A Novel Compound Heterozygous Mutation in VARS2 in a Newborn
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
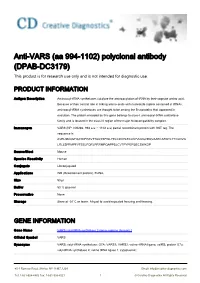
Anti-VARS (Aa 994-1102) Polyclonal Antibody (DPAB-DC3179) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-VARS (aa 994-1102) polyclonal antibody (DPAB-DC3179) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description Aminoacyl-tRNA synthetases catalyze the aminoacylation of tRNA by their cognate amino acid. Because of their central role in linking amino acids with nucleotide triplets contained in tRNAs, aminoacyl-tRNA synthetases are thought to be among the first proteins that appeared in evolution. The protein encoded by this gene belongs to class-I aminoacyl-tRNA synthetase family and is located in the class III region of the major histocompatibility complex. Immunogen VARS (NP_006286, 994 a.a. ~ 1102 a.a) partial recombinant protein with GST tag. The sequence is AVRLSNQGFQAYDFPAVTTAQYSFWLYELCDVYLECLKPVLNGVDQVAAECARQTLYTCLDVG LRLLSPFMPFVTEELFQRLPRRMPQAPPSLCVTPYPEPSECSWKDP Source/Host Mouse Species Reactivity Human Conjugate Unconjugated Applications WB (Recombinant protein), ELISA, Size 50 μl Buffer 50 % glycerol Preservative None Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. GENE INFORMATION Gene Name VARS valyl-tRNA synthetase [ Homo sapiens (human) ] Official Symbol VARS Synonyms VARS; valyl-tRNA synthetase; G7A; VARS1; VARS2; valine--tRNA ligase; valRS; protein G7a; valyl-tRNA synthetase 2; valine tRNA ligase 1, cytoplasmic; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Entrez Gene ID 7407 Protein Refseq NP_006286 UniProt ID A0A024RCN6 Chromosome Location 6p21.3 Pathway Aminoacyl-tRNA biosynthesis; Cytosolic tRNA aminoacylation; tRNA Aminoacylation; Function ATP binding; aminoacyl-tRNA editing activity; valine-tRNA ligase activity; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 2 © Creative Diagnostics All Rights Reserved. -

Downloaded Per Proteome Cohort Via the Web- Site Links of Table 1, Also Providing Information on the Deposited Spectral Datasets
www.nature.com/scientificreports OPEN Assessment of a complete and classifed platelet proteome from genome‑wide transcripts of human platelets and megakaryocytes covering platelet functions Jingnan Huang1,2*, Frauke Swieringa1,2,9, Fiorella A. Solari2,9, Isabella Provenzale1, Luigi Grassi3, Ilaria De Simone1, Constance C. F. M. J. Baaten1,4, Rachel Cavill5, Albert Sickmann2,6,7,9, Mattia Frontini3,8,9 & Johan W. M. Heemskerk1,9* Novel platelet and megakaryocyte transcriptome analysis allows prediction of the full or theoretical proteome of a representative human platelet. Here, we integrated the established platelet proteomes from six cohorts of healthy subjects, encompassing 5.2 k proteins, with two novel genome‑wide transcriptomes (57.8 k mRNAs). For 14.8 k protein‑coding transcripts, we assigned the proteins to 21 UniProt‑based classes, based on their preferential intracellular localization and presumed function. This classifed transcriptome‑proteome profle of platelets revealed: (i) Absence of 37.2 k genome‑ wide transcripts. (ii) High quantitative similarity of platelet and megakaryocyte transcriptomes (R = 0.75) for 14.8 k protein‑coding genes, but not for 3.8 k RNA genes or 1.9 k pseudogenes (R = 0.43–0.54), suggesting redistribution of mRNAs upon platelet shedding from megakaryocytes. (iii) Copy numbers of 3.5 k proteins that were restricted in size by the corresponding transcript levels (iv) Near complete coverage of identifed proteins in the relevant transcriptome (log2fpkm > 0.20) except for plasma‑derived secretory proteins, pointing to adhesion and uptake of such proteins. (v) Underrepresentation in the identifed proteome of nuclear‑related, membrane and signaling proteins, as well proteins with low‑level transcripts. -

