(2):43-53 Soil Transmitted Helminths and Schistos
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Districts of Ethiopia
Region District or Woredas Zone Remarks Afar Region Argobba Special Woreda -- Independent district/woredas Afar Region Afambo Zone 1 (Awsi Rasu) Afar Region Asayita Zone 1 (Awsi Rasu) Afar Region Chifra Zone 1 (Awsi Rasu) Afar Region Dubti Zone 1 (Awsi Rasu) Afar Region Elidar Zone 1 (Awsi Rasu) Afar Region Kori Zone 1 (Awsi Rasu) Afar Region Mille Zone 1 (Awsi Rasu) Afar Region Abala Zone 2 (Kilbet Rasu) Afar Region Afdera Zone 2 (Kilbet Rasu) Afar Region Berhale Zone 2 (Kilbet Rasu) Afar Region Dallol Zone 2 (Kilbet Rasu) Afar Region Erebti Zone 2 (Kilbet Rasu) Afar Region Koneba Zone 2 (Kilbet Rasu) Afar Region Megale Zone 2 (Kilbet Rasu) Afar Region Amibara Zone 3 (Gabi Rasu) Afar Region Awash Fentale Zone 3 (Gabi Rasu) Afar Region Bure Mudaytu Zone 3 (Gabi Rasu) Afar Region Dulecha Zone 3 (Gabi Rasu) Afar Region Gewane Zone 3 (Gabi Rasu) Afar Region Aura Zone 4 (Fantena Rasu) Afar Region Ewa Zone 4 (Fantena Rasu) Afar Region Gulina Zone 4 (Fantena Rasu) Afar Region Teru Zone 4 (Fantena Rasu) Afar Region Yalo Zone 4 (Fantena Rasu) Afar Region Dalifage (formerly known as Artuma) Zone 5 (Hari Rasu) Afar Region Dewe Zone 5 (Hari Rasu) Afar Region Hadele Ele (formerly known as Fursi) Zone 5 (Hari Rasu) Afar Region Simurobi Gele'alo Zone 5 (Hari Rasu) Afar Region Telalak Zone 5 (Hari Rasu) Amhara Region Achefer -- Defunct district/woredas Amhara Region Angolalla Terana Asagirt -- Defunct district/woredas Amhara Region Artuma Fursina Jile -- Defunct district/woredas Amhara Region Banja -- Defunct district/woredas Amhara Region Belessa -- -
Final Report
Final report July 2017 – April 2018 Wag Himra Zone, Amhara Region Ethiopia ACKNOWLEDGEMENTS The nutrition causal analysis Link NCA in Sekota and Dehana woredas, Wag Himra zone, Amhara region, Ethiopia was funded by the European Union. The study was conducted by Link NCA Analysts, Joanne Chui and Lenka Blanárová, under the supervision of study’s focal points: Amelia Lyons and Vincent Veillaud, Deputy Country Directors for Programs, Action Against Hunger, Ethiopia, and Janis Differt, Technical Advisor Food Security and Livelihoods, Action Against Hunger, France, with valuable contributions from the pool of Technical Advisors at Action Against Hunger, France and Action Against Hunger, Ethiopia, namely Celine Soulier, Xuan Phan, Tom Heath and Jogie Abucejo Agbogan. The Link NCA team wishes to express their thanks to all those who have contributed to this study and/or facilitated its development, in particular: To local authorities for their tireless dedication in the fight against undernutrition and their unwavering support over the course of the study; to Mr. Gardie Nigatu Abuye and his team for their absolute availability and support as well as creative troubleshooting during all stages of the study. To all technical experts who attended the Link NCA technical workshops, including the entire team of technical advisors and project managers at Action Against Hunger, Ethiopia, representatives of partner organizations, such as Danish Church Aid, Organization for Rehabilitation & Development in Amhara, Plan International and Save the Children, as well as all dedicated staff representing woreda and zone offices in their respective domains, for sharing their expertise and hence contributing to the high quality of the study. -
20210714 Access Snapshot- Tigray Region June 2021 V2
