Isolated Palmar Dislocation of the Fifth Carpometacarpal Joint: a Case Report of Rare Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

New Fixation Approach for Transverse Metacarpal Neck Fracture: a Biomechanical Study
Chiu et al. Journal of Orthopaedic Surgery and Research (2018) 13:183 https://doi.org/10.1186/s13018-018-0890-2 RESEARCHARTICLE Open Access New fixation approach for transverse metacarpal neck fracture: a biomechanical study Yung-Cheng Chiu1,2, Ming-Tzu Tsai3, Cheng-En Hsu4,5, Horng-Chaung Hsu1,2, Heng-Li Huang6,7 and Jui-Ting Hsu6,7* Abstract Background: Fifth metacarpal neck fracture, also known as boxer’s fracture, is the most common metacarpal fracture. Percutaneous Kirschner-wire (K-wire) pinning has been shown to produce favorable clinical results. However, the fixation power of K-wires is a major concern. Plate fixation is also a surgical option, but it has the disadvantages of tendon adhesion, requirement of secondary surgery for removal of the implant, and postoperative joint stiffness. A fixation method that causes little soft tissue damage and provides high biomechanical stability is required for patients with fifth metacarpal neck fracture for whom surgical intervention is indicated. The present study proposed fixation using K-wires and a cerclage wire to treat fifth metacarpal neck fracture. The fixation power of this new method was compared with that of K-wires alone and plates. Methods: We used a saw blade to create transverse metacarpal neck fractures in 16 artificial metacarpal bone specimens, which were then treated with four types of fixation as follows: (1) locking plate with five locking bicortical screws (LP group), (2) regular plate with five bicortical screws (RP group), (3) two K-wires (K group), and (4) two K-wires and a figure-of-eight cerclage wire (KW group). -

Orthopaedics Instructions: to Best Navigate the List, First Download This PDF File to Your Computer
Orthopaedics Instructions: To best navigate the list, first download this PDF file to your computer. Then navigate the document using the bookmarks feature in the left column. The bookmarks expand and collapse. Finally, ensure that you look at the top of each category and work down to review notes or specific instructions. Bookmarks: Bookmarks: notes or specific with expandable instructions and collapsible topics As you start using the codes, it is recommended that you also check in Index and Tabular lists to ensure there is not a code with more specificity or a different code that may be more appropriate for your patient. Copyright APTA 2016, ALL RIGHTS RESERVED. Last Updated: 09/14/16 Contact: [email protected] Orthopaedics Disorder by site: Ankle Achilles tendinopathy ** Achilles tendinopathy is not listed in ICD10 M76.6 Achilles tendinitis Achilles bursitis M76.61 Achilles tendinitis, right leg M76.62 Achilles tendinitis, left leg ** Tendinosis is not listed in ICD10 M76.89 Other specified enthesopathies of lower limb, excluding foot M76.891 Other specified enthesopathies of right lower limb, excluding foot M76.892 Other specified enthesopathies of left lower limb, excluding foot Posterior tibialis dysfunction **Posterior Tibial Tendon Dysfunction (PTTD) is not listed in ICD10 M76.82 Posterior tibial tendinitis M76.821 Posterior tibial tendinitis, right leg M76.822 Posterior tibial tendinitis, left leg M76.89 Other specified enthesopathies of lower limb, excluding foot M76.891 Other specified enthesopathies of right lower limb, -

