Blueprint Genetics Organic Acidemia/Aciduria &Amp
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hyperammonemia in Review: Pathophysiology, Diagnosis, and Treatment
Pediatr Nephrol DOI 10.1007/s00467-011-1838-5 EDUCATIONAL REVIEW Hyperammonemia in review: pathophysiology, diagnosis, and treatment Ari Auron & Patrick D. Brophy Received: 23 September 2010 /Revised: 9 January 2011 /Accepted: 12 January 2011 # IPNA 2011 Abstract Ammonia is an important source of nitrogen and is the breakdown and catabolism of dietary and bodily proteins, required for amino acid synthesis. It is also necessary for respectively. In healthy individuals, amino acids that are not normal acid-base balance. When present in high concentra- needed for protein synthesis are metabolized in various tions, ammonia is toxic. Endogenous ammonia intoxication chemical pathways, with the rest of the nitrogen waste being can occur when there is impaired capacity of the body to converted to urea. Ammonia is important for normal animal excrete nitrogenous waste, as seen with congenital enzymatic acid-base balance. During exercise, ammonia is produced in deficiencies. A variety of environmental causes and medica- skeletal muscle from deamination of adenosine monophos- tions may also lead to ammonia toxicity. Hyperammonemia phate and amino acid catabolism. In the brain, the latter refers to a clinical condition associated with elevated processes plus the activity of glutamate dehydrogenase ammonia levels manifested by a variety of symptoms and mediate ammonia production. After formation of ammonium signs, including significant central nervous system (CNS) from glutamine, α-ketoglutarate, a byproduct, may be abnormalities. Appropriate and timely management requires a degraded to produce two molecules of bicarbonate, which solid understanding of the fundamental pathophysiology, are then available to buffer acids produced by dietary sources. differential diagnosis, and treatment approaches available. -

Clinical Spectrum of Glycine Encephalopathy in Indian Children
Clinical Spectrum of Glycine Encephalopathy in Indian children Anil B. Jalan *, Nandan Yardi ** NIRMAN, 203, Nirman Vyapar Kendra, Sector 17, Vashi – Navi-Mumbai, India – 400 705 * Chief Scientific Research Officer (Bio – chemical Genetics) ** Paediatric Neurologist an Epileptologist, Pune. Introduction: NKH is generally considered to be a rare disease, but relatively higher incidences have been reported in Northern Finland, British Columbia and Israel (1,2). Non Ketotic Hyperglycinemia, also known as Glycine Encephalopathy, is an Autosomal recessive disorder of Glycine metabolism caused by a defect in the Glycine cleavage enzyme complex (GCS). GCS is a complex of four proteins and coded on 4 different chromosomes. 1. P – Protein ( Pyridoxal Phosphate containing glycine Decarboxylase, GLDC) -> 80 % cases, [ MIM no. 238300 ] , 2. H – Protein (Lipoic acid containing) – Rare, [MIM no. 238310], 3. T – Protein ( Tetrahydrofolate requiring aminomethyltranferase AMT ) – 15 % cases [ MIM no. 238330], 4. L – Protein (Lipoamide dehydrogenase) – MSUD like picture [MIM no. 238331] (1). In classical NKH, levels of CSF – glycine and the ratio of CSF / Plasma glycine are very high (1). Classically, NKH presents in the early neonatal period with progressive lethargy, hypotonia, myoclonic jerks, hiccups, and apnea, usually leading to total unresponsiveness, coma, and death unless the patient is supported through this stage with mechanical ventilation. Survivors almost invariably display profound neurological disability and intractable seizures. In a minority of NKH cases the presentation is atypical with a later onset and features including seizures, developmental delay and / or regression, hyperactivity, spastic diplegia, spino – cerebeller degeneration, optic atrophy, vertical gaze palsy, ataxia, chorea, and pulmonary hypertension. Atypical cases are more likely to have milder elevations of glycine concentrations (2). -
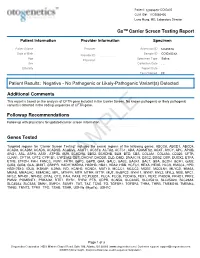
PDF Document Created by Pdffiller
Patient: 1234567843314948-COtGx0053 CLIA ID#: 11D2066426 Larry Hung, MD, Laboratory Director GxTM Carrier Screen Testing Report Patient Information Provider Information Specimen Patient Name Haley Papevies Provider Harbin Clinic Women's Accession ID 1234567843314948 Center Cartersville Date of Birth Apr 16, 1998 Sample ID COtGx0053XX Provider ID 1124488556 Age 19 Specimen Type Saliva Physician Vicki Yates Sex female Collection Date Jul 20, 2017 Ethnicity Report Date Aug 5, 2017 Test Ordered CF Patient Results: Negative - No Pathogenic or Likely-Pathogenic Variant(s) Detected Additional Comments This report is based on the analysis of CFTR gene included in the Carrier Screen. No known pathogenic or likely pathogenic variant(s) detected in the coding sequences of CFTR gene. Followup Recommendations Follow up with physicians for updated carrier screen information. The sequencing for CFTR gene was carried out with the other genes included in the Carrier Screen Testing (listed below). The analysis of the other genes in the Carrier Screen could be ordered through your physicians. Genes Tested Targeted regions for “Carrier Screen Testing” includes the exonic regions of the following genes: ABCC8, ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACSF3, ACTA2, ACTC1, ADA, ADAMTS2, AGXT, AHCY, APC, APOB, ARG1, ASL, ASPA, ASS1, ATP7B, AUH, BCKDHA, BBS2, BCKDHB, BLM, BTD, CBS, COL3A1, COL4A3, CD320, CFTR, CLRN1, CPT1A, CPT2, CYP1B1, CYP21A2, DBT, DHCR7, DHDDS, DLD, DMD, DNAJC19, DSC2, DSG2, DSP, DUOX2, ETFA, ETFB, ETFDH, FAH, FANCC, FBN1, -