ETHIOPIA Tigray: Humanitarian Access Snapshot (July 2021) As of 31 July 2021 The conflict in Tigray continues despite the unilateral ceasefire announced by the Ethiopian Federal Government on 28 June, which resulted in the withdrawal of the Ethiopian National Overview of reported incidents July Since Nov July Since Nov Defense Forces (ENDF) and Eritrea’s Defense Forces (ErDF) from Tigray. In July, Tigray forces (TF) engaged in a military offensive in boundary areas of Amhara and Afar ERITREA 13 153 2 14 regions, displacing thousands of people and impacting access into the area. #Incidents impacting Aid workers killed Federal authorities announced the mobilization of armed forces from other regions. The Amhara region the security of aid Tahtay North workers Special Forces (ASF), backed by ENDF, maintain control of Western zone, with reports of a military Adiyabo Setit Humera Western build-up on both sides of the Tekezi river. ErDF are reportedly positioned in border areas of Eritrea and in SUDAN Kafta Humera Indasilassie % of incidents by type some kebeles in North-Western and Eastern zones. Thousands of people have been displaced from town Central Eastern these areas into Shire city, North-Western zone. In line with the Access Monitoring and Western Korarit https://bit.ly/3vcab7e May Reporting Framework: Electricity, telecommunications, and banking services continue to be disconnected throughout Tigray, Gaba Wukro Welkait TIGRAY 2% while commercial cargo and flights into the region remain suspended. This is having a major impact on Tselemti Abi Adi town May Tsebri relief operations. Partners are having to scale down operations and reduce movements due to the lack Dansha town town Mekelle AFAR 4% of fuel. -

Modeling Malaria Cases Associated with Environmental Risk Factors in Ethiopia Using Geographically Weighted Regression
MODELING MALARIA CASES ASSOCIATED WITH ENVIRONMENTAL RISK FACTORS IN ETHIOPIA USING GEOGRAPHICALLY WEIGHTED REGRESSION Berhanu Berga Dadi i MODELING MALARIA CASES ASSOCIATED WITH ENVIRONMENTAL RISK FACTORS IN ETHIOPIA USING THE GEOGRAPHICALLY WEIGHTED REGRESSION MODEL, 2015-2016 Dissertation supervised by Dr.Jorge Mateu Mahiques,PhD Professor, Department of Mathematics University of Jaume I Castellon, Spain Ana Cristina Costa, PhD Professor, Nova Information Management School University of Nova Lisbon, Portugal Pablo Juan Verdoy, PhD Professor, Department of Mathematics University of Jaume I Castellon, Spain March 2020 ii DECLARATION OF ORIGINALITY I declare that the work described in this document is my own and not from someone else. All the assistance I have received from other people is duly acknowledged, and all the sources (published or not published) referenced. This work has not been previously evaluated or submitted to the University of Jaume I Castellon, Spain, or elsewhere. Castellon, 30th Feburaury 2020 Berhanu Berga Dadi iii Acknowledgments Before and above anything, I want to thank our Lord Jesus Christ, Son of GOD, for his blessing and protection to all of us to live. I want to thank also all consortium of Erasmus Mundus Master's program in Geospatial Technologies for their financial and material support during all period of my study. Grateful acknowledgment expressed to Supervisors: Prof.Dr.Jorge Mateu Mahiques, Universitat Jaume I(UJI), Prof.Dr.Ana Cristina Costa, Universidade NOVA de Lisboa, and Prof.Dr.Pablo Juan Verdoy, Universitat Jaume I(UJI) for their immense support, outstanding guidance, encouragement and helpful comments throughout my thesis work. Finally, but not least, I would like to thank my lovely wife, Workababa Bekele, and beloved daughter Loise Berhanu and son Nethan Berhanu for their patience, inspiration, and understanding during the entire period of my study. -

Ethiopia Final Evaluation Report
ETHIOPIA: Mid-Term Evaluation of UNCDF’s Local Development Programme Submitted to: United Nations Capital Development Fund Final Evaluation Report 23 July 2007 Prepared by: Maple Place North Woodmead Business Park 145 Western Service Road Woodmead 2148 Tel: +2711 802 0015 Fax: +2711 802 1060 www.eciafrica.com UNITED NATIONS DEVELOPMENT FUND EVALUATION REPORT TABLE OF CONTENTS 1. PROJECT SUMMARY 1 2. PURPOSE OF THE EVALUATION 2 Purpose of the evaluation 2 Programme Cycle 2 3. EVALUATION METHODOLOGY 3 Methodology and tools used 3 Work plan 4 Team composition 5 4. PROGRAMME PROFILE 6 Understanding the context 6 Donor Interventions in Amhara Region 7 Programme Summary 8 Programme Status 9 5. KEY EVALUATION FINDINGS 13 Results achievement 13 Sustainability of results 