Four Unusual Cases of Congenital Forelimb Malformations in Dogs
animals Article Four Unusual Cases of Congenital Forelimb Malformations in Dogs Simona Di Pietro 1 , Giuseppe Santi Rapisarda 2, Luca Cicero 3,* , Vito Angileri 4, Simona Morabito 5, Giovanni Cassata 3 and Francesco Macrì 1 1 Department of Veterinary Sciences, University of Messina, Viale Palatucci, 98168 Messina, Italy; [email protected] (S.D.P.); [email protected] (F.M.) 2 Department of Veterinary Prevention, Provincial Health Authority of Catania, 95030 Gravina di Catania, Italy; [email protected] 3 Institute Zooprofilattico Sperimentale of Sicily, Via G. Marinuzzi, 3, 90129 Palermo, Italy; [email protected] 4 Veterinary Practitioner, 91025 Marsala, Italy; [email protected] 5 Ospedale Veterinario I Portoni Rossi, Via Roma, 57/a, 40069 Zola Predosa (BO), Italy; [email protected] * Correspondence: [email protected] Simple Summary: Congenital limb defects are sporadically encountered in dogs during normal clinical practice. Literature concerning their diagnosis and management in canine species is poor. Sometimes, the diagnosis and description of congenital limb abnormalities are complicated by the concurrent presence of different malformations in the same limb and the lack of widely accepted classification schemes. In order to improve the knowledge about congenital limb anomalies in dogs, this report describes the clinical and radiographic findings in four dogs affected by unusual congenital forelimb defects, underlying also the importance of reviewing current terminology. Citation: Di Pietro, S.; Rapisarda, G.S.; Cicero, L.; Angileri, V.; Morabito, Abstract: Four dogs were presented with thoracic limb deformity. After clinical and radiographic S.; Cassata, G.; Macrì, F. Four Unusual examinations, a diagnosis of congenital malformations was performed for each of them. -

Fractures of Hamate: a Clinical Overview
MUSCULOSKELETAL SURGERY (2019) 103:15–21 https://doi.org/10.1007/s12306-018-0543-y REVIEW Fractures of hamate: a clinical overview G. Mouzopoulos1 · C. Vlachos1 · L. Karantzalis1 · K. Vlachos1 Received: 28 June 2017 / Accepted: 20 May 2018 / Published online: 29 May 2018 © Istituto Ortopedico Rizzoli 2018 Abstract Hamate fractures are exceedingly rare clinical entities. However, the diagnosis and treatment of these injuries are often delayed and can severely handicap the performance of afected laborers or athletes. This review focuses on fractures of the hamate and provides an update on the current consensus as to mechanism, diagnosis, management, and complications after such injuries. Keywords Hamate · Hook · Fracture Epidemiology the hook of the hamate [2]. If the grip is relaxed or control is lost, the fracture occurs at the end of a poor swing, as Fractures of the hamate usually occur through the hook centrifugal force is transmitted through the handle of the or body of the bone [1]. Type I fractures involve the hook racquet against the hook [7]. In golfers or baseball players, of the hamate and further are subdivided into three sub- a dubbed shot or a checked swing will fracture the hamulus types involving: base, waist, and avulsion (tip). Fractures because the butt of the club or bat will strike the hook. It has located at the base and proximal third (76%) of the hook also been described in polo and ice hockey [8]. are presented more frequently than fractures located at the Fall on an outstretched hand causing sudden forcible mid-third (13%) or the distal third (11%). -

Fractures of the Neck of the Fifth Metacarpal Bone. Medium-Term Results in 28 Cases Treated by Percutaneous Transverse Pinning I
Injury, Int. J. Care Injured 43 (2012) 242–245 Contents lists available at SciVerse ScienceDirect Injury jo urnal homepage: www.elsevier.com/locate/injury Fractures of the neck of the fifth metacarpal bone. Medium-term results in 28 cases treated by percutaneous transverse pinning V. Potenza *, R. Caterini, F. De Maio, S. Bisicchia, P. Farsetti Department of Orthopaedic Surgery, University of Rome ‘Tor Vergata’, Rome, Italy A R T I C L E I N F O A B S T R A C T Article history: The purpose of this study was to report the medium-term results in 28 patients affected by closed Accepted 27 October 2011 displaced fractures of the neck of the fifth metacarpal bone (boxer’s fracture) with an associated severe swelling of the hand, who were treated with percutaneous transverse K-wire pinning, to verify the Keywords: effectiveness of this surgical treatment. We opted for this treatment in all cases in which malrotation of Boxer’s fracture the fifth finger and volar angulation of the metacarpal head greater than 308 were associated with a Transverse pinning severe swelling of the hand. All the patients were reviewed clinically and radiologically at an average of Metacarpal neck fracture 25 months after surgery. At the final follow-up, no patient reported residual pain. All patients had full extension of the fifth finger, except two in whom we observed a limitation of the extension of the fifth metacarpophalangeal (MP) joint of about 108, without significant impairment of hand function. All patients had at least 908 flexion of the fifth MP joint and full range of motion of the interphalangeal (IP) joints. -

