) DYT11: Myoclonus-dystonia AD ATP1A3 (182350) DYT12: Rapid-onset dystonia AD parkinsonism PRKRA (603424) DYT16: Young-onset dystonia AR parkinsonism ANO3 (610110) DYT24: Primary focal dystonia AD GNAL (139312) DYT25: Primary torsion dystonia AD 2: Inborn errors of metabolism: GCDH (608801) Glutaric aciduria type 1 AR PCCA (232000) Propionic aciduria AR PCCB (232050) Propionic aciduria AR MUT (609058) Methylmalonic aciduria AR MMAA (607481) Cobalamin A deficiency AR MMAB (607568) Cobalamin B deficiency AR MMACHC (609831) Cobalamin C deficiency AR C2orf25 (611935) Cobalamin D deficiency AR MTRR (602568) Cobalamin E deficiency AR LMBRD1 (612625) Cobalamin F deficiency AR MTR (156570) Cobalamin G deficiency AR CBS (613381) Homocysteinuria AR PCBD (126090) Hyperphelaninemia variant D AR TH (191290) Tyrosine hydroxylase deficiency AR SPR (182125) Sepiaterine reductase -

Abstracts from the 9Th Biennial Scientific Meeting of The
International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):15 DOI 10.1186/s13633-017-0054-x MEETING ABSTRACTS Open Access Abstracts from the 9th Biennial Scientific Meeting of the Asia Pacific Paediatric Endocrine Society (APPES) and the 50th Annual Meeting of the Japanese Society for Pediatric Endocrinology (JSPE) Tokyo, Japan. 17-20 November 2016 Published: 28 Dec 2017 PS1 Heritable forms of primary bone fragility in children typically lead to Fat fate and disease - from science to global policy a clinical diagnosis of either osteogenesis imperfecta (OI) or juvenile Peter Gluckman osteoporosis (JO). OI is usually caused by dominant mutations affect- Office of Chief Science Advsor to the Prime Minister ing one of the two genes that code for two collagen type I, but a re- International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):PS1 cessive form of OI is present in 5-10% of individuals with a clinical diagnosis of OI. Most of the involved genes code for proteins that Attempts to deal with the obesity epidemic based solely on adult be- play a role in the processing of collagen type I protein (BMP1, havioural change have been rather disappointing. Indeed the evidence CREB3L1, CRTAP, LEPRE1, P4HB, PPIB, FKBP10, PLOD2, SERPINF1, that biological, developmental and contextual factors are operating SERPINH1, SEC24D, SPARC, from the earliest stages in development and indeed across generations TMEM38B), or interfere with osteoblast function (SP7, WNT1). Specific is compelling. The marked individual differences in the sensitivity to the phenotypes are caused by mutations in SERPINF1 (recessive OI type obesogenic environment need to be understood at both the individual VI), P4HB (Cole-Carpenter syndrome) and SEC24D (‘Cole-Carpenter and population level. -

6. Annular Space & Sealing
6. Annular Space & Sealing (this page left intentionally blank) 6. Annular Space & Sealing Chapter Table of Contents Chapter Table of Contents Chapter Description ......................................................................................................................................................................................... 6 Regulatory Requirements – Annular Space & Sealing of a New Well ..................................................................................................... 6 Relevant Sections – The Wells Regulation.............................................................................................................................................. 6 The Requirements – Plainly Stated .......................................................................................................................................................... 6 Well Record – Relevant Sections............................................................................................................................................................14 Best Management Practice – Report use of Centralizers .......................................................................................................... 15 Key Concepts ..................................................................................................................................................................................................16 The Annular Space ...................................................................................................................................................................................16 -
Underwater Inspection and Repair of Bridge Substructures
[.Tl [•1•] NATIONAL COOPERATIVE HIGHWAY RESEARCH PROGRAM SYNTHESIS OF HIGHWAY PRACTICE UNDERWATER INSPECTION AND REPAIR OF BRIDGE SUBSTRUCTURES Supv ) ç J j p1 JUNO 81982 3 up2Leder I.T.D. DIV OF H!GHWAYS BRIDGE SECTION FUe_OUT MAIL TRANSPORTATION RESEARCH BOARD NATIONAL RESEARCH COUNCIL TRANSPORTATION RESEARCH BOARD EXECUTIVE COMMITTEE 1981 Officers Chairman THOMAS D. LARSON Secretary, Pennsylvania Department of Transportation Vice Chairman DARRELL V MANNING, Director, Idaho Transportation Department Secretary THOMAS B. DEEN, Executive Director, Transportation Research Board Members RAY A. BARNHART, Federal Highway Administrator, U.S. Department of Transportation (cx officio) ROBERT W. BLANCHETTE, Federal Railroad Administrator, U.S. Department of Transportation (cx officio) FRANCIS B. FRANCOIS, Executive Director, American Association of State Highway and Transportation Officials (cx officio) WILLIAM J. HARRIS, JR., Vice President—Research and lest Department, Association of American Railroad.. (ex officio) J. LYNN HELMS, Federal Aviation Administrator, U.S. Department of Transportation (cx officio) PETER G. KOLTNOW, President, Highway Users Federation for Safety and Mobility (cx officio. Past Chairman, 1979) ELLIOTT W. MONTROLL, Chairman, Co,n,nission on Sociotechnical Systems, National Research Council (cx officio) RAYMOND A. PECK, JR., National Highway Traffic Safety Administrator, U.S. Department of Transportation (cx officio) ARTHUR E. TEELE, JR., Urban Mass Transportation Administrator, U.S. Department of Transportation (cx officio) JOHN F. WING, Senior Vice President, Booz. Allen & Hamilton. Inc. (cx officio, MTRB liaison) CHARLEY V. WOOTAN. Director, Texas Transportation Institute, Texas A&M University (cx officio, Past Chairman 1980) GEORGE J. BEAN. Director of Aviation, Hilisborough County (Florida) Aviation Authority THOMAS W. BRADSHAW, JR., Secretary, North Carolina Department of Transportation RICHARD P. -