21 Factors affecting successful implementation & results achievement 24 External Factors 24 Programme related factors 24 Strategic position and partnerships 26 Future UNCDF role 27 6. LESSONS 28 Programme-level lessons 28 7. RECOMMENDATIONS 29 Results achievement 29 Sustainability of results 29 Factors affecting successful implementation and results achievement 30 Strategic positioning and partnerships 31 Future UNCDF role 31 “The analysis and recommendations of this report do not necessarily reflect the view of the United Nations Capital Development Fund, its Executive Board or the United Nations Member States. This is an independent publication of UNCDF and reflects the views of its authors” PREPARED BY ECIAFRICA CONSULTING (PTY) LTD, PROPRIETARY AND CONFIDENTIAL i 2007/05/24 -
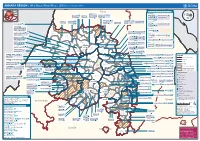
AMHARA REGION : Who Does What Where (3W) (As of 13 February 2013)
AMHARA REGION : Who Does What Where (3W) (as of 13 February 2013) Tigray Tigray Interventions/Projects at Woreda Level Afar Amhara ERCS: Lay Gayint: Beneshangul Gumu / Dire Dawa Plan Int.: Addis Ababa Hareri Save the fk Save the Save the df d/k/ CARE:f k Save the Children:f Gambela Save the Oromia Children: Children:f Children: Somali FHI: Welthungerhilfe: SNNPR j j Children:l lf/k / Oxfam GB:af ACF: ACF: Save the Save the af/k af/k Save the df Save the Save the Tach Gayint: Children:f Children: Children:fj Children:l Children: l FHI:l/k MSF Holand:f/ ! kj CARE: k Save the Children:f ! FHI:lf/k Oxfam GB: a Tselemt Save the Childrenf: j Addi Dessie Zuria: WVE: Arekay dlfk Tsegede ! Beyeda Concern:î l/ Mirab ! Concern:/ Welthungerhilfe:k Save the Children: Armacho f/k Debark Save the Children:fj Kelela: Welthungerhilfe: ! / Tach Abergele CRS: ak Save the Children:fj ! Armacho ! FHI: Save the l/k Save thef Dabat Janamora Legambo: Children:dfkj Children: ! Plan Int.:d/ j WVE: Concern: GOAL: Save the Children: dlfk Sahla k/ a / f ! ! Save the ! Lay Metema North Ziquala Children:fkj Armacho Wegera ACF: Save the Children: Tenta: ! k f Gonder ! Wag WVE: Plan Int.: / Concern: Save the dlfk Himra d k/ a WVE: ! Children: f Sekota GOAL: dlf Save the Children: Concern: Save the / ! Save: f/k Chilga ! a/ j East Children:f West ! Belesa FHI:l Save the Children:/ /k ! Gonder Belesa Dehana ! CRS: Welthungerhilfe:/ Dembia Zuria ! î Save thedf Gaz GOAL: Children: Quara ! / j CARE: WVE: Gibla ! l ! Save the Children: Welthungerhilfe: k d k/ Takusa dlfj k -

Benefit SBN 2019 Annual Report
Benefit SBN 2019 Annual Report 1 2 Contents 1.Sustainable agricultural production: Production cost price reduction 1 1.1. Sustainable agricultural production – Production cost price reduction 1 1.1.1. Yield and quality improvement 2 1.1.2. Harvest, transport and storage loss reduction 8 1.1.3. Improved farmers’ access to input credit 9 2. Product and market development 11 2.1. Post-harvest value creation 11 2.1.1 Store management 12 2.1.2.Cleaning and sorting 12 2.1.3. Exploring local oil extraction and quality standards 12 2.1.4. Product development for sesame and its rotational crops 13 2.2 Improved market linkages and sales 13 2.2.1. Cooperative spot market trade 13 2.2.2. Direct marketing unions and investors 14 2.2.3. Sourcing of processing companies 14 2.2.4. Marketing rotational crops 15 2.3. Improved access to marketing credit 15 2.3.1 Guarantee fund 15 3.Strengthened enabling environment for the Ethiopian sesame sector 17 3.1. Evidence-based information gathering and sharing 18 3.1.1. Stakeholder databases at woreda level (Excel and E-Prod) 18 3.1.2. Lessons learned, issue briefs and experience papers 18 3.1.3. Market information 19 3.1.4. Training and extension materials 19 3.2, Stakeholder capacity development 20 3.2.1. ARC staff training 20 3.2.2. Agronomic training 20 Table 2. No of farmers participated in GAP at woreda and kebele levels 21 Table 3 No of development agents trained at woreda and zone level 21 3.2.3. -

Transhumance Cattle Production System in North Gondar, Amhara Region, Ethiopia: Is It Sustainable?
