Sir Gordon Holmes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

George Streeter
NATIONAL ACADEMY OF SCIENCES G EORGE LINIUS S TREETER 1873—1948 A Biographical Memoir by GE O R G E W . CORNER Any opinions expressed in this memoir are those of the author(s) and do not necessarily reflect the views of the National Academy of Sciences. Biographical Memoir COPYRIGHT 1954 NATIONAL ACADEMY OF SCIENCES WASHINGTON D.C. GEORGE LINIUS STREETER 1873-1948 BY GEORGE W. CORNER George Linius Streeter was generally recognized during the latter years of his life by the embryologists of the world as their leader in the study of human embryology. From 1914 until his death in 1948 he was connected with the Department of Embryology of the Carnegie Institution of Washington, of which he was Director for 23 years (1917-1940). So fully indeed did he plan and lead the work of the Baltimore embryo- logical laboratory that his fame and that of his department are scarcely separable. Dr. Streeter was born January 12, 1873 at Johnstown in western New York, whither his family, of English descent, had migrated by way of New England. His father was a leader in the chief industry of that region, glove manufacturing. After being graduated from Union College in 1895 ne studied at the College of Physicians and Surgeons of Columbia University and took the degree of Doctor of Medicine in 1899. While in medi- cal school his interest in human anatomy was aroused by Columbia's accomplished professor of that subject, George S. Huntington. After an internship in Roosevelt Hospital, New York City, Streeter became assistant to Dr. -

Introduction to the Sixteenth C.U. Arie¨Ns Kappers Lecture
Progress in Brain Research, Vol. 147 ISSN 0079-6123 Copyright ß 2005 Elsevier BV. All rights reserved CHAPTER 4 Introduction to the sixteenth C.U. Arie¨ns Kappers lecture D.F. Swaab*, J. van Pelt and M.A. Hofman Netherlands Institute for Brain Research, Meibergdreef 33, 1105 AZ Amsterdam, The Netherlands Professor Dennis D.M. O’Leary was invited to Royal Society, the ‘‘Central Commission for Brain deliver the sixteenth C.U. Arie¨ns Kappers Lecture Research’’ was constituted. This so-called ‘‘Brain during the 23rd International Summer School of Commission’’ set itself the task of ‘‘... organizing a Brain Research on 25 August 2003, for his out- network of institutions throughout the civilized world, standing achievements in unraveling the molecular dedicated to the study of the structure and functions control of cortical development. The C.U. Arie¨ns of the central organ....’’ Several governments respon- Kappers Award was created to honor the first ded to this ambition by founding brain research director of the Netherlands Institute for Brain institutes (Table 2), among which was the Central Research. The award is presented approximately Institute for Brain Research in the Netherlands, which once a year to a leading and outstanding neuroscien- opened its doors on 8 June 1909, in the presence of the tist, who is invited to give the C.U. Arie¨ns Kappers Nobel laureate Dr. Camillo Golgi. Lecture (Table 1). Prof. C.U. Arie¨ns Kappers became the first Cornelius Ubbo Arie¨ns Kappers was born in director of the institute, a position he held until his Groningen in 1877. -