Oral Presentations
Journal of Inherited Metabolic Disease (2018) 41 (Suppl 1):S37–S219 https://doi.org/10.1007/s10545-018-0233-9 ABSTRACTS Oral Presentations PARALLEL SESSION 1A: Clycosylation and cardohydrate disorders O-002 Link between glycemia and hyperlipidemia in Glycogen Storage O-001 Disease type Ia Hoogerland J A1, Hijmans B S1, Peeks F1, Kooijman S3, 4, Bos T2, Fertility in classical galactosaemia, N-glycan, hormonal and inflam- Bleeker A1, Van Dijk T H2, Wolters H1, Havinga R1,PronkACM3, 4, matory gene expression interactions Rensen P C N3, 4,MithieuxG5, 6, Rajas F5, 6, Kuipers F1, 2,DerksTGJ1, Reijngoud D1,OosterveerMH1 Colhoun H O1,Rubio-GozalboME2,BoschAM3, Knerr I4,DawsonC5, Brady J J6,GalliganM8,StepienKM9, O'Flaherty R O7,MossC10, 1Dep Pediatrics, CLDM, Univ of Groningen, Groningen, Barker P11, Fitzgibbon M C6, Doran P8,TreacyEP1, 4, 9 Netherlands, 2Lab Med, CLDM, Univ of Groningen, Groningen, Netherlands, 3Dep of Med, Div of Endocrinology, LUMC, Leiden, 1Dept Paediatrics, Trinity College Dublin, Dublin, Ireland, 2Dept Paeds and Netherlands, 4Einthoven Lab Exp Vasc Med, LUMC, Leiden, Clin Genetics, UMC, Maastricht, Netherlands, 3Dept Paediatrics, AMC, Netherlands, 5Institut Nat Sante et Recherche Med, Lyon, Amsterdam, Netherlands, 4NCIMD, TSCUH, Dublin, Ireland, 5Dept France, 6Univ Lyon 1, Villeurbanne, France Endocrinology, NHS Foundation Trust, Birmingham, United Kingdom, 6Dept Clin Biochem, MMUH, Dublin, Ireland, 7NIBRT Glycoscience, Background: Glycogen Storage Disease type Ia (GSD Ia) is an NIBRT, Dublin, Ireland, 8UCDCRC,UCD,Dublin,Ireland,9NCIMD, inborn error of glucose metabolism characterized by fasting hypo- MMUH, Dublin, Ireland, 10Conway Institute, UCD, Dublin, Ireland, glycemia, hyperlipidemia and fatty liver disease. We have previ- 11CBAL, NHS Foundation, Cambridge, United Kingdom ously reported considerable heterogeneity in circulating triglycer- ide levels between individual GSD Ia patients, a phenomenon that Background: Classical Galactosaemia (CG) is caused by deficiency of is poorly understood. -