Supplement 1 Overview of Dystonia Genes
Supplement 1 Overview of genes that may cause dystonia in children and adolescents Gene (OMIM) Disease name/phenotype Mode of inheritance 1: (Formerly called) Primary dystonias (DYTs): TOR1A (605204) DYT1: Early-onset generalized AD primary torsion dystonia (PTD) TUBB4A (602662) DYT4: Whispering dystonia AD GCH1 (600225) DYT5: GTP-cyclohydrolase 1 AD deficiency THAP1 (609520) DYT6: Adolescent onset torsion AD dystonia, mixed type PNKD/MR1 (609023) DYT8: Paroxysmal non- AD kinesigenic dyskinesia SLC2A1 (138140) DYT9/18: Paroxysmal choreoathetosis with episodic AD ataxia and spasticity/GLUT1 deficiency syndrome-1 PRRT2 (614386) DYT10: Paroxysmal kinesigenic AD dyskinesia SGCE (604149) DYT11: Myoclonus-dystonia AD ATP1A3 (182350) DYT12: Rapid-onset dystonia AD parkinsonism PRKRA (603424) DYT16: Young-onset dystonia AR parkinsonism ANO3 (610110) DYT24: Primary focal dystonia AD GNAL (139312) DYT25: Primary torsion dystonia AD 2: Inborn errors of metabolism: GCDH (608801) Glutaric aciduria type 1 AR PCCA (232000) Propionic aciduria AR PCCB (232050) Propionic aciduria AR MUT (609058) Methylmalonic aciduria AR MMAA (607481) Cobalamin A deficiency AR MMAB (607568) Cobalamin B deficiency AR MMACHC (609831) Cobalamin C deficiency AR C2orf25 (611935) Cobalamin D deficiency AR MTRR (602568) Cobalamin E deficiency AR LMBRD1 (612625) Cobalamin F deficiency AR MTR (156570) Cobalamin G deficiency AR CBS (613381) Homocysteinuria AR PCBD (126090) Hyperphelaninemia variant D AR TH (191290) Tyrosine hydroxylase deficiency AR SPR (182125) Sepiaterine reductase -

