Motor Subtypes of Delirium
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Nursing Service Guidelines FALL PREVENTION MULTIDISCIPLINARY FALL PREVENTION
Nursing Service Guidelines FALL PREVENTION Title: MULTIDISCIPLINARY FALL PREVENTION Responsibility: Multidisciplinary staff need to take an active role in fall prevention. Equipment: Fall identification wrist bands, fall identification materials, and fall prevention equipment. Purpose: Since research has identified that numerous intrinsic and extrinsic variables can contribute to a patient’s risk of falling during a hospitalization, it is essential to determine the risk factors that place the patient at the greatest (highest) risk. By utilizing strategies that take into consideration the fall risk assessment score, clinical judgement, medication management, the patients mental status, and the patients ability to ambulate, it is intended that this approach will help prevent patient falls. The purpose of this guideline is to provide multidisciplinary staff with fall risk assessment tools that can be used to assist them in properly identifying those patients at risk for falling and determining interventions. General Information: A fall is defined as any unplanned descent to the floor, with or without injury (National Database of Nursing Quality Indicators [NDNQI], 2015). A fall may be either unassisted or assisted (where someone helps to ‘break’ the fall by helping the patient to the floor) and the NDNQI definition also includes falls where a patient lands on a surface where you would not expect to find the patient. University of Toledo Medical Center’s (UTMCs) fall injury level categories: • None • Minor (dressing, ice, cleaning, or elevation) • Moderate (suturing, splinting, or steri-strips/skin glue) • Major* (surgery, casting, traction, or neuro consult) • Death* (died as a result of injuries sustained from the fall) *if a patient’s fall has a major injury level or results in a death, the department manager or house supervisor and Quality Management need to be notified immediately. -

State of Florida Division of Administrative Hearings
STATE OF FLORIDA DIVISION OF ADMINISTRATIVE HEARINGS AGENCY FOR HEALTH CARE ) ADMINISTRATION, ) ) Petitioner, ) ) vs. ) Case Nos. 09-5360 ) 09-5363 GULF COAST MEDICAL CENTER, ) 09-5364 LEE MEMORIAL HEALTH SYSTEM, ) 09-5365 ) Respondent. ) ) RECOMMENDED ORDER Pursuant to notice to all parties, a final hearing was conducted in this case on January 25 through 29, 2010, in Fort Myers, Florida, before Administrative Law Judge R. Bruce McKibben of the Division of Administrative Hearings. The parties were represented as set forth below. APPEARANCES For Petitioner: Andrea M. Lang, Esquire Agency for Health Care Administration 2295 Victoria Avenue, Room 346C Fort Myers, Florida 33901 For Respondent: W. David Watkins, Esquire Watkins & Associates, P.A. Post Office Box 15828 Tallahassee, Florida 32317-5828 STATEMENT OF THE ISSUES The issues in this case are set forth in 11 separate counts within the four consolidated cases: Case No. 09-5360 Count I--Whether Respondent failed to properly monitor and care for a patient in restraints. Count II--Whether Respondent failed to ensure the physician's plan of care for patient was implemented. Case No. 09-5363 Count I--Whether Respondent failed to properly implement the physician's plan of care for patient. Case No. 09-5364 Count I--Whether Respondent failed to ensure a patients' right to privacy. Count II--Whether Respondent failed to ensure that food was served in the prescribed safe temperature zone. Count III--Whether Respondent failed to ensure that only authorized personnel had access to locked areas where medications were stored. Count IV--Whether Respondent failed to perform proper nursing assessments of a patient. -