Franz Nissl (1860-1919), Noted Neuropsychiatrist and Neuropathologist, Staining the Neuron, but Not Limiting It
Dement Neuropsychol 2019 September;13(3):352-355 History Note http://dx.doi.org/10.1590/1980-57642018dn13-030014 Franz Nissl (1860-1919), noted neuropsychiatrist and neuropathologist, staining the neuron, but not limiting it Marleide da Mota Gomes1 ABSTRACT. Franz Alexander Nissl carried out studies on mental and nervous disorders, as a clinician, but mainly as a pathologist, probably the most important of his time. He recognized changes in glial cells, blood elements, blood vessels and brain tissue in general, achieving this by using a special blue stain he himself developed – Nissl staining, while still a medical student. However, he did not accept the neuron theory supported by the new staining methods developed by Camillo Golgi and Santiago Ramón y Cajal. Nissl had worked with the crème de la crème of German neuropsychiatry, including Alois Alzheimer, besides Emil Kraepelin, Korbinian Brodmann and Walther Spielmeyer. He became (1904), Kraepelin’s successor as Professor of Psychiatry and Director of the Psychiatric Clinic, in Heidelberg. Moreover, in 1918, the year before Nissl´s death, Kraepelin offered him a research position as head of the Histopathology Department of the newly founded “Deutsche Forschungsanstalt fur Psychiatrie” of the Max Planck Institute for Psychiatry, in Munich. Key words: Franz Nissl, neuropathology, staining method, neuron theory. FRANZ NISSL (1860-1919), NOTÁVEL NEUROPSIQUIATRA E NEUROPATOLOGISTA, TINGINDO O NEURÔNIO, MAS NÃO O LIMITANDO RESUMO. Franz Alexander Nissl realizou estudos sobre transtornos mentais e nervosos, como clínico, mas principalmente como patologista, provavelmente o mais importante de seu tempo. Ele reconheceu mudanças nas células gliais, elementos sangüíneos, vasos sangüíneos e tecido cerebral em geral, realizando-o por meio de um corante azul especial desenvolvida por ele mesmo – coloração de Nissl, ainda como estudante de medicina. -

The Neuro Nobels
NEURO NOBELS Richard J. Barohn, MD Gertrude and Dewey Ziegler Professor of Neurology University Distinguished Professor Vice Chancellor for Research President Research Institute Research & Discovery Director, Frontiers: The University of Kansas Clinical and Translational Science Grand Rounds Institute February 14, 2018 1 Alfred Nobel 1833-1896 • Born Stockholm, Sweden • Father involved in machine tools and explosives • Family moved to St. Petersburg when Alfred was young • Father worked on armaments for Russians in the Crimean War… successful business/ naval mines (Also steam engines and eventually oil).. made and lost fortunes • Alfred and brothers educated by private teachers; never attended university or got a degree • Sent to Sweden, Germany, France and USA to study chemical engineering • In Paris met the inventor of nitroglycerin Ascanio Sobrero • 1863- Moved back to Stockholm and worked on nitro but too dangerous.. brother killed in an explosion • To make it safer to use he experimented with different additives and mixed nitro with kieselguhr, turning liquid into paste which could be shaped into rods that could be inserted into drilling holes • 1867- Patented this under name of DYNAMITE • Also invented the blasting cap detonator • These inventions and advances in drilling changed construction • 1875-Invented gelignite, more stable than dynamite and in 1887, ballistics, predecessor of cordite • Overall had over 350 patents 2 Alfred Nobel 1833-1896 The Merchant of Death • Traveled much of his business life, companies throughout Europe and America • Called " Europe's Richest Vagabond" • Solitary man / depressive / never married but had several love relationships • No children • This prompted him to rethink how he would be • Wrote poetry in English, was considered remembered scandalous/blasphemous. -
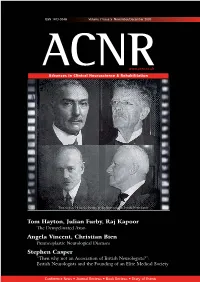
ACNRND07:Layout 1
ISSN 1473-9348 Volume 7 Issue 5 November/December 2007 ACNRwww.acnr.co.uk Advances in Clinical Neuroscience & Rehabilitation Turn to page 16 for the history of the Association of British Neurologists Tom Hayton, Julian Furby, Raj Kapoor The Demyelinated Axon Angela Vincent, Christian Bien Paraneoplastic Neurological Diseases Stephen Casper “Then why not an Association of British Neurologists?”: British Neurologists and the Founding of an Elite Medical Society Conference News • Journal Reviews • Book Reviews • Diary of Events Pen & Pump Ad V2 210x297 4/9/07 12:12 Page 1 ON &ON&ON&ON &ON&ON&ON& APO-go: treatment for both PREDICTABLE and UNPREDICTABLE symptoms of Parkinson’s disease Predictable symptoms: Use APO-go Pen early in treatmenttreatment plan for rapid reversal of impending “off’s”. Simple, easy to use sc injection Positive NICE review: “Intermittent apomorphine injections may be used to reduce “off” time in people with PD with severe motor complications.” Unpredictable symptoms: Use continuous APO-go infusion for full waking-day cover. Continuous dopaminergic stimulation – reduces pulsatile treatment-related complications including “on-off” fl uctuations Positive NICE review: “Continuous subcutaneous infusions of apomorphine may be used to reduce “off” time and dyskinesia in people with PD with severe motor complications.” Make the switch and turn their “off’s” to “on” ABRIDGED PRESCRIBING INFORMATION in patients with Parkinson’s disease. Patients must be informed of this and advised to exercise caution while Consult Summary of Product Characteristics before prescribing. Uses The treatment of disabling motor driving or operating machines during treatment with apomorphine. Haematology tests should be undertaken fluctuations (‘’on-off’’ phenomena) in patients with Parkinson’s disease which persist despite individually titrated at regular intervals as with levodopa when given concomitantly with apomorphine. -