Functional Anatomy of the Equine Musculoskeletal System
1 CHAPTER Functional Anatomy of the Equine Musculoskeletal System ANNA DEE FAILS ANATOMIC NOMENCLATURE AND USAGE Foot Veterinary medical anatomists have been using the The foot consists of the hoof and all it encloses: the Nomina Anatomica Veterinaria, created by the Inter connective tissue corium (dermis), digital cushion, distal national Committee on Veterinary Gross Anatomical phalanx (coffin bone), most of the cartilages of the distal Nomenclature since 1968 to standardize the names of phalanx, distal interphalangeal (coffin) joint, distal part anatomical structures.46 This chapter endeavors to use the of the middle phalanx (short pastern bone), distal sesa most current, correct terms as outlined in that publication. moid (navicular) bone, podotrochlear bursa (navicular Nonetheless, equine practitioners need to be equally fluent bursa), several ligaments, tendons of insertion of the in older terminology, which is likely to be in wide usage common digital extensor and deep digital flexor mus among horse owners and equine professionals. This chap cles, blood vessels, and nerves. Skin between the heels is ter will provide useful and common synonyms for many also part of the foot. structures, along with their more technically correct terms. Figure 1.1 provides the directional terms for veteri HOOF WALL, SOLE, AND FROG nary anatomy that will be used in this chapter. With the exception of the ocular and oral cavity structures, the The hoof is continuous with the epidermis at the cor terms anterior, posterior, superior, and inferior are not onet, and the underlying corium of the hoof is likewise applicable to quadrupeds. continuous with the dermis of the skin. -

Fifth Metacarpal Bone Boxer's Fracture Phalanx Scissoring Brace May Be Used During Treatment
320 Warner Drive Lewiston, ID 83501 Boxer's Fracture Overview A boxer's fracture is a break of the metacarpal of the little finger. The metacarpals are the long bones in the hand that connect the fingers to the wrist. A boxer's fracture refers to a break at the end of the bone nearest the knuckle, which is called the metacarpal neck. Causes This type of fracture most commonly occurs when someone punches a hard surface (or another person) with a closed fist. Since most people punch in a roundhouse fashion, the first point of boney contact in a punch is the little finger metacarpal bone. The force concentrates at the metacarpal neck, leading to a fracture. Ironically, this is a rare injury in boxers because they are trained to punch with even force over the entire hand, maximizing force and minimizing injury. A boxer's fracture can also occur when a person stumbles and tries to Fifth metacarpal bone break his fall with a closed fist to the ground. Occasionally, direct trauma to the hand can also cause this injury. Boxer’s fracture Symptoms Common symptoms include pain, tenderness, and swelling around the knuckle of the little finger. Bruising and loss of knuckle contour are also common, and extending the finger may be difficult. In severely displaced fractures, the fingers may overlap (or scissor) when they are flexed. Phalanx Treatment Most boxer's fractures can be treated with a cast or brace to stabilize the fracture while it heals. If the knuckle is severely deformed, a procedure called a Scissoring closed reduction may be needed to push the fracture back into proper position before casting. -

Fracture of the Hamate with Interposition of the Base of 5Th
Journal of Case Reports and Studies Volume 5 | Issue 1 ISSN: 2348-9820 Case Report Open Access Fracture of the Hamate with Interposition of the Base of 5th Metacarpal, a Frequently Missed Injury Dabboussi NA, Fakih RR, Al husari H and Abtar HK* Department of Surgery, Makassed General Hospital, Beirut, Lebanon *Corresponding author: Abtar HK, Makassed General Hospital, P.O. Box: 11-6301 Riad EI-Solh, 11072210, Beirut, Lebanon, Tel: +961 70 858658, +961 1858658, E-mail: [email protected] Citation: Dabboussi NA, Fakih RR, Al husari H, Abtar HK (2017) Fracture of the Hamate with Interposition of the Base of 5th Metacarpal, a Frequently Missed Injury. J Case Rep Stud 5(1): 104. doi: 10.15744/2348- 9820.5.104 Received Date: December 26, 2016 Accepted Date: February 25, 2017 Published Date: February 28, 2017 Abstract We report a case of hamate fracture in the coronal plane with interposition of the base of 5th metacarpal bone. This injury is frequently missed and may results in increasing rate of morbidity and mal-union. In this article, the approach to this type of injuries, the diagnostic modalities, and the management will be discussed with review of the literature. Keywords: Hamate Bone; Fracture-Dislocation; Missed Injury List of Abbreviations: Three Dimensional Computed Tomography: 3D CT Scan Introduction Hamate fracture represents a small percentage of all carpal bone fractures [1], it is rare to the point that the incidence of its subtypes was not established. Hamate fractures with dislocation of fifth metacarpal are frequently missed by conventional x-rays, they need special views to be diagnosed, and the fracture architecture is best seen on three dimensional computed tomography (3D CT scan) [2]. -

