Treatable Inborn Errors of Metabolism Presenting As Cerebral Palsy Mimics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hyperammonemia in Review: Pathophysiology, Diagnosis, and Treatment
Pediatr Nephrol DOI 10.1007/s00467-011-1838-5 EDUCATIONAL REVIEW Hyperammonemia in review: pathophysiology, diagnosis, and treatment Ari Auron & Patrick D. Brophy Received: 23 September 2010 /Revised: 9 January 2011 /Accepted: 12 January 2011 # IPNA 2011 Abstract Ammonia is an important source of nitrogen and is the breakdown and catabolism of dietary and bodily proteins, required for amino acid synthesis. It is also necessary for respectively. In healthy individuals, amino acids that are not normal acid-base balance. When present in high concentra- needed for protein synthesis are metabolized in various tions, ammonia is toxic. Endogenous ammonia intoxication chemical pathways, with the rest of the nitrogen waste being can occur when there is impaired capacity of the body to converted to urea. Ammonia is important for normal animal excrete nitrogenous waste, as seen with congenital enzymatic acid-base balance. During exercise, ammonia is produced in deficiencies. A variety of environmental causes and medica- skeletal muscle from deamination of adenosine monophos- tions may also lead to ammonia toxicity. Hyperammonemia phate and amino acid catabolism. In the brain, the latter refers to a clinical condition associated with elevated processes plus the activity of glutamate dehydrogenase ammonia levels manifested by a variety of symptoms and mediate ammonia production. After formation of ammonium signs, including significant central nervous system (CNS) from glutamine, α-ketoglutarate, a byproduct, may be abnormalities. Appropriate and timely management requires a degraded to produce two molecules of bicarbonate, which solid understanding of the fundamental pathophysiology, are then available to buffer acids produced by dietary sources. differential diagnosis, and treatment approaches available. -

Alternative Splicing of Bicistronic MOCS1 Defines a Novel Mitochondrial Protein
bioRxiv preprint doi: https://doi.org/10.1101/429183; this version posted September 27, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Alternative splicing of bicistronic MOCS1 defines a novel mitochondrial protein maturation mechanism Simon Julius Mayr1, Juliane Röper1 and Guenter Schwarz1,2,3,* 1 Institute of Biochemistry, Department of Chemistry, University of Cologne, 50674 Cologne, Germany 2 Center for Molecular Medicine Cologne, University of Cologne, 50931 Cologne, Germany 3 Cluster of Excellence Cluster in Aging Research, University of Cologne, 50931 Cologne, Germany * correspondence: [email protected] Running Title: Mitochondrial MOCS1 protein maturation bioRxiv preprint doi: https://doi.org/10.1101/429183; this version posted September 27, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract Molybdenum cofactor biosynthesis is a conserved multistep pathway. The first step, the conversion of GTP to cyclic pyranopterin monophosphate (cPMP), requires bicsistronic MOCS1. Alternative splicing of MOCS1 in exons 1 and 9 produces four different N-terminal and three different C-terminal products (type I-III). Type I splicing results in bicistronic transcripts with two open reading frames, of which only the first, MOCS1A, is translated, whereas type II/III splicing produces two-domain MOCS1AB proteins. Here, we report and characterize the mitochondrial translocation of alternatively spliced MOCS1 proteins. While MOCS1A requires exon 1a for mitochondrial translocation, MOCS1AB variants target to mitochondria via an internal motif overriding the N-terminal targeting signal. -

The Epidemiology of the Cerebral Palsies