The Study of Primate Brain Evolution: Where Do We Go from Here?
Page 1 Jerison (2001 draft of Festschrift Epilogue [Comments for 2007 pdf in square brackets] The Study of Primate Brain Evolution: Where Do We Go From Here? Harry J. Jerison I am pleased to accept the title that Dean Falk and Kathleen Gibson assigned me for this concluding essay. And of course I thank them for arranging the meeting of the American Association of Physical Anthropologists in my honor. Most of all I must thank the contributors at that meeting and the others who have taken time to prepare the chapters in this book, which commemorates that meeting. In my judgment it would be inappropriate for me to comment on those excellent chapters, to argue with some of them or to agree with others. The chapters speak well for themselves, I will leave commentary to the journals, such as Current Anthropology or Brain and Behavior Sciences, that specialize in it. It has been a great pleasure to be involved with these activities. I will depart from my assignment in three ways. First I must write about where I would go from here rather than prescribe for others. The chapters in this book present better prescriptions than I am competent to offer for the route our field as a whole can take. Second, I would like to write about where we have been, because my particular route is so much one involving the fossil evidence that I think it takes some explaining. Finally, I have to write about more than only primates, because my emphasis has been and continues to be on the evolution of the vertebrate brain, including the primates among the mammals. -

Tilly Edinger and the Science of Paleoneurology
Brain Research Bulletin, Vol. 48, No. 4, pp. 351–361, 1999 Copyright © 1999 Elsevier Science Inc. Printed in the USA. All rights reserved 0361-9230/99/$–see front matter PII S0361-9230(98)00174-9 HISTORY OF NEUROSCIENCE The gospel of the fossil brain: Tilly Edinger and the science of paleoneurology Emily A. Buchholtz1* and Ernst-August Seyfarth2 1Department of Biological Sciences, Wellesley College, Wellesley, MA, USA; and 2Zoologisches Institut, Biologie-Campus, J.W. Goethe-Universita¨ t, D-60054 Frankfurt am Main, Germany [Received 21 September 1998; Revised 26 November 1998; Accepted 3 December 1998] ABSTRACT: Tilly Edinger (1897–1967) was a vertebrate paleon- collection and description of accidental finds of natural brain casts, tologist interested in the evolution of the central nervous that is, the fossilized sediments filling the endocrania (and spinal system. By combining methods and insights gained from com- canals) of extinct animals. These can reflect characteristic features parative neuroanatomy and paleontology, she almost single- of external brain anatomy in great detail. handedly founded modern paleoneurology in the 1920s while Modern paleoneurology was founded almost single-handedly working at the Senckenberg Museum in Frankfurt am Main. Edinger’s early research was mostly descriptive and conducted by Ottilie (“Tilly”) Edinger in Germany in the 1920s. She was one within the theoretical framework of brain evolution formulated of the first to systematically investigate, compare, and summarize by O. C. Marsh in the late 19th -