CBS, MET Act Sheet
Newborn Screening ACT Sheet Increased Methionine Homocystinuria (CBS Deficiency) / Hypermethioninemia (MET) Differential Diagnosis: Classical homocystinuria (cystathionine β-synthase (CBS) deficiency); hypermethioninemia (MET) due to methionine adenosyltransferase I/III MAT I/III deficiency; glycine n-methyltransferase GNMT deficiency; adenosylhomocysteine hydrolase deficiency; liver disease; hyperalimentation. Condition Description: Methionine from ingested protein is normally converted to homocysteine. In classical homocystinuria due to CBS deficiency, homocysteine cannot be converted to cystathionine. As a result, the concentration of homocysteine and its precursor, methionine, will become elevated. In MAT I/III deficiency and the other hypermethioninemias, methionine is increased in the absence of, or only with, a slightly increased level of homocysteine. You Should Take the Following IMMEDIATE Actions • Contact family to inform them of the newborn screening result and ascertain clinical status. • Consult with pediatric metabolic specialist. (See attached list.) • Evaluate the newborn with attention to liver disease and refer as appropriate. • Initiate confirmatory/diagnostic tests in consultation with metabolic specialist. • Initial testing: Plasma quantitative amino acids and plasma total homocysteine. • Repeat newborn screen if second screen has not been done. • Educate family about homocystinuria and its management as appropriate. • Report findings to newborn screening program. Diagnostic Evaluation: Plasma quantitative amino -

Incidence of Inborn Errors of Metabolism by Expanded Newborn
Original Article Journal of Inborn Errors of Metabolism & Screening 2016, Volume 4: 1–8 Incidence of Inborn Errors of Metabolism ª The Author(s) 2016 DOI: 10.1177/2326409816669027 by Expanded Newborn Screening iem.sagepub.com in a Mexican Hospital Consuelo Cantu´-Reyna, MD1,2, Luis Manuel Zepeda, MD1,2, Rene´ Montemayor, MD3, Santiago Benavides, MD3, Hector´ Javier Gonza´lez, MD3, Mercedes Va´zquez-Cantu´,BS1,4, and Hector´ Cruz-Camino, BS1,5 Abstract Newborn screening for the detection of inborn errors of metabolism (IEM), endocrinopathies, hemoglobinopathies, and other disorders is a public health initiative aimed at identifying specific diseases in a timely manner. Mexico initiated newborn screening in 1973, but the national incidence of this group of diseases is unknown or uncertain due to the lack of large sample sizes of expanded newborn screening (ENS) programs and lack of related publications. The incidence of a specific group of IEM, endocrinopathies, hemoglobinopathies, and other disorders in newborns was obtained from a Mexican hospital. These newborns were part of a comprehensive ENS program at Ginequito (a private hospital in Mexico), from January 2012 to August 2014. The retrospective study included the examination of 10 000 newborns’ results obtained from the ENS program (comprising the possible detection of more than 50 screened disorders). The findings were the following: 34 newborns were confirmed with an IEM, endocrinopathies, hemoglobinopathies, or other disorders and 68 were identified as carriers. Consequently, the estimated global incidence for those disorders was 3.4 in 1000 newborns; and the carrier prevalence was 6.8 in 1000. Moreover, a 0.04% false-positive rate was unveiled as soon as diagnostic testing revealed negative results. -

EXTENDED CARRIER SCREENING Peace of Mind for Planned Pregnancies
Focusing on Personalised Medicine EXTENDED CARRIER SCREENING Peace of Mind for Planned Pregnancies Extended carrier screening is an important tool for prospective parents to help them determine their risk of having a child affected with a heritable disease. In many cases, parents aren’t aware they are carriers and have no family history due to the rarity of some diseases in the general population. What is covered by the screening? Genomics For Life offers a comprehensive Extended Carrier Screening test, providing prospective parents with the information they require when planning their pregnancy. Extended Carrier Screening has been shown to detect carriers who would not have been considered candidates for traditional risk- based screening. With a simple mouth swab collection, we are able to test for over 419 genes associated with inherited diseases, including Fragile X Syndrome, Cystic Fibrosis and Spinal Muscular Atrophy. The assay has been developed in conjunction with clinical molecular geneticists, and includes genes listed in the NIH Genetic Test Registry. For a list of genes and disorders covered, please see the reverse of this brochure. If your gene of interest is not covered on our Extended Carrier Screening panel, please contact our friendly team to assist you in finding a gene test panel that suits your needs. Why have Extended Carrier Screening? Extended Carrier Screening prior to pregnancy enables couples to learn about their reproductive risk and consider a complete range of reproductive options, including whether or not to become pregnant, whether to use advanced reproductive technologies, such as preimplantation genetic diagnosis, or to use donor gametes. -