Clinics in Developmental Medicine No. 87 The Epidemiology of the Cerebral Palsies Edited by FIONA STANLEY EVA ALBERMAN 1984 Spastics International Medical Publications OXFORD: Blackwell Scientific Publications Ltd. PHILADELPHIA: J. B. Lippincott Co. CHAPTER 11 Prenatal and Perinatal Risk Factors in a Survey of 681 Swedish Cases BENGT and GUDRUN HAGBERG I, that am curtail'd of this fair proportion, Cheated of feature by dissembling nature, , Deform'd, unfinish'd, sent before my time Into this breathing world, scarce half made up, And that so lamely and unfashionable That dogs bark at me, as I halt by them. Shakespeare, Richard III Introduction The aim of this chapter is to try and shed light on more specific aspects of the main groups of prenatal causes and risk factors for cerebral palsy, their mutual importance, and particularly their relationship to superimposed detrimental perinatal events. This survey is based on an investigation of 681 cases born in Sweden from 1959 to 1976. In our original retrospective analysis of causes of cerebral palsy (Hagberg et al. 1975a), it was found necessary to make certain generalisations about the aetiological groupings. Only the risk factor that was considered to be the predominating possible cause was used for classification. There is no doubt that this oversimplifies the issue as it neglects the complex network of different interacting detrimental risk factors that are present in the majority of cases, and in all probability underlie the development of brain lesions. Definitions For the purpose of the Swedish investigation, the following definition of cerebral palsy was used: a non-progressive 'disorder of movement and posture due to a defect or lesion of the immature brain' (Bax 1964). -
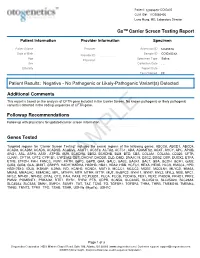
PDF Document Created by Pdffiller
Patient: 1234567843314948-COtGx0053 CLIA ID#: 11D2066426 Larry Hung, MD, Laboratory Director GxTM Carrier Screen Testing Report Patient Information Provider Information Specimen Patient Name Haley Papevies Provider Harbin Clinic Women's Accession ID 1234567843314948 Center Cartersville Date of Birth Apr 16, 1998 Sample ID COtGx0053XX Provider ID 1124488556 Age 19 Specimen Type Saliva Physician Vicki Yates Sex female Collection Date Jul 20, 2017 Ethnicity Report Date Aug 5, 2017 Test Ordered CF Patient Results: Negative - No Pathogenic or Likely-Pathogenic Variant(s) Detected Additional Comments This report is based on the analysis of CFTR gene included in the Carrier Screen. No known pathogenic or likely pathogenic variant(s) detected in the coding sequences of CFTR gene. Followup Recommendations Follow up with physicians for updated carrier screen information. The sequencing for CFTR gene was carried out with the other genes included in the Carrier Screen Testing (listed below). The analysis of the other genes in the Carrier Screen could be ordered through your physicians. Genes Tested Targeted regions for “Carrier Screen Testing” includes the exonic regions of the following genes: ABCC8, ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACSF3, ACTA2, ACTC1, ADA, ADAMTS2, AGXT, AHCY, APC, APOB, ARG1, ASL, ASPA, ASS1, ATP7B, AUH, BCKDHA, BBS2, BCKDHB, BLM, BTD, CBS, COL3A1, COL4A3, CD320, CFTR, CLRN1, CPT1A, CPT2, CYP1B1, CYP21A2, DBT, DHCR7, DHDDS, DLD, DMD, DNAJC19, DSC2, DSG2, DSP, DUOX2, ETFA, ETFB, ETFDH, FAH, FANCC, FBN1, -

Supplement 1 Overview of Dystonia Genes