WP14_Cover.pdf 2/12/2009 2:21:51 PM www.ipms-ethiopia.org Working Paper No. 14 Transhumance cattle production system in North Gondar, Amhara Region, Ethiopia: Is it sustainable? C M Y CM MY CY CMY K Transhumance cattle production system in North Gondar, Amhara Region, Ethiopia: Is it sustainable? Azage Tegegne,* Tesfaye Mengistie, Tesfaye Desalew, Worku Teka and Eshete Dejen Improving Productivity and Market Success (IPMS) of Ethiopian Farmers Project, International Livestock Research Institute (ILRI), Addis Ababa, Ethiopia * Corresponding author: [email protected] Authors’ affiliations Azage Tegegne, Improving Productivity and Market Success (IPMS) of Ethiopian Farmers Project, International Livestock Research Institute (ILRI), Addis Ababa, Ethiopia Tesfaye Mengistie, Bureau of Agriculture and Rural Development, Amhara Regional State, Ethiopia Tesfaye Desalew, Kutaber woreda Office of Agriculture and Rural Development, Kutaber, South Wello Zone, Amhara Regional State, Ethiopia Worku Teka, Research and Development Officer, Metema, Amhara Region, Improving Productivity and Market Success (IPMS) of Ethiopian Farmers Project, International Livestock Research Institute (ILRI), Addis Ababa, Ethiopia Eshete Dejen, Amhara Regional Agricultural Research Institute (ARARI), P.O. Box 527, Bahir Dar, Amhara Regional State, Ethiopia © 2009 ILRI (International Livestock Research Institute). All rights reserved. Parts of this publication may be reproduced for non-commercial use provided that such reproduction shall be subject to acknowledgement of ILRI as holder of copyright. Editing, design and layout—ILRI Publications Unit, Addis Ababa, Ethiopia. Correct citation: Azage Tegegne, Tesfaye Mengistie, Tesfaye Desalew, Worku Teka and Eshete Dejen. 2009. Transhumance cattle production system in North Gondar, Amhara Region, Ethiopia: Is it sustainable? IPMS (Improving Productivity and Market Success) of Ethiopian Farmers Project. -

Ethiopia Round 6 SDP Questionnaire
Ethiopia Round 6 SDP Questionnaire Always 001a. Your name: [NAME] Is this your name? ◯ Yes ◯ No 001b. Enter your name below. 001a = 0 Please record your name 002a = 0 Day: 002b. Record the correct date and time. Month: Year: ◯ TIGRAY ◯ AFAR ◯ AMHARA ◯ OROMIYA ◯ SOMALIE BENISHANGUL GUMZ 003a. Region ◯ ◯ S.N.N.P ◯ GAMBELA ◯ HARARI ◯ ADDIS ABABA ◯ DIRE DAWA filter_list=${this_country} ◯ NORTH WEST TIGRAY ◯ CENTRAL TIGRAY ◯ EASTERN TIGRAY ◯ SOUTHERN TIGRAY ◯ WESTERN TIGRAY ◯ MEKELE TOWN SPECIAL ◯ ZONE 1 ◯ ZONE 2 ◯ ZONE 3 ZONE 5 003b. Zone ◯ ◯ NORTH GONDAR ◯ SOUTH GONDAR ◯ NORTH WELLO ◯ SOUTH WELLO ◯ NORTH SHEWA ◯ EAST GOJAM ◯ WEST GOJAM ◯ WAG HIMRA ◯ AWI ◯ OROMIYA 1 ◯ BAHIR DAR SPECIAL ◯ WEST WELLEGA ◯ EAST WELLEGA ◯ ILU ABA BORA ◯ JIMMA ◯ WEST SHEWA ◯ NORTH SHEWA ◯ EAST SHEWA ◯ ARSI ◯ WEST HARARGE ◯ EAST HARARGE ◯ BALE ◯ SOUTH WEST SHEWA ◯ GUJI ◯ ADAMA SPECIAL ◯ WEST ARSI ◯ KELEM WELLEGA ◯ HORO GUDRU WELLEGA ◯ Shinile ◯ Jijiga ◯ Liben ◯ METEKEL ◯ ASOSA ◯ PAWE SPECIAL ◯ GURAGE ◯ HADIYA ◯ KEMBATA TIBARO ◯ SIDAMA ◯ GEDEO ◯ WOLAYITA ◯ SOUTH OMO ◯ SHEKA ◯ KEFA ◯ GAMO GOFA ◯ BENCH MAJI ◯ AMARO SPECIAL ◯ DAWURO ◯ SILTIE ◯ ALABA SPECIAL ◯ HAWASSA CITY ADMINISTRATION ◯ AGNEWAK ◯ MEJENGER ◯ HARARI ◯ AKAKI KALITY ◯ NEFAS SILK-LAFTO ◯ KOLFE KERANIYO 2 ◯ GULELE ◯ LIDETA ◯ KIRKOS-SUB CITY ◯ ARADA ◯ ADDIS KETEMA ◯ YEKA ◯ BOLE ◯ DIRE DAWA filter_list=${level1} ◯ TAHTAY ADIYABO ◯ MEDEBAY ZANA ◯ TSELEMTI ◯ SHIRE ENIDASILASE/TOWN/ ◯ AHIFEROM ◯ ADWA ◯ TAHTAY MAYCHEW ◯ NADER ADET ◯ DEGUA TEMBEN ◯ ABIYI ADI/TOWN/ ◯ ADWA/TOWN/ ◯ AXUM/TOWN/ ◯ SAESI TSADAMBA ◯ KLITE -

Spatial Modeling, Prediction and Seasonal Variation of Malaria in Northwest Ethiopia Asefa Adimasu Taddese, Adhanom Gebreegziabher Baraki* and Kassahun Alemu Gelaye
Taddese et al. BMC Res Notes (2019) 12:273 https://doi.org/10.1186/s13104-019-4305-1 BMC Research Notes RESEARCH NOTE Open Access Spatial modeling, prediction and seasonal variation of malaria in northwest Ethiopia Asefa Adimasu Taddese, Adhanom Gebreegziabher Baraki* and Kassahun Alemu Gelaye Abstract Objectives: The aim of this study was to determine the spatial modeling, seasonal variation of malaria and making prediction map of malaria in northwest Ethiopia. Results: The overall average cumulative annual malaria incidence during the study period was 30 per 100 popula- tions at risk. The highest proportion (29.2%) was observed from June 2015 to October 2016. In temporal analysis of clusters, the epidemic was observed from 2015/7/1 to 2016/12/31 throughout the study period in all districts. Hot- spot areas with high clusters (p < 0.001) were observed in Metema district it accounts 18.6% of the total malaria cases. An area of high median predicted incidence proportion (> 50%) was seen in the southwest part of the region. Most of the northern part of the study area was predicted to have a low median incidence proportion (< 10%). Keywords: Spatial analysis, Interpolation, Bayesian kriging, Clustering, Geostatistics modeling Introduction Malaria mosquitos are aggregated over large areas and Malaria is a mosquito-borne infectious disease of time periods. Tere are few studies examining the extent humans caused by the genus Plasmodium, which are and drivers of local variation in malaria exposure. introduced into the circulatory system by the bite of an In geographical location, close proximity share com- infected female anopheles mosquito [1]. -
2020 Annual Report P.O
Wageningen Centre for Development Innovation Wageningen Centre for Development Innovation supports value creation by Wageningen University & Research strengthening capacities for sustainable development. As the international expertise BENEFIT Partnership – 2020 Annual Report P.O. Box 88 and capacity building institute of Wageningen University & Research we bring 6700 AB Wageningen knowledge into action, with the aim to explore the potential of nature to improve The Netherlands the quality of life. With approximately 30 locations, 6,500 members (5,500 fte) of T +31 (0)317 48 68 00 