Genome-Wide Association Study of Diabetic Kidney Disease Highlights Biology Involved in Glomerular Basement Membrane Collagen
CLINICAL RESEARCH www.jasn.org Genome-Wide Association Study of Diabetic Kidney Disease Highlights Biology Involved in Glomerular Basement Membrane Collagen Rany M. Salem ,1 Jennifer N. Todd,2,3,4 Niina Sandholm ,5,6,7 Joanne B. Cole ,2,3,4 Wei-Min Chen,8 Darrell Andrews,9 Marcus G. Pezzolesi,10 Paul M. McKeigue,11 Linda T. Hiraki,12 Chengxiang Qiu,13 Viji Nair,14 Chen Di Liao,12 Jing Jing Cao,12 Erkka Valo ,5,6,7 Suna Onengut-Gumuscu,8 Adam M. Smiles,15 Stuart J. McGurnaghan,16 Jani K. Haukka,5,6,7 Valma Harjutsalo,5,6,7,17 Eoin P. Brennan,9 Natalie van Zuydam,18,19 Emma Ahlqvist,20 Ross Doyle,9 Tarunveer S. Ahluwalia ,21 Maria Lajer,21 Maria F. Hughes,9 Jihwan Park,13 Jan Skupien,15 Athina Spiliopoulou,11 Andrew Liu,22 Rajasree Menon,14,23 Carine M. Boustany-Kari,24 Hyun M. Kang,23,25 Robert G. Nelson,26 Ronald Klein,27 Barbara E. Klein,27 Kristine E. Lee ,27 Xiaoyu Gao,28 Michael Mauer,29 Silvia Maestroni,30 Maria Luiza Caramori,29 Ian H. de Boer ,31 Rachel G. Miller,32 Jingchuan Guo ,32 Andrew P. Boright,12 David Tregouet,33,34 Beata Gyorgy,33,34 Janet K. Snell-Bergeon,35 David M. Maahs,36 Shelley B. Bull ,37 Angelo J. Canty,38 Colin N.A. Palmer,39 Lars Stechemesser,40 Bernhard Paulweber,40 Raimund Weitgasser,40,41 Jelizaveta Sokolovska,42 Vita Rovıte,43 Valdis Pırags, 42,44 Edita Prakapiene,45 Lina Radzeviciene,46 Rasa Verkauskiene,46 Nicolae Mircea Panduru,6,47 Leif C. -

Supporting Information
Supporting Information Poulogiannis et al. 10.1073/pnas.1009941107 SI Materials and Methods Loss of Heterozygosity (LOH) Analysis of PARK2. Seven microsatellite Bioinformatic Analysis of Genome and Transcriptome Data. The markers (D6S1550, D6S253, D6S305, D6S955, D6S980, D6S1599, aCGH package in R was used to identify significant DNA copy and D6S396) were amplified for LOH analysis within the PARK2 number (DCN) changes in our collection of 100 sporadic CRCs locus using primers that were previously described (8). (1) (Gene Expression Omnibus, accession no. GSE12520). The MSP of the PARK2 Promoter. CpG sites within the PARK2 promoter aCGH analysis of cell lines and liver metastases was derived region were detected using the Methprimer software (http://www. from published data (2, 3). Chromosome 6 tiling-path array- urogene.org/methprimer/index.html). Methylation-specificand CGH was used to identify the smallest and most frequently al- control primers were designed using the Primo MSP software tered regions of DNA copy number change on chromosome 6. (http://www.changbioscience.com/primo/primom.html); bisulfite An integrative approach was used to correlate expression pro- modification of genomic DNA was performed as described pre- files with genomic copy number data from a SNP array from the viously (9). All tumor DNA samples from primary CRC tumors same tumors (n = 48) (4) (GSE16125), using Pearson’s corre- (n = 100) and CRC lines (n = 5), as well as those from the leukemia lation coefficient analysis to identify the relationships between cell lines KG-1a (acute myeloid leukemia, AML), U937 (acute DNA copy number changes and gene expression of those genes lymphoblastic leukemia, ALL), and Raji (Burkitt lymphoma, BL) SssI located within the small frequently altered regions of DCN were screened as part of this analysis. -