Construction of Tremie Concrete Cutoff Wall, Wolf Creek Dam, Kentucky
c / y (y ¥ f t D n a a n in_r uir D 0!ID§Ii I <__ -j M IS C E L L A N E O U S PAPER SL-80-10 CONSTRUCTION OF TREMIE CONCRETE CUTOFF WALL, WOLF CREEK DAM, KENTUCKY by Terence C. Holland, Joseph R. Turner Structures Laboratory U. S. Army Engineer Waterways Experiment Station P. O. Box 631, Vicksburg, Miss. 39180 September 1980 Final Report Approved For Public Release; Distribution Unlimited Prepared for Office, Chief of Engineers, U. S. Army TA Washington, D. C. 20314 7 .W34m Under C W IS 3 I5 5 3 SL-80-10 1980 », Ar ' \ 8 ;v ;>"* % * OCT 2 7 1980 Water & : as Service Denver, Colorado Destroy this report when no longer needed. Do not return it to the originator. The findings in this report are not to be construed as an official Department of the Army position unless so designated by other authorized documents. The contents of this report are not to be used for advertising, publication, or promotional purposes. Citation of trade names does not constitute an official endorsement or approval of the use of such commercial products. SURÈAU OF RECLAMATrON DENVER u *W ff \& A /P 92059356 \y£ ,\s> , *c£p £ > b <0 Unclassified V * ie05*l35Ï.V SECURITY CLASSIFICATION OF THIS PAGE (When Data Entered) O' READ INSTRUCTIONS REPORT DOCUMENTATION PAGE BEFORE COMPLETING FORM 1. REPORT NUMBER 2. GOVT ACCESSION NO. 3. RECIPIENT'S CATALOG NUMBER Miscellaneous Paper SL-80-10 ' 4. T I T L E (and Subtitle) 5. TYPE OF REPORT & PERIOD COVERED V CONSTRUCTION OF TREMIE CONCRETE CUTOFF WALL, Final report WOLF CREEK DAM, KENTUCKY 6. -

Nobel Lecture by Roger Y. Tsien
CONSTRUCTING AND EXPLOITING THE FLUORESCENT PROTEIN PAINTBOX Nobel Lecture, December 8, 2008 by Roger Y. Tsien Howard Hughes Medical Institute, University of California San Diego, 9500 Gilman Drive, La Jolla, CA 92093-0647, USA. MOTIVATION My first exposure to visibly fluorescent proteins (FPs) was near the end of my time as a faculty member at the University of California, Berkeley. Prof. Alexander Glazer, a friend and colleague there, was the world’s expert on phycobiliproteins, the brilliantly colored and intensely fluorescent proteins that serve as light-harvesting antennae for the photosynthetic apparatus of blue-green algae or cyanobacteria. One day, probably around 1987–88, Glazer told me that his lab had cloned the gene for one of the phycobilipro- teins. Furthermore, he said, the apoprotein produced from this gene became fluorescent when mixed with its chromophore, a small molecule cofactor that could be extracted from dried cyanobacteria under conditions that cleaved its bond to the phycobiliprotein. I remember becoming very excited about the prospect that an arbitrary protein could be fluorescently tagged in situ by genetically fusing it to the phycobiliprotein, then administering the chromophore, which I hoped would be able to cross membranes and get inside cells. Unfortunately, Glazer’s lab then found out that the spontane- ous reaction between the apoprotein and the chromophore produced the “wrong” product, whose fluorescence was red-shifted and five-fold lower than that of the native phycobiliprotein1–3. An enzyme from the cyanobacteria was required to insert the chromophore correctly into the apoprotein. This en- zyme was a heterodimer of two gene products, so at least three cyanobacterial genes would have to be introduced into any other organism, not counting any gene products needed to synthesize the chromophore4. -