STAHNISCH Frank W – CV May 31, 2020 the University of Calgary Faculty of Arts / Cumming School of Medicine CURRICULUM VITAE
STAHNISCH Frank W – CV May 31, 2020 The University of Calgary Faculty of Arts / Cumming School of Medicine CURRICULUM VITAE I. BIOGRAPHICAL DATA Prof. Frank W. Stahnisch University of Calgary Teaching, Research and Wellness Building Room 3E41 3280 Hospital Drive NW Calgary, AB, Canada T2N 4Z6 Telephone: 403-210-6290 Fax: 403-270-7307 Email: [email protected] https://hom.ucalgary.ca http://ucalgary.ca/communityhealthsciences Present Rank: Full Professor (“tenured”) Additional Alberta Medical Foundation/Hannah Professorship Affiliation: in the History of Medicine and Health Care Department: History Faculty: Arts & Department: Community Health Sciences Faculty: Cumming School of Medicine Supervisory PhD and MA, Faculty of Arts* Privileges: PhD and MSc, Cumming School of Medicine* **Dean’s Renewal for next Five-Year Term (2019-24) Institution: The University of Calgary II. ACADEMIC RECORD 1. Vordiplom (equivalent to a B.A., Johann Wolfgang Goethe University of Frankfurt am Main), Germany, 1992 2. Physicum (equivalent to a B.Sc., Johann Wolfgang Goethe University of Frankfurt am Main), Germany, 1993 3. Graduation as Master of Science (M. Sc.) in Philosophy of Science, University of Edinburgh (with distinction), United Kingdom, 1995 4. Medizinisches Staatsexamen (equivalent to an MD), Humboldt University of Berlin, Germany, 1998 May 31, 2020 1 STAHNISCH Frank W – CV 5. Medical Licence to Practice (Approbation), Department of Health, Berlin, Germany, 2000 6. Graduation as Doctor medicinae (Dr. med. – equivalent to a PhD) in History of Medicine, Free University of Berlin (magna cum laude), Germany, 2001 III. AWARDS AND DISTINCTIONS 03/2020 INVITED Endowed Lecture: Sebastian K. Littmann Keynote Lecture to the Department of Psychiatry at the University of Calgary Cumming School of Medicine, Foothills Medical Centre Auditorium, Calgary, Alberta (Canada). -

Ludwig Edinger.~) (1855---1918.) Von Kurt Goldstein
Ludwig Edinger.~) (1855---1918.) Von Kurt Goldstein. (Eingegangen am 15. Juli 1918.) M.H. So sehr es mir aueh nur mit den Gefiihlen des Schmerzes mSglich ist, fiber meinen verstorbenen Lehrer zu Ihnen zu sprechen, so sehr erscheint es mir andrerseits eine besonders ehrenvolle Aufgabe im ~rztlichen Verein einen Uberblick fiber das Lebenswerk Ludwig Edingers zu geben -- yon der Stelle aus, vonder der Verstorbene so viele seiner neuen Entdeckungen zuerst mitgeteilt hat. Eine ehren- volle Aufgabe, aber keine leiehte -- gilt es doch eine schier unfiberseh- bare Menge von Einzeluntersucl~ungen, von Ideen, deren Problematik noch gar nieht zu fibersehen, geschweige denn zu erschSpfen ist, die sich alle an den Namen Edinger knfipfen, in einen einheitlichen Rah- men zusammenzubringen. Wenn mir dies doch gelingen sollte, so liegt dies an dem einheitliehen Grundzug, der, wie wir spater sehen wer- den, alle die Arbeiten und Gedanken Edingers durchzieht. Der Lebensgang Ludwig Edingers ist schnell geschildert. Er ist 1855 in Worms geboren, studierte in Heidelberg und Stra[tburg. Unter dem Einflui] so ausgezeiehneter Lehrer wie Gegenbaur und Waldeyer erwachte frfihzeitig sein Interesse ffir die Anatomie und Biologie. So entstanden seine ersten wissensehaftlichen Arbeiten: die Dissertation ,,Uber die Schleimhaut des Fisehdarmes (usw.)" 18761), die ,,Untersuehung fiber die Endigung der Haut- nerven bei Pterotrachea ''2) und ,,Uber die Drfisenzellen des Magens besonders beim Menschen"3). Naeh Beeudigung seiner Stuclienzeit land E d i n g e r nieht die seinen Neigungen zur vergleichenden Anatomie und Biologie entspreehende Assistentenstelle; er mul~te eine klinisehe Stelle annehmen. Er be- schreibt in seinem Aufsatze zu Kussmauls 60. Geburtstage 121) sehr eindringlich seinen Schmerz darfiber; glaubte er doch, dadureh von seinem eigenttichen Berufe, dem des Anatomen und Biologen, abzu- *) Nach einem bei der Trauel~eicr fiir Ludwig Edinger im ~rztlichen Verein zu Frankfurt a. -