Rabbit Anti-Valyl Trna/FITC Conjugated Antibody-SL10504R
SunLong Biotech Co.,LTD Tel: 0086-571- 56623320 Fax:0086-571- 56623318 E-mail:[email protected] www.sunlongbiotech.com Rabbit Anti-valyl tRNA/FITC Conjugated antibody SL10504R-FITC Product Name: Anti-valyl tRNA/FITC Chinese Name: FITC标记的缬氨酰-tRNA合成酶抗体 SYVM_HUMAN; Valine--tRNA ligase, mitochondrial; Valyl-tRNA synthetase; Alias: ValRS; Valyl-tRNA synthetase-like; valyl tRNA; VARS2; KIAA1885; VARS2L; VARSL. Organism Species: Rabbit Clonality: Polyclonal React Species: Human,Mouse,Rat,Pig,Cow,Horse,Sheep, ICC=1:50-200IF=1:50-200 Applications: not yet tested in other applications. optimal dilutions/concentrations should be determined by the end user. Molecular weight: 115kDa Form: Lyophilized or Liquid Concentration: 1mg/ml immunogen: KLH conjugated synthetic peptide derived from human vars2 Lsotype: IgG Purification: affinity purified by Protein A Storage Buffer: 0.01Mwww.sunlongbiotech.com TBS(pH7.4) with 1% BSA, 0.03% Proclin300 and 50% Glycerol. Store at -20 °C for one year. Avoid repeated freeze/thaw cycles. The lyophilized antibody is stable at room temperature for at least one month and for greater than a year Storage: when kept at -20°C. When reconstituted in sterile pH 7.4 0.01M PBS or diluent of antibody the antibody is stable for at least two weeks at 2-4 °C. background: ValRS (valyl-tRNA synthetase), also known as Protein G7a, belongs to the class-I aminoacyl-tRNA synthetase family that includes the related proteins, LeuRS and IleRS. These proteins are large monomeric proteins and play a major role in catalyzing the Product Detail: aminoacylation of tRNA by their cognate amino acid. ValRS joins Val to tRNA(Val) at its synthetic active site. -

Clinical, Biochemical, and Genetic Features Associated with VARS2-Related Mitochondrial Disease
Received: 21 July 2017 Revised: 21 December 2017 Accepted: 28 December 2017 DOI: 10.1002/humu.23398 RESEARCH ARTICLE Clinical, biochemical, and genetic features associated with VARS2-related mitochondrial disease Francesco Bruni1∗,† Ivano Di Meo2∗ Emanuele Bellacchio3 Bryn D. Webb4 Robert McFarland1 Zofia M.A. Chrzanowska-Lightowlers1 Langping He1 Ewa Skorupa5 Isabella Moroni6 Anna Ardissone2,6,7 Anna Walczak8 Henna Tyynismaa9 Pirjo Isohanni9,10 Hanna Mandel11 Holger Prokisch12,13 Tobias Haack13 Penelope E. Bonnen14 Enrico Bertini15 Ewa Pronicka16 Daniele Ghezzi2,17 Robert W. Taylor1∗ Daria Diodato15∗ 1Wellcome Centre for Mitochondrial Research, Institute of Neuroscience, Newcastle University, Newcastle upon Tyne, United Kingdom 2Molecular Neurogenetics Unit, Foundation IRCCS Neurological Institute C. Besta, Milan, Italy 3Genetics and Rare Diseases, Research Division, ‘Bambino Gesù’ Children Hospital, Rome, Italy 4Department of Genetics and Genomic Sciences, Icahn School of Medicine at Mount Sinai, New York, New York 5Department of Biochemistry, Radioimmunology and Experimental Medicine, The Children's Memorial Health Institute, Warsaw, Poland 6Child Neurology Unit, Foundation IRCCS Neurological Institute “C. Besta”, Milan, Italy 7Department of Molecular and Translational Medicine DIMET, University of Milan-Bicocca, Milan, Italy 8Department of Medical Genetics, Centre of Biostructure, Medical University of Warsaw, Warsaw, Poland 9Research Programs Unit, Molecular Neurology, University of Helsinki, Helsinki, Finland 10Department of Pediatric -