Developing Learning Models to Teach Equine Anatomy and Biomechanics
The University of Maine DigitalCommons@UMaine Honors College Spring 5-2017 Developing Learning Models to Teach Equine Anatomy and Biomechanics Zandalee E. Toothaker University of Maine Follow this and additional works at: https://digitalcommons.library.umaine.edu/honors Part of the Animal Sciences Commons, and the Veterinary Anatomy Commons Recommended Citation Toothaker, Zandalee E., "Developing Learning Models to Teach Equine Anatomy and Biomechanics" (2017). Honors College. 453. https://digitalcommons.library.umaine.edu/honors/453 This Honors Thesis is brought to you for free and open access by DigitalCommons@UMaine. It has been accepted for inclusion in Honors College by an authorized administrator of DigitalCommons@UMaine. For more information, please contact [email protected]. DEVELOPING LEARNING MODELS TO TEACH EQUINE ANATOMY AND BIOMECHANICS By Zandalee E. Toothaker A Thesis Submitted in Partial Fulfillment of the Requirements for a Degree with Honors (Animal and Veterinary Science) The Honors College University of Maine May 2017 Advisory Committee: Dr. Robert C. Causey, Associate Professor of Animal and Veterinary Sciences, Advisor Dr. David Gross, Adjunct Associate Professor in Honors (English) Dr. Sarah Harlan-Haughey, Assistant Professor of English and Honors Dr. Rita L. Seger, Researcher of Animal and Veterinary Sciences Dr. James Weber, Associate Professor and Animal and Veterinary Sciences © 2017 Zandalee Toothaker All Rights Reserved ABSTRACT Animal owners and professionals benefit from an understanding of an animal’s anatomy and biomechanics. This is especially true of the horse. A better understanding of the horse’s anatomy and weight bearing capabilities will allow people to treat and prevent injuries in equine athletes and work horses. -
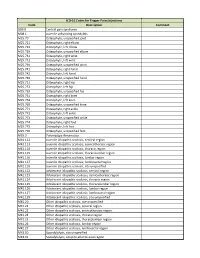
ICD-10 Codes for Trigger Point Injections
ICD-10 Codes for Trigger Point Injections Code Description Comment G89.0 Central pain syndrome M08.1 Juvenile ankylosing spondylitis M25.70 Osteophyte, unspecified joint M25.721 Osteophyte, right elbow M25.722 Osteophyte, left elbow M25.729 Osteophyte, unspecified elbow M25.731 Osteophyte, right wrist M25.732 Osteophyte, left wrist M25.739 Osteophyte, unspecified wrist M25.741 Osteophyte, right hand M25.742 Osteophyte, left hand M25.749 Osteophyte, unspecified hand M25.751 Osteophyte, right hip M25.752 Osteophyte, left hip M25.759 Osteophyte, unspecified hip M25.761 Osteophyte, right knee M25.762 Osteophyte, left knee M25.769 Osteophyte, unspecified knee M25.771 Osteophyte, right ankle M25.772 Osteophyte, left ankle M25.773 Osteophyte, unspecified ankle M25.774 Osteophyte, right foot M25.775 Osteophyte, left foot M25.776 Osteophyte, unspecified foot M35.3 Polymyalgia rheumatica M41.112 Juvenile idiopathic scoliosis, cervical region M41.113 Juvenile idiopathic scoliosis, cervicothoracic region M41.114 Juvenile idiopathic scoliosis, thoracic region M41.115 Juvenile idiopathic scoliosis, thoracolumbar region M41.116 Juvenile idiopathic scoliosis, lumbar region M41.117 Juvenile idiopathic scoliosis, lumbosacral region M41.119 Juvenile idiopathic scoliosis, site unspecified M41.122 Adolescent idiopathic scoliosis, cervical region M41.123 Adolescent idiopathic scoliosis, cervicothoracic region M41.124 Adolescent idiopathic scoliosis, thoracic region M41.125 Adolescent idiopathic scoliosis, thoracolumbar region M41.126 Adolescent idiopathic -