Ergab Sich Bald Ein Merkwürdiges Hindernis ... « Zur Aktualität Von Ludwig Edingers Neurowissenschaftlichem Projekt
Wissenschafts- und Universitätsgeschichte »... ergab sich bald ein merkwürdiges Hindernis ... « Zur Aktualität von Ludwig Edingers neurowissenschaftlichem Projekt udwig Edinger (1855–1918) Lgalt als »die größte Autorität der vergleichenden Neurologie« /1/. Un- ter Neurologie verstand man sei- nerzeit alle Fächer, die zur Lehre vom Nervensystem beitrugen. In die- sem Sinne konzipierte Edinger sein Neurologisches Institut als interdiszip- linäre Arbeitsstätte zur Erforschung des Nervensystems. Neuroanatomie und Neuropathologie erhielten hier 1907 jeweils eigene Abteilungen, Aquarien und Terrarien standen für tierpsychologische Beobachtungen zur Verfügung, und Edinger hatte als Leiter der ersten Frankfurter Po- liklinik für Nervenkranke das ganze Spektrum neurologischer Krank- heitsbilder vor Augen. 1910 grün- dete er überdies einen Psychologi- schen Verein, in dem Mediziner mit Zoologen und Psychologen zusam- menarbeiteten. Durch Interdisziplinarität eine ■1 Das von Lovis Brücke zwischen Hirnforschung Corinth (1858 – und Psychologie zu schlagen, war 1925) gefertigte das erklärte Ziel Edingers, und Ölgemälde Ludwig Edingers zeichnete sein Institut unter den (145 × 110 cm) »interakademischen Hirnforschungs- entstand 1909 instituten« aus, die sich nach der und gilt als eines Jahrhundertwende zur »Brain der bedeutendsten Commission« zusammengeschlos- Arztporträts des sen hatten. Der Erste Weltkrieg setz- 20. Jahrhunderts. te dieser internationalen Kooperati- Das Bild gehört heute zu den Be- on ein Ende, die erst in den 1960er ständen des His- Jahren als »Neuroscience« wieder torischen Muse- institutionelle Strukturen finden ums in Frankfurt sollte. Allerdings ist es bisher nicht am Main. gelungen, die konzeptionell unver- bundene Praxis der einzelnen neu- rowissenschaftlichen Fächer in eine dass ein Teil der vom Nervensystem portional ausbildende Neuhirn Disziplin zu überführen, die das geleisteten Arbeit dem Träger be- (Neencephalon), auf dem die höhe- Verhältnis von Gehirn und Be- wusst werden kann«. -

