Investigations Into the Early Steps of Cobalamin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
PDF Document Created by Pdffiller
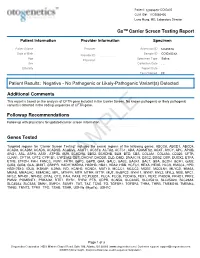
Patient: 1234567843314948-COtGx0053 CLIA ID#: 11D2066426 Larry Hung, MD, Laboratory Director GxTM Carrier Screen Testing Report Patient Information Provider Information Specimen Patient Name Haley Papevies Provider Harbin Clinic Women's Accession ID 1234567843314948 Center Cartersville Date of Birth Apr 16, 1998 Sample ID COtGx0053XX Provider ID 1124488556 Age 19 Specimen Type Saliva Physician Vicki Yates Sex female Collection Date Jul 20, 2017 Ethnicity Report Date Aug 5, 2017 Test Ordered CF Patient Results: Negative - No Pathogenic or Likely-Pathogenic Variant(s) Detected Additional Comments This report is based on the analysis of CFTR gene included in the Carrier Screen. No known pathogenic or likely pathogenic variant(s) detected in the coding sequences of CFTR gene. Followup Recommendations Follow up with physicians for updated carrier screen information. The sequencing for CFTR gene was carried out with the other genes included in the Carrier Screen Testing (listed below). The analysis of the other genes in the Carrier Screen could be ordered through your physicians. Genes Tested Targeted regions for “Carrier Screen Testing” includes the exonic regions of the following genes: ABCC8, ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACSF3, ACTA2, ACTC1, ADA, ADAMTS2, AGXT, AHCY, APC, APOB, ARG1, ASL, ASPA, ASS1, ATP7B, AUH, BCKDHA, BBS2, BCKDHB, BLM, BTD, CBS, COL3A1, COL4A3, CD320, CFTR, CLRN1, CPT1A, CPT2, CYP1B1, CYP21A2, DBT, DHCR7, DHDDS, DLD, DMD, DNAJC19, DSC2, DSG2, DSP, DUOX2, ETFA, ETFB, ETFDH, FAH, FANCC, FBN1, -

Abstracts from the 9Th Biennial Scientific Meeting of The
International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):15 DOI 10.1186/s13633-017-0054-x MEETING ABSTRACTS Open Access Abstracts from the 9th Biennial Scientific Meeting of the Asia Pacific Paediatric Endocrine Society (APPES) and the 50th Annual Meeting of the Japanese Society for Pediatric Endocrinology (JSPE) Tokyo, Japan. 17-20 November 2016 Published: 28 Dec 2017 PS1 Heritable forms of primary bone fragility in children typically lead to Fat fate and disease - from science to global policy a clinical diagnosis of either osteogenesis imperfecta (OI) or juvenile Peter Gluckman osteoporosis (JO). OI is usually caused by dominant mutations affect- Office of Chief Science Advsor to the Prime Minister ing one of the two genes that code for two collagen type I, but a re- International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):PS1 cessive form of OI is present in 5-10% of individuals with a clinical diagnosis of OI. Most of the involved genes code for proteins that Attempts to deal with the obesity epidemic based solely on adult be- play a role in the processing of collagen type I protein (BMP1, havioural change have been rather disappointing. Indeed the evidence CREB3L1, CRTAP, LEPRE1, P4HB, PPIB, FKBP10, PLOD2, SERPINF1, that biological, developmental and contextual factors are operating SERPINH1, SEC24D, SPARC, from the earliest stages in development and indeed across generations TMEM38B), or interfere with osteoblast function (SP7, WNT1). Specific is compelling. The marked individual differences in the sensitivity to the phenotypes are caused by mutations in SERPINF1 (recessive OI type obesogenic environment need to be understood at both the individual VI), P4HB (Cole-Carpenter syndrome) and SEC24D (‘Cole-Carpenter and population level. -