Supplement 1 Overview of genes that may cause dystonia in children and adolescents Gene (OMIM) Disease name/phenotype Mode of inheritance 1: (Formerly called) Primary dystonias (DYTs): TOR1A (605204) DYT1: Early-onset generalized AD primary torsion dystonia (PTD) TUBB4A (602662) DYT4: Whispering dystonia AD GCH1 (600225) DYT5: GTP-cyclohydrolase 1 AD deficiency THAP1 (609520) DYT6: Adolescent onset torsion AD dystonia, mixed type PNKD/MR1 (609023) DYT8: Paroxysmal non- AD kinesigenic dyskinesia SLC2A1 (138140) DYT9/18: Paroxysmal choreoathetosis with episodic AD ataxia and spasticity/GLUT1 deficiency syndrome-1 PRRT2 (614386) DYT10: Paroxysmal kinesigenic AD dyskinesia SGCE (604149) DYT11: Myoclonus-dystonia AD ATP1A3 (182350) DYT12: Rapid-onset dystonia AD parkinsonism PRKRA (603424) DYT16: Young-onset dystonia AR parkinsonism ANO3 (610110) DYT24: Primary focal dystonia AD GNAL (139312) DYT25: Primary torsion dystonia AD 2: Inborn errors of metabolism: GCDH (608801) Glutaric aciduria type 1 AR PCCA (232000) Propionic aciduria AR PCCB (232050) Propionic aciduria AR MUT (609058) Methylmalonic aciduria AR MMAA (607481) Cobalamin A deficiency AR MMAB (607568) Cobalamin B deficiency AR MMACHC (609831) Cobalamin C deficiency AR C2orf25 (611935) Cobalamin D deficiency AR MTRR (602568) Cobalamin E deficiency AR LMBRD1 (612625) Cobalamin F deficiency AR MTR (156570) Cobalamin G deficiency AR CBS (613381) Homocysteinuria AR PCBD (126090) Hyperphelaninemia variant D AR TH (191290) Tyrosine hydroxylase deficiency AR SPR (182125) Sepiaterine reductase -

Newborn Screening Laboratory Manual of Services
Newborn Screening Laboratory Manual of Services Test Panel: Please see the following links for a detailed description of testing in the Newborn Screening section. Information about the Newborn Screening program is available here. Endocrine Disorders Congenital adrenal hyperplasia (CAH) Congenital hypothyroidism (TSH) Hemoglobinopathies Sickle cell disease (FS) Alpha (Barts) Sickle βeta Thalassemia (FSA) Other sickling hemoglobinopathies such as: FAS FAC FAD FAE Homozygous conditions such as: FC FD FE Metabolic Disorders Biotinidase deficiency Galactosemia Cystic fibrosis (CF) first tier screening for elevated immunoreactive trypsinogen (IRT) Cystic fibrosis second tier genetic mutation analysis on the top 4% IRT concentrations. Current alleles detected : F508del, I507del, G542X, G85E, R117H, 621+1G->T, 711+1G->T, R334W, R347P, A455E, 1717-1G->A, R560T, R553X, G551D, 1898+1G->A, 2184delA, 2789+5G->A, 3120+1G->A, R1162X, 3659delC, 3849+10kbC->T, W1282X, N1303K, IVS polyT T5/T7/T9 *Currently validating a mutation panel that includes the above alleles in addition to the following: 1078delT, Y122X, 394delTT, R347H, M1101K, S1255X, 1898+5G->T, 2183AA->G, 2307insA, Y1092X, 3876delA, 3905insT, S549N, S549R_1645A->C, S549R-1647T->G, S549R-1647T->G, V520F, A559T, 1677delTA, 2055del9->A, 2143delT, 3199del6, 406-1G->A, 935delA, D1152H, CFTRdele2, E60X, G178R, G330X, K710X, L206W, Q493X, Q890X, R1066C, R1158X, R75X, S1196X, W1089X, G1244E, G1349D, G551S, R560KT, S1251N, S1255P Amino acid disorders Phenylketonuria (PKU) / Hyperphenylalaninemia Maple -

Disorders Included in the Newborn Screening Panel Disorders
Disorders Included in the Newborn Screening Panel Disorders Detected by Tandem Mass Spectrometry Acylcarnitine Profile Amino Acid Profile Fatty Acid Oxidation Disorders Amino Acid Disorders Carnitine/Acylcarnitine Translocase Deficiency Argininemia 1 Carnitine Palmitoyl Transferase Deficiency Type I Argininosuccinic Aciduria 1 3-Hydroxy Long Chain Acyl-CoA Dehydrogenase 5-Oxoprolinuria 1 Deficiency Carbamoylphosphate Synthetase Deficiency 1 2,4-Dienoyl-CoA Reductase Deficiency Citrullinemia Medium Chain Acyl-CoA Dehydrogenase Deficiency Homocystinuria Multiple Acyl-CoA Dehydrogenase Deficiency Hypermethioninemia Neonatal Carnitine Palmitoyl Transferase Deficiency Hyperammonemia, Hyperornithinemia, Homocitrullinuria Type II Syndrome1 1 Short Chain Acyl-CoA Dehydrogenase Deficiency Hyperornithinemia with Gyral Atrophy Short Chain Hydroxy Acyl-CoA Dehydrogenase Maple Syrup Urine Disease Deficiency Phenylketonuria Trifunctional Protein Deficiency Classical/Hyperphenylalaninemia Very Long Chain Acyl-CoA Dehydrogenase Deficiency Biopterin Cofactor Deficiencies Tyrosinemia Organic Acid Disorders Transient Neonatal Tyrosinemia 2 Tyrosinemia Type I 3-Hydroxy-3-Methylglutaryl-CoA Lyase Deficiency Tyrosinemia Type II Glutaric Acidemia Type I Tyrosinemia Type III Isobutyryl-CoA Dehydrogenase Deficiency Isovaleric Acidemia 2-Methylbutyryl-CoA Dehydrogenase Deficiency 3-Methylcrotonyl-CoA Carboxylase Deficiency Other Observations 3-Methylglutaconyl-CoA Hydratase Deficiency Methylmalonic Acidemias Hyperalimentation Methylmalonyl-CoA Mutase Deficiency -