Surprising Roles for Bilins in a Green Alga Jean-David Rochaix1 Departments of Molecular Biology and Plant Biology, University of Geneva,1211 Geneva, Switzerland
COMMENTARY COMMENTARY Surprising roles for bilins in a green alga Jean-David Rochaix1 Departments of Molecular Biology and Plant Biology, University of Geneva,1211 Geneva, Switzerland It is well established that the origin of plastids which serves as chromophore of phyto- can be traced to an endosymbiotic event in chromes (Fig. 1). An intriguing feature of which a free-living photosynthetic prokaryote all sequenced chlorophyte genomes is that, invaded a eukaryotic cell more than 1 billion although they lack phytochromes, their years ago. Most genes from the intruder genomes encode two HMOXs, HMOX1 were gradually transferred to the host nu- andHMOX2,andPCYA.InPNAS,Duanmu cleus whereas a small number of these genes et al. (6) investigate the role of these genes in were maintained in the plastid and gave the green alga Chlamydomonas reinhardtii rise to the plastid genome with its associated and made unexpected findings. protein synthesizing system. The products of Duanmu et al. first show that HMOX1, many of the genes transferred to the nucleus HMOX2, and PCYA are catalytically active were then retargeted to the plastid to keep it and produce bilins in vitro (6). They also functional. Altogether, approximately 3,000 demonstrate in a very elegant way that these nuclear genes in plants and algae encode proteins are functional in vivo by expressing plastid proteins, whereas chloroplast ge- a cyanobacteriochrome in the chloroplast Fig. 1. Tetrapyrrole biosynthetic pathways. The heme nomes contain between 100 and 120 genes of C. reinhardtii, where, remarkably, the and chlorophyll biosynthetic pathways diverge at pro- (1). A major challenge for eukaryotic pho- photoreceptor is assembled with bound toporphyrin IX (ProtoIX). -

Theoretical Study of the Excited States of Chlorin, Bacteriochlorin, Pheophytin A, and Chlorophyll a by the SAC/SAC-CI Method
1320 J. Phys. Chem. B 1998, 102, 1320-1326 Theoretical Study of the Excited States of Chlorin, Bacteriochlorin, Pheophytin a, and Chlorophyll a by the SAC/SAC-CI Method J. Hasegawa, Y. Ozeki, K. Ohkawa, M. Hada, and H. Nakatsuji*,† Department of Synthetic and Biological Chemistry, Faculty of Engineering, Kyoto UniVersity, Sakyo-ku, Kyoto 606-01, Japan ReceiVed: September 4, 1997; In Final Form: NoVember 19, 1997 Excited states of free base chlorin (FBC), free base Bacteriochlorin (FBBC), pheophytin a (Pheo a), and chlorophyll a (Chlo a), which are derivatives of free base porphine (FBP), were calculated by the SAC (symmetry adapted cluster)/SAC-CI (configuration interaction) method. The results reproduced well the experimentally determined excitation energies. The reduction of the outer double bonds in the porphine ring in the order of FBP, FBC, and FBBC causes a breakdown of the symmetry and a narrowing of the HOMO- LUMO gap, which result in a red shift of the Qx band and an increase of its intensity. In the change from Pheo a to Chlo a, the Mg coordination reduces the quasidegeneracy in the Qx state and then increases the spectral intensity. The disappearance of the Qy humps from the absorption spectrum of Pheo a, compared with that of Chlo a, is due to the red shift of the Qy state. Introduction Many biological systems contain porphyrins, chlorins, and bacteriochlorins.1,2 These compounds often take an important part in biochemical reactions, such as light absorption, electron transfer,1 and oxygen transport and storage.2 Because of their scientific importance, they have been the subject of a wide variety of studies. -

Seven Novel Genetic Variants in a North Indian Cohort with Classical Homocystinuria Rajdeep Kaur1, Savita V
www.nature.com/scientificreports OPEN Seven novel genetic variants in a North Indian cohort with classical homocystinuria Rajdeep Kaur1, Savita V. Attri1*, Arushi G. Saini1, Naveen Sankhyan1, Satwinder Singh1, Mohammed Faruq2, V. L. Ramprasad3, Sheetal Sharda3 & Sakthivel Murugan3 Classical homocystinuria is the most common cause of isolated homocystinuria. The variants of the CBS gene remain unidentifed in Indian children with this disorder. Based on the hallmark clinical features, family history, and/or biochemical clues for classical homocystinuria, 16 children below the age of 18 years were evaluated by Sanger sequencing of the coding exons of CBS gene with fanking intronic regions. The common C677T variant of the MTHFR gene was also screened by restriction fragment length polymorphism. Fifteen children were clinically suspected of having classical homocystinuria and one asymptomatic child with positive family history. Only seven children had biochemical features of classical homocystinuria. Sanger sequencing of the CBS gene confrmed 15 diferent pathogenic or likely pathogenic variants in 14 cases. Of these, seven variants were novel (three frameshift deletions, two nonsense, one missense, one splice site variant) and were predicted to be deleterious by Mutation Taster software. Seven cases were homozygous, another six were compound heterozygous, and one case was single heterozygous in the study. None of the three most frequent mutations reported worldwide viz., I278T, G307S, and IVS 11-2A>C were found in our cohort. No variants were detected in the exons 2, 8, 12, and 14 as compared to reported literature. Eleven out of 15 variants were associated with the conserved catalytic domain of the CBS polypeptide.