Oral Presentations
Journal of Inherited Metabolic Disease (2018) 41 (Suppl 1):S37–S219 https://doi.org/10.1007/s10545-018-0233-9 ABSTRACTS Oral Presentations PARALLEL SESSION 1A: Clycosylation and cardohydrate disorders O-002 Link between glycemia and hyperlipidemia in Glycogen Storage O-001 Disease type Ia Hoogerland J A1, Hijmans B S1, Peeks F1, Kooijman S3, 4, Bos T2, Fertility in classical galactosaemia, N-glycan, hormonal and inflam- Bleeker A1, Van Dijk T H2, Wolters H1, Havinga R1,PronkACM3, 4, matory gene expression interactions Rensen P C N3, 4,MithieuxG5, 6, Rajas F5, 6, Kuipers F1, 2,DerksTGJ1, Reijngoud D1,OosterveerMH1 Colhoun H O1,Rubio-GozalboME2,BoschAM3, Knerr I4,DawsonC5, Brady J J6,GalliganM8,StepienKM9, O'Flaherty R O7,MossC10, 1Dep Pediatrics, CLDM, Univ of Groningen, Groningen, Barker P11, Fitzgibbon M C6, Doran P8,TreacyEP1, 4, 9 Netherlands, 2Lab Med, CLDM, Univ of Groningen, Groningen, Netherlands, 3Dep of Med, Div of Endocrinology, LUMC, Leiden, 1Dept Paediatrics, Trinity College Dublin, Dublin, Ireland, 2Dept Paeds and Netherlands, 4Einthoven Lab Exp Vasc Med, LUMC, Leiden, Clin Genetics, UMC, Maastricht, Netherlands, 3Dept Paediatrics, AMC, Netherlands, 5Institut Nat Sante et Recherche Med, Lyon, Amsterdam, Netherlands, 4NCIMD, TSCUH, Dublin, Ireland, 5Dept France, 6Univ Lyon 1, Villeurbanne, France Endocrinology, NHS Foundation Trust, Birmingham, United Kingdom, 6Dept Clin Biochem, MMUH, Dublin, Ireland, 7NIBRT Glycoscience, Background: Glycogen Storage Disease type Ia (GSD Ia) is an NIBRT, Dublin, Ireland, 8UCDCRC,UCD,Dublin,Ireland,9NCIMD, inborn error of glucose metabolism characterized by fasting hypo- MMUH, Dublin, Ireland, 10Conway Institute, UCD, Dublin, Ireland, glycemia, hyperlipidemia and fatty liver disease. We have previ- 11CBAL, NHS Foundation, Cambridge, United Kingdom ously reported considerable heterogeneity in circulating triglycer- ide levels between individual GSD Ia patients, a phenomenon that Background: Classical Galactosaemia (CG) is caused by deficiency of is poorly understood. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Itemised List of Supplemental Material 1. Supplemental Materials And
Itemised list of Supplemental Material 1. Supplemental Materials and Methods 2. Supplemental References 3. Supplemental Table S1. Summary of pathological abnormalities observed with variable penetrance in L597VBraf-expressing mice. 4. Supplemental Figures S1-7. Fig. S1: Multiplex PCR genotyping of Braf+/LSL-L597V mouse ear samples Fig. S2: H&E-stained sections of benign growths Fig. S3: PCR to detect Cre-mediated recombination in MEFs Fig. S4: Characterisation of the Erk pathway in MEFs: Dusp 6 knockdown and p90RSK phosphorylation Fig. S5: PCR to detection Cre-mediated recombination in lung Fig. S6: Expression of D-type cyclins in primary MEFs. Fig. S7: Heterodimer formation between L597VBRAF and CRAF in HEK293T cells. 5. Supplemental Table S2. Summary of microarray data 6. Supplemental Table S3. Genes whose expression is significantly altered in V600EBraf, G12DKras and L597VBraf/G12DKras MEFs. 7. Supplemental Table S4. Genes whose expression is altered in L597VBraf/G12DKras MEFs but not G12DKras or V600EBraf MEFs Supplemental Materials and Methods Transfection of HEK293T cells HEK293T cells were cultured in DMEM with 10% FCS and penicillin/streptomycin and transfected with lipofectamine 2000 using conditions recommended by the manufacturer (Invitrogen). Cells were either mock transfected or transfected with myc-tagged expression vectors for human WTBRAF or L597VBRAF. 48 hours after transfection, cells were harvested and protein lysates generated by previously reported methods (Huser et al. 2001). BRAF was immunoprecipitated using the BRAF antibody (Santa Cruz Inc. #SC-5284). Immunoblotting Protein lysates were prepared by previously published methods (Huser et al. 2001). Antibodies used were as follows: Cyclin d1 (Cell Signaling Tech. #2922), Cyclin d2 (Santa Cruz Inc. -