Der Neurologe Ludwig Edinger Und Die Universität Frankfurt Am Main
Der Neurologe Ludwig Edinger und die Universität Frankfurt am Main Udo Benzenhöfer Ludwig Edinger zählt zweifellos zu den bedeutendsten Frankfurter Universitätsmedizinern. In der vorliegenden Arbeit soll nach einem kurzen Überblick über Leben und Werk1 der Komplex „Edinger und die Universität Frankfurt“ näher betrachtet werden. In einem Exkurs wird Edinger als Kritiker bestimmter Bestrebungen der Medizin seiner Zeit konturiert. Leben und Werk im Überblick Ludwig Edinger wurde am 13.4.1855 in Worms geboren (HW S. 68). Er stammte aus einer wohlhabenden jüdischen Familie, sein Vater war Textilfabrikant, seine Mutter Arzttochter (HW S. 68). Er hatte vier Geschwister (HW S. 68f.). 1872 machte Edinger in Worms das Abitur (HW S. 69). Er studierte Medizin in Heidelberg (1872-1874) und Straßburg (1874-1877) (HW S. 69). 1876 beendete er bei Wil- helm Waldeyer in Straßburg seine Dissertation „Über die Schleim- haut des Fischdarmes“ (HW S. 68, E S. 38, K S. 33; die Arbeit wurde noch 1876 im Archiv für mikroskopische Anatomie veröffentlicht). Laut Emisch (S. 38) legte Edinger im Herbst 1876 das Doktorexa- men ab. Die Approbation erhielt er nach Ablegen der ärztlichen Prüfung erst im März 1877 (E S. 38; S. 39: Faksimile der Approba- 1 Die Darstellung erfolgte im Wesentlichen auf der Grundlage von Emisch 1991 (abgekürzt: E), Heuer/Wolf 1997 (abgekürzt: HW), Kreft 2005 (abgekürzt: K) und der 2005 veröffentlichten Autobiographie (Edinger 2005, abgekürzt: EA). 18 tionsurkunde). 1877/78 absolvierte Edinger seinen Militärdienst in Worms bzw. in Straßburg (HW S. 40). 1878/79 war er Assistent an der Medizinischen Universitätsklinik in Straßburg unter Adolf Kussmaul (HW S. 70). -

Contents 100 Years of MPI-BR 1
Friends of the newsletter 1/2014 Max Planck Institute for Brain Research newsletter 1/2014 contents 100 years of MPI-BR 1 Exhibition 2 News from our Institute 3 FeM Mädchenhaus 4 Upcoming Neuroscience Lectures and Symposia Photo: HG Esch Photography HG Esch Photo: 100 years of MPI-BR May 28, we celebrated the official opening of the new Institute‘s building as well as hundred yearson of MPI for Brain Research (MPI-BR) with a morning of talks and the opening of our commemorative exhibit, minds in motion (see below), the unveiling of a commissioned piece of art, Mindscape, by Gayle Chong Kwan (www.gaylechongkwan.com) and a book, minds in motion – 100 years, chronicling the history and future directions of our Institute. The morning talks in the Lecture Hall of the new building included presentations from Boris Rhein (Hessen Minister of Science and Arts), as well as Gunter Henn (architect of the building), Herbert Jäckle (Vice President of the Max Planck Society) and a joint lecture by Wolf Singer and Heinz Wässle (Emeritus Directors at the Institute) about the Institute‘s history. Musical intermezzos were provided by Alex Jacobowitz (www.alexjacobowitz.com) who played the xylophone. For more information please visit our website www.brain.mpg.de/mindsinmotion Impression of the official celebrations Photo: Tracy Yamawaki Tracy Photo: on May 28, 2014 newsletter 1/2014 The Exhibition “minds in motion“ exhibition “100 years of MPI, minds in motion“ was opened theon May 28, 2014. The exhibition is located in the public area of the Max Planck Institute for Brain Research and can be visi- ted during week days between 8.00-18.00 hours.