Mouse Vars2 Knockout Project (CRISPR/Cas9)
https://www.alphaknockout.com Mouse Vars2 Knockout Project (CRISPR/Cas9) Objective: To create a Vars2 knockout Mouse model (C57BL/6J) by CRISPR/Cas-mediated genome engineering. Strategy summary: The Vars2 gene (NCBI Reference Sequence: NM_175137 ; Ensembl: ENSMUSG00000038838 ) is located on Mouse chromosome 17. 29 exons are identified, with the ATG start codon in exon 1 and the TGA stop codon in exon 29 (Transcript: ENSMUST00000043674). Exon 7~25 will be selected as target site. Cas9 and gRNA will be co-injected into fertilized eggs for KO Mouse production. The pups will be genotyped by PCR followed by sequencing analysis. Note: Exon 7 starts from about 21.13% of the coding region. Exon 7~25 covers 63.05% of the coding region. The size of effective KO region: ~6721 bp. The KO region does not have any other known gene. Page 1 of 9 https://www.alphaknockout.com Overview of the Targeting Strategy Wildtype allele 5' gRNA region gRNA region 3' 16 18 21 1 7 8 9 10 11 12 13 14 15 17 19 20 2223 24 25 29 Legends Exon of mouse Vars2 Knockout region Page 2 of 9 https://www.alphaknockout.com Overview of the Dot Plot (up) Window size: 15 bp Forward Reverse Complement Sequence 12 Note: The 933 bp section upstream of Exon 7 is aligned with itself to determine if there are tandem repeats. No significant tandem repeat is found in the dot plot matrix. So this region is suitable for PCR screening or sequencing analysis. Overview of the Dot Plot (down) Window size: 15 bp Forward Reverse Complement Sequence 12 Note: The 813 bp section downstream of Exon 25 is aligned with itself to determine if there are tandem repeats. -

Physiological and Molecular Consequences of Large Y Chromosome Long Arm Deletions in Mice
Physiological and Molecular Consequences of Large Y Chromosome Long Arm Deletions in Mice Emma Elizabeth Philippa Johnson MRes Emmanuel College Department of Pathology University of Cambridge September 2017 This dissertation is submitted for the degree of Doctor of Philosophy. This dissertation is submitted to the University of Cambridge in accordance with requirements of the degree of Doctor of Philosophy in the School of the Biological Sciences. Page 1 of 331 Page 2 of 331 Physiological and Molecular Consequences of Large Y Chromosome Long Arm Deletions in Mice Emma Elizabeth Philippa Johnson Summary The mammalian Y chromosome contains genes important for male sexual maturity and reproduction. The mouse Y chromosome long arm harbours a number of multi-copy genes whose absence or reduced representation has been linked to sperm defects and offspring sex ratio distortion in favour of females. Understanding the biological mechanisms of sex ratio distortion and related sperm aberrations could not only result in benefits for fertility research, but also in the development of methods for large scale animal breeding pre-implantation sex selection. The distortion has been linked to an intragenomic conflict between the X and Y chromosomes that impacts spermiogenesis. Since the proportion of X- and Y-bearing sperm does not differ in affected animals, and there is no selective destruction of male embryos post-fertilisation, a functional difference must exist between the X- and Y-bearing sperm. This thesis describes the investigation into the physiological and molecular mechanisms of a large Y-chromosome long arm deletion in the mouse model MF1XYRIIIqdel. The examination of physiological characteristics revealed a distinct sperm morphology within the deletion model. -