Molecular Diagnostic Requisition
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 MOLECULAR DIAGNOSTIC REQUISITION PATIENT INFORMATION SAMPLE INFORMATION NAME: DATE OF COLLECTION: / / LAST NAME FIRST NAME MI MM DD YY HOSPITAL#: ACCESSION#: DATE OF BIRTH: / / GENDER (Please select one): FEMALE MALE MM DD YY SAMPLE TYPE (Please select one): ETHNIC BACKGROUND (Select all that apply): UNKNOWN BLOOD AFRICAN AMERICAN CORD BLOOD ASIAN SKELETAL MUSCLE ASHKENAZIC JEWISH MUSCLE EUROPEAN CAUCASIAN -OR- DNA (Specify Source): HISPANIC NATIVE AMERICAN INDIAN PLACE PATIENT STICKER HERE OTHER JEWISH OTHER (Specify): OTHER (Please specify): REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: INDICATION FOR STUDY SYMPTOMATIC (Summarize below.): *FAMILIAL MUTATION/VARIANT ANALYSIS: COMPLETE ALL FIELDS BELOW AND ATTACH THE PROBAND'S REPORT. GENE NAME: ASYMPTOMATIC/POSITIVE FAMILY HISTORY: (ATTACH FAMILY HISTORY) MUTATION/UNCLASSIFIED VARIANT: RELATIONSHIP TO PROBAND: THIS INDIVIDUAL IS CURRENTLY: SYMPTOMATIC ASYMPTOMATIC *If family mutation is known, complete the FAMILIAL MUTATION/ VARIANT ANALYSIS section. NAME OF PROBAND: ASYMPTOMATIC/POPULATION SCREENING RELATIONSHIP TO PROBAND: OTHER (Specify clinical findings below): BMGL LAB#: A COPY OF ORIGINAL RESULTS ATTACHED IF PROBAND TESTING WAS PERFORMED AT ANOTHER LAB, CALL TO DISCUSS PRIOR TO SENDING SAMPLE. A POSITIVE CONTROL MAY BE REQUIRED IN SOME CASES. REQUIRED: NEW YORK STATE PHYSICIAN SIGNATURE OF CONSENT I certify that the patient specified above and/or their legal guardian has been informed of the benefits, risks, and limitations of the laboratory test(s) requested. -

Natalis Information Sheet V03
Sema4 Natalis Clinical significance of panel Sema4 has designed and validated Natalis, a supplemental newborn screening panel offered for newborns, infants, and young children. This test may be offered to parents as an addition to the state mandated newborn screening that their child received at birth. This panel includes next-generation sequencing, targeting genotyping, and multiplex ligation-dependent probe amplification in a total of 166 genes to screen for 193 conditions that have onset in infancy or early childhood and for which there is treatment or medical management that, when administered early in an infant or child’s life, will significantly improve the clinical outcome. Conditions included in this panel were curated based on criteria such as: inclusion on current state mandated newborn screening panels, onset of symptoms occurring <10 years of age, evidence of high penetrance (>80%), and availability of a treatment or improvement in life due to early intervention. Sema4 has also designed and validated a pediatric pharmacogenetic (PGx) genotyping panel as an adjunct test to the Natalis assay. This panel includes 10 genes and 41 sequence variants involved in drug response variability. The genes and variants in the PGx genotyping panel inform on more than 40 medications that can be prescribed during childhood. Currently, there is evidence supporting the clinical utility of testing for certain PGx variants for which there are genotype-directed clinical practice recommendations for selected gene/drug pairs. Approximately 95% of all individuals will carry at least one clinically actionable variant in the PGx panel. Testing methods, sensitivity, and limitations A cheek swab, saliva sample, or blood sample is provided by the child and a biological parent. -