Birth Prevalence of Disorders Detectable Through Newborn Screening by Race/Ethnicity
©American College of Medical Genetics and Genomics ORIGINAL RESEARCH ARTICLE Birth prevalence of disorders detectable through newborn screening by race/ethnicity Lisa Feuchtbaum, DrPH, MPH1, Jennifer Carter, MPH2, Sunaina Dowray, MPH2, Robert J. Currier, PhD1 and Fred Lorey, PhD1 Purpose: The purpose of this study was to describe the birth prev- Conclusion: The California newborn screening data offer a alence of genetic disorders among different racial/ethnic groups unique opportunity to explore the birth prevalence of many through population-based newborn screening data. genetic dis orders across a wide spectrum of racial/ethnicity classifications. The data demonstrate that racial/ethnic subgroups Methods: Between 7 July 2005 and 6 July 2010 newborns in Cali- of the California newborn population have very different patterns fornia were screened for selected metabolic, endocrine, hemoglobin, of heritable disease expression. Determining the birth prevalence and cystic fibrosis disorders using a blood sample collected via heel of these disorders in California is a first step to understanding stick. The race and ethnicity of each newborn was self-reported by the short- and long-term medical and treatment needs faced by the mother at the time of specimen collection. affected communities, especially those groups that are impacted by Results: Of 2,282,138 newborns screened, the overall disorder detec- more severe disorders. tion rate was 1 in 500 births. The disorder with the highest prevalence Genet Med 2012:14(11):937–945 among all groups was primary congenital hypothyroidism (1 in 1,706 births). Birth prevalence for specific disorders varied widely among Key Words: birth prevalence; disorders; newborn screening; race different racial/ethnic groups. -

Abstracts from the 9Th Biennial Scientific Meeting of The
International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):15 DOI 10.1186/s13633-017-0054-x MEETING ABSTRACTS Open Access Abstracts from the 9th Biennial Scientific Meeting of the Asia Pacific Paediatric Endocrine Society (APPES) and the 50th Annual Meeting of the Japanese Society for Pediatric Endocrinology (JSPE) Tokyo, Japan. 17-20 November 2016 Published: 28 Dec 2017 PS1 Heritable forms of primary bone fragility in children typically lead to Fat fate and disease - from science to global policy a clinical diagnosis of either osteogenesis imperfecta (OI) or juvenile Peter Gluckman osteoporosis (JO). OI is usually caused by dominant mutations affect- Office of Chief Science Advsor to the Prime Minister ing one of the two genes that code for two collagen type I, but a re- International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):PS1 cessive form of OI is present in 5-10% of individuals with a clinical diagnosis of OI. Most of the involved genes code for proteins that Attempts to deal with the obesity epidemic based solely on adult be- play a role in the processing of collagen type I protein (BMP1, havioural change have been rather disappointing. Indeed the evidence CREB3L1, CRTAP, LEPRE1, P4HB, PPIB, FKBP10, PLOD2, SERPINF1, that biological, developmental and contextual factors are operating SERPINH1, SEC24D, SPARC, from the earliest stages in development and indeed across generations TMEM38B), or interfere with osteoblast function (SP7, WNT1). Specific is compelling. The marked individual differences in the sensitivity to the phenotypes are caused by mutations in SERPINF1 (recessive OI type obesogenic environment need to be understood at both the individual VI), P4HB (Cole-Carpenter syndrome) and SEC24D (‘Cole-Carpenter and population level. -