Gene Expression Imputation Across Multiple Brain Regions Provides Insights Into Schizophrenia Risk
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Hofstra Northwell Academic Works (Hofstra Northwell School of Medicine) Journal Articles 2019 Gene expression imputation across multiple brain regions provides insights into schizophrenia risk L. M. Huckins A. Dobbyn D. M. Ruderfer G. Hoffman W. Wang See next page for additional authors Follow this and additional works at: https://academicworks.medicine.hofstra.edu/articles Part of the Psychiatry Commons Recommended Citation Huckins LM, Dobbyn A, Ruderfer DM, Hoffman G, Wang W, Pardinas AF, Rajagopal VM, Als TD, Malhotra AK, Sullivan PF, . Gene expression imputation across multiple brain regions provides insights into schizophrenia risk. 2019 Jan 01; 51(4):Article 5709 [ p.]. Available from: https://academicworks.medicine.hofstra.edu/articles/5709. Free full text article. This Article is brought to you for free and open access by Donald and Barbara Zucker School of Medicine Academic Works. It has been accepted for inclusion in Journal Articles by an authorized administrator of Donald and Barbara Zucker School of Medicine Academic Works. For more information, please contact [email protected]. Authors L. M. Huckins, A. Dobbyn, D. M. Ruderfer, G. Hoffman, W. Wang, A. F. Pardinas, V. M. Rajagopal, T. D. Als, A. K. Malhotra, P. F. Sullivan, and +343 additional authors This article is available at Donald and Barbara Zucker School of Medicine Academic Works: https://academicworks.medicine.hofstra.edu/articles/5709 HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Nat Genet Manuscript Author . Author manuscript; Manuscript Author available in PMC 2020 February 21. Published in final edited form as: Nat Genet. -

1 Supplementary Material Figure S1. Volcano Plot of Differentially
Supplementary material Figure S1. Volcano Plot of differentially expressed genes between preterm infants fed own mother’s milk (OMM) or pasteurized donated human milk (DHM). Table S1. The 10 most representative biological processes filtered for enrichment p- value in preterm infants. Biological Processes p-value Quantity of DEG* Transcription, DNA-templated 3.62x10-24 189 Regulation of transcription, DNA-templated 5.34x10-22 188 Transport 3.75x10-17 140 Cell cycle 1.03x10-13 65 Gene expression 3.38x10-10 60 Multicellular organismal development 6.97x10-10 86 1 Protein transport 1.73x10-09 56 Cell division 2.75x10-09 39 Blood coagulation 3.38x10-09 46 DNA repair 8.34x10-09 39 Table S2. Differential genes in transcriptomic analysis of exfoliated epithelial intestinal cells between preterm infants fed own mother’s milk (OMM) and pasteurized donated human milk (DHM). Gene name Gene Symbol p-value Fold-Change (OMM vs. DHM) (OMM vs. DHM) Lactalbumin, alpha LALBA 0.0024 2.92 Casein kappa CSN3 0.0024 2.59 Casein beta CSN2 0.0093 2.13 Cytochrome c oxidase subunit I COX1 0.0263 2.07 Casein alpha s1 CSN1S1 0.0084 1.71 Espin ESPN 0.0008 1.58 MTND2 ND2 0.0138 1.57 Small ubiquitin-like modifier 3 SUMO3 0.0037 1.54 Eukaryotic translation elongation EEF1A1 0.0365 1.53 factor 1 alpha 1 Ribosomal protein L10 RPL10 0.0195 1.52 Keratin associated protein 2-4 KRTAP2-4 0.0019 1.46 Serine peptidase inhibitor, Kunitz SPINT1 0.0007 1.44 type 1 Zinc finger family member 788 ZNF788 0.0000 1.43 Mitochondrial ribosomal protein MRPL38 0.0020 1.41 L38 Diacylglycerol -