Seven Novel Genetic Variants in a North Indian Cohort with Classical Homocystinuria Rajdeep Kaur1, Savita V
www.nature.com/scientificreports OPEN Seven novel genetic variants in a North Indian cohort with classical homocystinuria Rajdeep Kaur1, Savita V. Attri1*, Arushi G. Saini1, Naveen Sankhyan1, Satwinder Singh1, Mohammed Faruq2, V. L. Ramprasad3, Sheetal Sharda3 & Sakthivel Murugan3 Classical homocystinuria is the most common cause of isolated homocystinuria. The variants of the CBS gene remain unidentifed in Indian children with this disorder. Based on the hallmark clinical features, family history, and/or biochemical clues for classical homocystinuria, 16 children below the age of 18 years were evaluated by Sanger sequencing of the coding exons of CBS gene with fanking intronic regions. The common C677T variant of the MTHFR gene was also screened by restriction fragment length polymorphism. Fifteen children were clinically suspected of having classical homocystinuria and one asymptomatic child with positive family history. Only seven children had biochemical features of classical homocystinuria. Sanger sequencing of the CBS gene confrmed 15 diferent pathogenic or likely pathogenic variants in 14 cases. Of these, seven variants were novel (three frameshift deletions, two nonsense, one missense, one splice site variant) and were predicted to be deleterious by Mutation Taster software. Seven cases were homozygous, another six were compound heterozygous, and one case was single heterozygous in the study. None of the three most frequent mutations reported worldwide viz., I278T, G307S, and IVS 11-2A>C were found in our cohort. No variants were detected in the exons 2, 8, 12, and 14 as compared to reported literature. Eleven out of 15 variants were associated with the conserved catalytic domain of the CBS polypeptide. -

Downloaded from the App Store and Nucleobase, Nucleotide and Nucleic Acid Metabolism 7 Google Play
Hoytema van Konijnenburg et al. Orphanet J Rare Dis (2021) 16:170 https://doi.org/10.1186/s13023-021-01727-2 REVIEW Open Access Treatable inherited metabolic disorders causing intellectual disability: 2021 review and digital app Eva M. M. Hoytema van Konijnenburg1†, Saskia B. Wortmann2,3,4†, Marina J. Koelewijn2, Laura A. Tseng1,4, Roderick Houben6, Sylvia Stöckler‑Ipsiroglu5, Carlos R. Ferreira7 and Clara D. M. van Karnebeek1,2,4,8* Abstract Background: The Treatable ID App was created in 2012 as digital tool to improve early recognition and intervention for treatable inherited metabolic disorders (IMDs) presenting with global developmental delay and intellectual disabil‑ ity (collectively ‘treatable IDs’). Our aim is to update the 2012 review on treatable IDs and App to capture the advances made in the identifcation of new IMDs along with increased pathophysiological insights catalyzing therapeutic development and implementation. Methods: Two independent reviewers queried PubMed, OMIM and Orphanet databases to reassess all previously included disorders and therapies and to identify all reports on Treatable IDs published between 2012 and 2021. These were included if listed in the International Classifcation of IMDs (ICIMD) and presenting with ID as a major feature, and if published evidence for a therapeutic intervention improving ID primary and/or secondary outcomes is avail‑ able. Data on clinical symptoms, diagnostic testing, treatment strategies, efects on outcomes, and evidence levels were extracted and evaluated by the reviewers and external experts. The generated knowledge was translated into a diagnostic algorithm and updated version of the App with novel features. Results: Our review identifed 116 treatable IDs (139 genes), of which 44 newly identifed, belonging to 17 ICIMD categories. -

Treatable Inborn Errors of Metabolism Presenting As Cerebral Palsy Mimics
Leach et al. Orphanet Journal of Rare Diseases 2014, 9:197 http://www.ojrd.com/content/9/1/197 RESEARCH Open Access Treatable inborn errors of metabolism presenting as cerebral palsy mimics: systematic literature review Emma L Leach1,2, Michael Shevell3,4,KristinBowden2, Sylvia Stockler-Ipsiroglu2,5,6 and Clara DM van Karnebeek2,5,6,7,8* Abstract Background: Inborn errors of metabolism (IEMs) have been anecdotally reported in the literature as presenting with features of cerebral palsy (CP) or misdiagnosed as ‘atypical CP’. A significant proportion is amenable to treatment either directly targeting the underlying pathophysiology (often with improvement of symptoms) or with the potential to halt disease progression and prevent/minimize further damage. Methods: We performed a systematic literature review to identify all reports of IEMs presenting with CP-like symptoms before 5 years of age, and selected those for which evidence for effective treatment exists. Results: We identified 54 treatable IEMs reported to mimic CP, belonging to 13 different biochemical categories. A further 13 treatable IEMs were included, which can present with CP-like symptoms according to expert opinion, but for which no reports in the literature were identified. For 26 of these IEMs, a treatment is available that targets the primary underlying pathophysiology (e.g. neurotransmitter supplements), and for the remainder (n = 41) treatment exerts stabilizing/preventative effects (e.g. emergency regimen). The total number of treatments is 50, and evidence varies for the various treatments from Level 1b, c (n = 2); Level 2a, b, c (n = 16); Level 4 (n = 35); to Level 4–5 (n = 6); Level 5 (n = 8). -