Inherited Metabolic Disease
Inherited metabolic disease Dr Neil W Hopper SRH Areas for discussion • Introduction to IEMs • Presentation • Initial treatment and investigation of IEMs • Hypoglycaemia • Hyperammonaemia • Other presentations • Management of intercurrent illness • Chronic management Inherited Metabolic Diseases • Result from a block to an essential pathway in the body's metabolism. • Huge number of conditions • All rare – very rare (except for one – 1:500) • Presentation can be non-specific so index of suspicion important • Mostly AR inheritance – ask about consanguinity Incidence (W. Midlands) • Amino acid disorders (excluding phenylketonuria) — 18.7 per 100,000 • Phenylketonuria — 8.1 per 100,000 • Organic acidemias — 12.6 per 100,000 • Urea cycle diseases — 4.5 per 100,000 • Glycogen storage diseases — 6.8 per 100,000 • Lysosomal storage diseases — 19.3 per 100,000 • Peroxisomal disorders — 7.4 per 100,000 • Mitochondrial diseases — 20.3 per 100,000 Pathophysiological classification • Disorders that result in toxic accumulation – Disorders of protein metabolism (eg, amino acidopathies, organic acidopathies, urea cycle defects) – Disorders of carbohydrate intolerance – Lysosomal storage disorders • Disorders of energy production, utilization – Fatty acid oxidation defects – Disorders of carbohydrate utilization, production (ie, glycogen storage disorders, disorders of gluconeogenesis and glycogenolysis) – Mitochondrial disorders – Peroxisomal disorders IMD presentations • ? IMD presentations • Screening – MCAD, PKU • Progressive unexplained neonatal -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Cerebral Palsy the ABC's of CP
Cerebral Palsy The ABC’s of CP Toni Benton, M.D. Continuum of Care Project UNM HSC School of Medicine April 20, 2006 Cerebral Palsy Outline I. Definition II. Incidence, Epidemiology and Distribution III. Etiology IV. Types V. Medical Management VI. Psychosocial Issues VII. Aging Cerebral Palsy-Definition Cerebral palsy is a symptom complex, (not a disease) that has multiple etiologies. CP is a disorder of tone, posture or movement due to a lesion in the developing brain. Lesion results in paralysis, weakness, incoordination or abnormal movement Not contagious, no cure. It is static, but it symptoms may change with maturation Cerebral Palsy Brain damage Occurs during developmental period Motor dysfunction Not Curable Non-progressive (static) Any regression or deterioration of motor or intellectual skills should prompt a search for a degenerative disease Therapy can help improve function Cerebral Palsy There are 2 major types of CP, depending on location of lesions: Pyramidal (Spastic) Extrapyramidal There is overlap of both symptoms and anatomic lesions. The pyramidal system carries the signal for muscle contraction. The extrapyramidal system provides regulatory influences on that contraction. Cerebral Palsy Types of brain damage Bleeding Brain malformation Trauma to brain Lack of oxygen Infection Toxins Unknown Epidemiology The overall prevalence of cerebral palsy ranges from 1.5 to 2.5 per 1000 live births. The overall prevalence of CP has remained stable since the 1960’s. Speculations that the increased survival of the VLBW preemies would cause a rise in the prevalence of CP have proven wrong. Likewise the expected decrease in CP as a result of C-section and fetal monitoring has not happened.