Skeletal Phenotypes Due to Abnormalities in Mitochondrial Protein Homeostasis and Import
International Journal of Molecular Sciences Review Skeletal Phenotypes Due to Abnormalities in Mitochondrial Protein Homeostasis and Import Tian Zhao 1, Caitlin Goedhart 2, Gerald Pfeffer 3, Steven C Greenway 4, Matthew Lines 2, Aneal Khan 5, A Micheil Innes 2 and Timothy E Shutt 1,* 1 Departments of Medical Genetics and Biochemistry & Molecular Biology, Cumming School of Medicine, Alberta Children’s Hospital Research Institute, Hotchkiss Brain Institute, University of Calgary, Calgary, AB T2N 4N1, Canada; [email protected] 2 Departments of Pediatrics and Medical Genetics, Cumming School of Medicine, Alberta Children’s Hospital Research Institute, Hotchkiss Brain Institute, University of Calgary, Calgary, AB T2N 4N1, Canada; [email protected] (C.G.); [email protected] (M.L.); [email protected] (A.M.I) 3 Departments of Clinical Neurosciences and Medical Genetics, Cumming School of Medicine, Hotchkiss Brain Institute, Alberta Child Health Research Institute, University of Calgary, Calgary, AB T2N 4N1, Canada; gerald.pfeff[email protected] 4 Departments of Pediatrics, Cardiac Sciences and Biochemistry & Molecular Biology, Cumming School of Medicine, Alberta Children’s Hospital Research Institute and Libin Cardiovascular Institute, University of Calgary, Calgary, AB T2N 4N1, Canada; [email protected] 5 Departments of Pediatrics and Medical Genetics, Cumming School of Medicine, Alberta Children’s Hospital Research Institute, University of Calgary, Calgary, AB T3B 6A8, Canada; [email protected] * Correspondence: [email protected] Received: 18 September 2020; Accepted: 3 November 2020; Published: 6 November 2020 Abstract: Mitochondrial disease represents a collection of rare genetic disorders caused by mitochondrial dysfunction. These disorders can be quite complex and heterogeneous, and it is recognized that mitochondrial disease can affect any tissue at any age. -

Histocompatibility Complex
Proc. Natl. Acad. Sci. USA Vol. 93, pp. 9096-9101, August 1996 Immunology Chromosomal localization of the proteasome Z subunit gene reveals an ancient chromosomal duplication involving the major histocompatibility complex (evolution/synteny) MASANORI KASAHARA*t, MASARU HAYASHI*, KEIJI TANAKAt, HIDETOSHI INOKO§, KIMIHIKO SUGAYAV, ToSHIMICHI IKEMURAS, AND TERUO ISHIBASHI* *Department of Biochemistry, Hokkaido University School of Medicine, Sapporo 060, Japan; *Institute for Enzyme Research, The University of Tokushima, Tokushima 770, Japan; §Division of Molecular Life Science, Tokai University School of Medicine, Isehara 259-11, Japan; and IDepartment of Evolutionary Genetics, National Institute of Genetics, and The Graduate University for Advanced Studies, Mishima 411, Japan Communicated by D. Bernard Amos, Duke University Medical Center, Durham, NC, May 22, 1996 (received for review March 20, 1996) ABSTRACT Proteasomes are the multi-subunit protease antigen presentation, presumably by altering the cleavage thought to play a key role in the generation of peptides specificities of the proteasome (15-17). presented by major histocompatibility complex (MHC) class Recently, Hisamatsu et al. (18) identified a third pair of I molecules. When cells are stimulated with interferon y, two structurally similar proteasome (3-type subunits, designated MHC-encoded subunits, low molecular mass polypeptide MECL1 and Z, whose expression is regulated reciprocally by (LMP) 2 and LMP7, and the MECL1 subunit encoded outside IFN-y. When cells are stimulated with IFN--y, the MECL1 the MHC are incorporated into the proteasomal complex, subunit is thought to be incorporated into the proteasome by presumably by displacing the housekeeping subunits desig- displacing the housekeeping Z subunit. Unlike the LMP2 and nated Y, X, and Z, respectively.