Birth Prevalence of Disorders Detectable Through Newborn Screening by Race/Ethnicity
©American College of Medical Genetics and Genomics ORIGINAL RESEARCH ARTICLE Birth prevalence of disorders detectable through newborn screening by race/ethnicity Lisa Feuchtbaum, DrPH, MPH1, Jennifer Carter, MPH2, Sunaina Dowray, MPH2, Robert J. Currier, PhD1 and Fred Lorey, PhD1 Purpose: The purpose of this study was to describe the birth prev- Conclusion: The California newborn screening data offer a alence of genetic disorders among different racial/ethnic groups unique opportunity to explore the birth prevalence of many through population-based newborn screening data. genetic dis orders across a wide spectrum of racial/ethnicity classifications. The data demonstrate that racial/ethnic subgroups Methods: Between 7 July 2005 and 6 July 2010 newborns in Cali- of the California newborn population have very different patterns fornia were screened for selected metabolic, endocrine, hemoglobin, of heritable disease expression. Determining the birth prevalence and cystic fibrosis disorders using a blood sample collected via heel of these disorders in California is a first step to understanding stick. The race and ethnicity of each newborn was self-reported by the short- and long-term medical and treatment needs faced by the mother at the time of specimen collection. affected communities, especially those groups that are impacted by Results: Of 2,282,138 newborns screened, the overall disorder detec- more severe disorders. tion rate was 1 in 500 births. The disorder with the highest prevalence Genet Med 2012:14(11):937–945 among all groups was primary congenital hypothyroidism (1 in 1,706 births). Birth prevalence for specific disorders varied widely among Key Words: birth prevalence; disorders; newborn screening; race different racial/ethnic groups. -

16. Questions and Answers
16. Questions and Answers 1. Which of the following is not associated with esophageal webs? A. Plummer-Vinson syndrome B. Epidermolysis bullosa C. Lupus D. Psoriasis E. Stevens-Johnson syndrome 2. An 11 year old boy complains that occasionally a bite of hotdog “gives mild pressing pain in his chest” and that “it takes a while before he can take another bite.” If it happens again, he discards the hotdog but sometimes he can finish it. The most helpful diagnostic information would come from A. Family history of Schatzki rings B. Eosinophil counts C. UGI D. Time-phased MRI E. Technetium 99 salivagram 3. 12 year old boy previously healthy with one-month history of difficulty swallowing both solid and liquids. He sometimes complains food is getting stuck in his retrosternal area after swallowing. His weight decreased approximately 5% from last year. He denies vomiting, choking, gagging, drooling, pain during swallowing or retrosternal pain. His physical examination is normal. What would be the appropriate next investigation to perform in this patient? A. Upper Endoscopy B. Upper GI contrast study C. Esophageal manometry D. Modified Barium Swallow (MBS) E. Direct laryngoscopy 4. A 12 year old male presents to the ER after a recent episode of emesis. The parents are concerned because undigested food 3 days old was in his vomit. He admits to a sensation of food and liquids “sticking” in his chest for the past 4 months, as he points to the upper middle chest. Parents relate a 10 lb (4.5 Kg) weight loss over the past 3 months. -

Neurodevelopmental Signatures of Narcotic and Neuropsychiatric Risk Factors in 3D Human-Derived Forebrain Organoids
Molecular Psychiatry www.nature.com/mp ARTICLE OPEN Neurodevelopmental signatures of narcotic and neuropsychiatric risk factors in 3D human-derived forebrain organoids 1 1 1 1 2 2 3 Michael Notaras , Aiman Lodhi , Estibaliz✉ Barrio-Alonso , Careen Foord , Tori Rodrick , Drew Jones , Haoyun Fang , David Greening 3,4 and Dilek Colak 1,5 © The Author(s) 2021 It is widely accepted that narcotic use during pregnancy and specific environmental factors (e.g., maternal immune activation and chronic stress) may increase risk of neuropsychiatric illness in offspring. However, little progress has been made in defining human- specific in utero neurodevelopmental pathology due to ethical and technical challenges associated with accessing human prenatal brain tissue. Here we utilized human induced pluripotent stem cells (hiPSCs) to generate reproducible organoids that recapitulate dorsal forebrain development including early corticogenesis. We systemically exposed organoid samples to chemically defined “enviromimetic” compounds to examine the developmental effects of various narcotic and neuropsychiatric-related risk factors within tissue of human origin. In tandem experiments conducted in parallel, we modeled exposure to opiates (μ-opioid agonist endomorphin), cannabinoids (WIN 55,212-2), alcohol (ethanol), smoking (nicotine), chronic stress (human cortisol), and maternal immune activation (human Interleukin-17a; IL17a). Human-derived dorsal forebrain organoids were consequently analyzed via an array of unbiased and high-throughput analytical approaches, including state-of-the-art TMT-16plex liquid chromatography/mass- spectrometry (LC/MS) proteomics, hybrid MS metabolomics, and flow cytometry panels to determine cell-cycle dynamics and rates of cell death. This pipeline subsequently revealed both common and unique proteome, reactome, and metabolome alterations as a consequence of enviromimetic modeling of narcotic use and neuropsychiatric-related risk factors in tissue of human origin. -