staff and 12,500 students, Wageningen University & Research is a world leader in its www.wur.eu/cdi domain. An integral way of working, and cooperation between the exact sciences Bilateral Ethiopian-Netherlands Eff ort for Food, Income and Trade Partnership and the technological and social disciplines are key to its approach. Report WCDI-21-136 Dawit Alemu, Irene Koomen, Selome Kebede, Legesse Abate & Mirjam Schaap, Amsalu Ayana, Mohammed Hassena & Gareth Borman, Eyasu Elias & Eric Smaling, Helen Getaw & Monika Sopov, Geremew Terefe & Ted Schrader, Tewodros Tefera & Remko Vonk BENEFIT Partnership – 2020 Annual Report Bilateral Ethiopian-Netherlands Effort for Food, Income and Trade Partnership Dawit Alemu, Irene Koomen, Selome Kebede, Legesse Abate & Mirjam Schaap1 Amsalu Ayana, Mohammed Hassena & Gareth Borman2 Eyasu Elias & Eric Smaling3 Helen Getaw & Monika Sopov4 Geremew Terefe & Ted Schrader5 Tewodros Tefera & Remko Vonk6 1 PCU 2 ISSD 3 CASCAPE 4 ENTAG 5 SBN 6 REALISE Wageningen University & Research Wageningen / Addis Ababa, February 2021 Report WCDI-21-136 Dawit Alemu, Irene Koomen, Selome Kebede, Legesse Abate & Mirjam Schaap, Amsalu Ayana, Mohammed Hassena & Gareth Borman, Eyasu Elias & Eric Smaling, Helen Getaw & Monika Sopov, Geremew Terefe & Ted Schrader, Tewodros Tefera & Remko Vonk, 2021. -

Broad Bed Maker Technology Package Innovations in Ethiopian Farming Systems: an Ex Post Impact Assessment
ILRI International Livestock Research Institute Research Report 20 Broad bed maker technology package innovations in Ethiopian farming systems: An ex post impact assessment ISBN 92–9146–226–8 Broad bed maker technology package innovations in Ethiopian farming systems: An ex post impact assessment Arlene S Rutherford (PhD) ILRI International Livestock Research Institute INTERNATIONAL LIVESTOCK RESEARCH INSTITUTE i Author’s affiliation Arlene S Rutherford (PhD), Consultant to ILRI (International Livestock Research Institute), Nairobi, Kenya © 2008 ILRI (International Livestock Research Institute). All rights reserved. Parts of this publication may be reproduced for non-commercial use provided that such reproduction shall be subject to acknowledgement of ILRI as holder of copyright. Editing, design and layout—ILRI Publication Unit, Addis Ababa, Ethiopia. ISBN 92–9146–226–8 Correct citation: Rutherford AS. 2008. Broad bed maker technology package innovations in Ethiopian farming systems: An ex post impact assessment. Research Report 20. ILRI (International Livestock Research Institute), Nairobi, Kenya. 89 pp. ii Table of Contents List of Tables iv Acknowledgements v Executive summary vi 1 Introduction 1 2 Methodology 4 3 Results and discussion 6 3.1 National and regional impacts 6 3.2 The policy environment 9 3.3 Farmer survey results 16 3.4 Crop yields and prices with and without the BBM TP: Gross margins (GM) 27 3.5 Welfare with and without the BBM TP: Economic surplus (ES) 28 4 Conclusions and recommendations 31 References 32 Annex 1 Drawings