Selection Signatures Scan in Several Italian Sheep Breeds Identifies Genes Influencing Micronutrient Metabolism S
Selection signatures scan in several Italian sheep breeds identifies genes influencing micronutrient metabolism S. Sorbolini1, C. Dimauro1, M. Cellesi1, F. Pilla2, N.P.P. Macciotta1 and the BIOVITA Consortium. 1Università di Sassari, Dipartimento di Agraria, Viale Italia 39, 07100 Sassari, Italy. 1Università del Studi del Molise, Dipartimento Agricoltura Ambiente Alimenti, Via F. de Sanctis s.n.c. 86100 Campobasso, Italy. [email protected] (Corresponding author) Summary Animal physiological functions involve enzymes and cofactors. Many of these substances can not be synthesized by the body, but derive from the diet. An example are micronutrients, that strongly affect production performance, whose requirements are often met by the farmers by adding supplements to the diet. The aim of this study was to investigate the genetic variability of Italian sheep breeds searching for possible selective sweeps that harbor genes involved in the metabolism of micronutrients in. SNP A sample of 496 sheep belonging to 20 breeds farmed in Italy were genotyped with the Illumina Ovine 50K beadchip. Data were analysed by canonical discriminant analysis (CDA). Forty SNP located in regions of the genome containing loci involved in the metabolism of vitamins and minerals were detected. in particular, genes linked to the metabolism of vitamins and minerals such as Selenocysteine Lyase (SCLY), calcium sensing receptor (CASR), Solute Carrier Family 23 Member 1 (SLC23A1) and Thiamine Triphosphatase (THTPA) were highlighted. Keywords: selection signatures, micronutrients, sheep, Canonical Discriminant Analysis Introduction Nutritional status is of particular importance for productive performances in livestock. Growth, milk production, reproduction depend on a wide range of essential nutrients such as amino acids, fatty acids, vitamins and minerals. -

The Genotype Analysis and Prenatal Genetic Diagnosis Among 244 Pedigrees with Methylmalonic Aciduria in China
The genotype analysis and prenatal genetic diagnosis among 244 pedigrees with methylmalonic aciduria in China Shuang Hu First Aliated Hospital of Zhengzhou University Lina Liu First Aliated Hospital of Zhengzhou University Zhihui Jiao First Aliated Hospital of Zhengzhou University Xiangdong Kong ( [email protected] ) First Aliated Hospital of Zhengzhou University Research Article Keywords: methylmalonic aciduria, MMACHC, MUT, variant, prenatal genetic diagnosis Posted Date: February 24th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-249909/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/20 Abstract To investigate the phenotypes, biochemical features and genotypes for 244 pedigrees with methylmalonic aciduria (MMA) in China, and to perform the prenatal genetic diagnosis by chorionic villus for these pedigrees. Gene analyses were performed for 244 pedigrees. There are 130 families, chorionic villus sampling was performed on the pregnant women to conduct the prenatal diagnosis. Among 244 patients, 168 (68.9%) cases were combined methylmalonic aciduria and homocystinuria, 76 (31.1%) cases were isolated methymalonic aciduria. All the patients were diagnosed with MMA by their clinical manifestation, elevated blood propionylcarnitine, propionylcarnitine to acetylcarnitine ratio, and/or urine/blood methylmalonic acid with or without hyperhomocysteinemia. MMACHC, MUT, SUCLG1 and LMBRD1 gene variants were found in 236 (96.7%) pedigrees included 6 probands with only one heterozygous variant out of 244 cases. For the 130 pedigrees who received a prenatal diagnosis, 22 foetuses were normal, 69 foetuses were carriers of heterozygous variants, and the remaining 39 foetuses harboured compound heterozygous variants or homozygous variants.