Abstracts from the 9Th Biennial Scientific Meeting of The
International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):15 DOI 10.1186/s13633-017-0054-x MEETING ABSTRACTS Open Access Abstracts from the 9th Biennial Scientific Meeting of the Asia Pacific Paediatric Endocrine Society (APPES) and the 50th Annual Meeting of the Japanese Society for Pediatric Endocrinology (JSPE) Tokyo, Japan. 17-20 November 2016 Published: 28 Dec 2017 PS1 Heritable forms of primary bone fragility in children typically lead to Fat fate and disease - from science to global policy a clinical diagnosis of either osteogenesis imperfecta (OI) or juvenile Peter Gluckman osteoporosis (JO). OI is usually caused by dominant mutations affect- Office of Chief Science Advsor to the Prime Minister ing one of the two genes that code for two collagen type I, but a re- International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):PS1 cessive form of OI is present in 5-10% of individuals with a clinical diagnosis of OI. Most of the involved genes code for proteins that Attempts to deal with the obesity epidemic based solely on adult be- play a role in the processing of collagen type I protein (BMP1, havioural change have been rather disappointing. Indeed the evidence CREB3L1, CRTAP, LEPRE1, P4HB, PPIB, FKBP10, PLOD2, SERPINF1, that biological, developmental and contextual factors are operating SERPINH1, SEC24D, SPARC, from the earliest stages in development and indeed across generations TMEM38B), or interfere with osteoblast function (SP7, WNT1). Specific is compelling. The marked individual differences in the sensitivity to the phenotypes are caused by mutations in SERPINF1 (recessive OI type obesogenic environment need to be understood at both the individual VI), P4HB (Cole-Carpenter syndrome) and SEC24D (‘Cole-Carpenter and population level. -

Involvements of Hyperhomocysteinemia in Neurological Disorders
H OH metabolites OH Review Involvements of Hyperhomocysteinemia in Neurological Disorders Marika Cordaro 1,† , Rosalba Siracusa 2,† , Roberta Fusco 2 , Salvatore Cuzzocrea 2,3,* , Rosanna Di Paola 2,* and Daniela Impellizzeri 2 1 Department of Biomedical, Dental and Morphological and Functional Imaging, University of Messina, Via Consolare Valeria, 98125 Messina, Italy; [email protected] 2 Department of Chemical, Biological, Pharmaceutical and Environmental Sciences, University of Messina, 98166 Messina, Italy; [email protected] (R.S.); [email protected] (R.F.); [email protected] (D.I.) 3 Department of Pharmacological and Physiological Science, Saint Louis University School of Medicine, Saint Louis, MO 63104, USA * Correspondence: [email protected] (S.C.); [email protected] (R.D.P.); Tel.: +39-090-6765208 (S.C. & R.D.P.) † The authors equally contributed to the review. Abstract: Homocysteine (HCY), a physiological amino acid formed when proteins break down, leads to a pathological condition called hyperhomocysteinemia (HHCY), when it is over a definite limit. It is well known that an increase in HCY levels in blood, can contribute to arterial damage and several cardiovascular disease, but the knowledge about the relationship between HCY and brain disorders is very poor. Recent studies demonstrated that an alteration in HCY metabolism or a deficiency in folate or vitamin B12 can cause altered methylation and/or redox potentials, that leads to a modification on calcium influx in cells, or into an accumulation in amyloid and/or tau protein involving a cascade of events that culminate in apoptosis, and, in the worst conditions, neuronal death. The present review will thus summarize how much is known about the possible role of HHCY in neurodegenerative disease.