Metacarpal Bone Density in Carpal Tunnel Syndrome Patients Without
Original Article / Orijinal Araflt›rma 15 Metacarpal Bone Density in Carpal Tunnel Syndrome Patients Without Thenar Atrophy Tenar Atrofisi Olmayan Karpal Tünel Sendromlu Hastalarda Metakarpal Kemik Yo¤unlu¤unun De¤erlendirilmesi Serpil Savafl, Berna Okudan1, Hasan Rifat Koyuncuo¤lu2, Hakan Çelik, Tamer Karaaslan3, Mustafa Y›ld›z 4 Süleyman Demirel Üniversitesi T›p Fakültesi Fiziksel T›p ve Rehabilitasyon, 2Nöroloji, 3Beyin Cerrahisi ve 4Nükleer T›p Anabilim Dal›, Isparta, Türkiye, 1Yeditepe Üniversitesi T›p Fakültesi Nükleer T›p Anabilim Dal›, ‹stanbul, Türkiye Abstract Özet Objective: Bone loss due to thenar atrophy was reported in the me- Amaç: Premenopozal karpal tünel sendromlu (KTS) kad›nlarda te- tacarpal bones in premenopausal patients with carpal tunnel nar atrofiye ba¤l› olarak metakarpal kemik yo¤unlu¤u kayb› oldu- syndrome (CTS). The present study was designed to assess bone ¤u bilinmektedir. Bu çal›flman›n amac›, tenar atrofisi olmayan KTS’li density in the metacarpal bones in patients with CTS without hastalarda metakarpal kemik mineral yo¤unlu¤unu de¤erlendir- thenar atrophy and to correlate the metacarpal bone density with mek, metakarpal kemik yo¤unlu¤u ile elektrofizyolojik bulgular›, el the electrophysiological findings, hand strength and Boston gücü ve Boston Anketi aras›ndaki iliflkiyi belirlemektir. Questionnaire (BQ). Hastalar ve Yöntem: Çal›flmaya tenar atrofisi olmayan 30 KTS’li pre- Patients and Methods: Thirty premenopausal patients with CTS menopozal hasta ile 32 premenopozal kontrol olgu al›nd›. KTS’li without thenar atrophy were enrolled in this study. Thirty-two hastalar›n semptom fliddeti ve fonksiyonel durumlar› Bostan Anke- consecutive premenopausal women were included in the study as ti ile de¤erlendirildi. -
Case Reports Series A, B, C & D Table of Contents
ACTEC X H E • • C S A T S E R REPO Case Reports Series A, B, C & D Table of ConTents Revision Total Joint Series A, Number 1 ..................................................................................................................................................... 3 Use of opteform® to Repair failed Total Knee Prosthesis with osteolysis, Harry Schmaltz, MD Series A, Number 2 ..................................................................................................................................................... 5 Use of opteform® to Repair Acetabular osteolysis Series A, Number 4 ..................................................................................................................................................... 7 large osteolytic Defect Repair Using opteform® Through an Illiac Window, Abbott Kagan, MD Series A, Number 5 ..................................................................................................................................................... 9 Repair of Acetabular fracture and osteolysis with opteform®-Two Year follow-Up, Wayne Moody, MD fACS Series A, Number 6 ................................................................................................................................................... 11 Acetabular Reconstruction with opteform® and Reconstruction Ring, Wayne Moody, MD fACS Series A, Number 7 ................................................................................................................................................... 13 Use of opteform®