Florida State Hospital State of Florida Operating Procedure Department of No
FLORIDA STATE HOSPITAL STATE OF FLORIDA OPERATING PROCEDURE DEPARTMENT OF NO. 150-14 CHILDREN AND FAMILIES CHATTAHOOCHEE, April 26, 2017 Health MEDICAL RESTRAINTS & SAFETY DEVICES 1. Purpose: This operating procedure prescribes the use of medical restraints and safety devices at Florida State Hospital. It establishes guidelines and methods to be employed by Hospital staff in restraining residents when the need is of a medical nature. 2. Scope: This procedure applies to all units at Florida State Hospital which use medical restraints. 3. References: a. Florida Statutes, Chapter 394 b. Florida Administrative Code 59A-3, Hospital Licensure c. Restraint Proper Environment OBRA Restraint Guidelines d. State Operations Manual, Appendix A, Survey Protocol, Regulations and Interpretive Guidelines for Hospitals, e. Centers for Medicare & Medicaid Services, HHS. §482.13 Conditions of Participation: Patient’s Rights 4. Philosophy of Florida State Hospital: Medical restraints of residents are methods of last resort and shall not be used unless lesser restrictive methods of intervention have been attempted and determined to be ineffective. Residents will be fully evaluated for restraint elimination and/or reduction at the time of each recovery team review (monthly, bi-monthly, 6-months and annual) and at the time of the 180-day review. Medical restraints shall be applied/ utilized in a manner that is most comfortable to the resident while preserving his/her dignity. Medical Restraints and safety devices shall NOT: a. impair neurovascular integrity; b. impair respiration; c. be tied to bedrails or moving parts of a gerichair or wheelchair; d. prevent residents from eating comfortably; e. interfere with toilet needs; This Operating Procedure supersedes: Operating Procedure 150-14 dated April 21, 2016 OFFICE OF PRIMARY RESPONSIBILITY: Medical Services DISTRIBUTION: See Training Requirements Matrix April26,2017 FSHOP150-14 f. -
Slides and Handouts
Organizing Clinical Information Systems to Manage and Improve Care Jennifer Allan, BSN, RN Methodist Healthcare System Jane Englebright, PhD, RN Columbia/HCA Healthcare Corporation Our Documentation System 1994 to 1996 • Four sites using a computerized clinical documentation system – Two using NANDA format – Two using NIC format • One site on paper Unresolved Problems Included: • Increased charting time, increased cost • Ambiguous, complex care plans • Hundreds of documentation screens • Physician dissatisfaction with nursing • Physician dissatisfaction with medical record • Fragmented, duplicative and conflicting information in the medical record “Fix” the System or De-install! • Meet legal, regulatory & clinical requirements • Decrease documentation time • Reduce costs • Eliminate repetition • Streamline record • Automate reports • Introduce interdisciplinary documentation • Lay foundation for quality monitoring • IMPROVE PATIENT CARE Two Early Rewrites Used Established Nursing Taxonomies Advantages Disadvantages NANDA Well known to Foreign to non- nurses nurses Non-exclusive diagnoses NIC Facilitates Long look-up for charging and interventions acuity Does not tie to care plan Review of Literature • NIC (Nursing Intervention Classification) • NANDA (North American Nursing Diagnosis Association) • Charting by Exception • Focus Charting • Problem Oriented (SOAP) • Practice Guidelines No current methodologies supported our vision: Concepts from NANDA, Our NIC, Charting by Goals Exception, Systems Theory Patient Centered Documentation © -
The Lethal Consequences of Restraint
EQUIP FOR EQUALITY A SPECIAL REPORT from the Abuse Investigation Unit NATIONAL REVIEW OF RESTRAINT RELATED DEATHS OF CHILDREN AND ADULTS WITH DISABILITIES: The Lethal Consequences of Restraint UIP FO Q R E E TM Q Y U A L I T UIP FO Q R E E TM Q Y U A L I T Mission Established in 1985, the mission of Equip for Equality is to advance the human and civil rights of people with disabilities in Illinois. Equip for Equality is a private not- for-profit legal advocacy organization designated by the governor to operate the federally mandated Protection and Advocacy System (P&A) to safeguard the rights of people with physical and mental disabilities, including developmental disabilities and mental illness. Equip for Equality is the only comprehensive statewide advocacy organization for people with disabilities and their families. All individuals with a disability in Illinois (as defined by the ADA) are eligible for services, including children, senior citizens, and individuals in state-operated facilities, nursing homes, and community-based programs. Services, Programs, and Projects Abuse Investigation Unit works to prevent abuse, neglect, and deaths of children and adults with disabilities in community-based programs, nursing homes, and state institutions. The Unit works with public investigatory agencies to improve their performance and coordination with each other; conducts investigations of abuse and neglect cases; alerts service providers to dangerous conditions and practices. Public Policy Advocacy achieves changes in state legislation, public policies and programs to safeguard individual rights and personal safety, enhance choice and self- determination, and promote independence, productivity, and community integration. -

Respondent's Brief, Wanda Williams V. CMO Management, LLC, No. 15-0553
No. 15-0553 IN THE SUPREME COURT OF APPEALS OF WEST V;.IR:..:::G~IN:...:..I:::....A:-__-::::::---:~ At Charleston ~OlS@ij WANDA WILLIAMS, INDIVIDUALLY AND ON BEHALF OF THE ESTATE AND WRONGFUL DEA H C~:~~r 2nZ~5,:~:J\ BENEFICIARIES OF ROBERT THOMPSON, Petitioner/Plaintiff Below, v. CMO MANAGEMENT, LLC (AS TO NICHOLAS COUNTY NURSING & REHABILITATION) Respondent/Defendant Below. Appeal from the Circuit Court of Nicholas County Honorable Gary L. Johnson, Judge Civil Action No. 13-C-92 BRIEF OF RESPONDENT/DEFENDANT BELOW CMO MANAGEMENT, LLC Jeffrey M. Wakefield, Esquire (W.va. Bar No. 3894) Mark A. Robinson, Esquire (W. Va. Bar No. 5954) Ryan A. Brown, Esquire (W. Va. Bar No.1 0025) FLAHERTY SENSABAUGH BONASSO PLLC P. O. Box 3843 Charleston, WV 25338-3843 Telephone: (304) 345-0200 Facsimile: (304) 345-0260 [email protected] [email protected] [email protected] Counsel for CMO Management, LLC TABLE OF CONTENTS TABLE OF AUTHORITIES ............................................................................................ii, iii STATEMENT OF THE CASE ...........................................................................................1 SUMMARY OF ARGUMENT ............................................................................................5 STATEMENT REGARDING ORAL ARGUMENT AND DECISION .................................8 ARGUMENT........................................................................................................................8 I. THE CIRCUIT COURT DID NOT ERR IN APPLYING THE MPLA'S -

Ethical Issues in Patient Restraint
Keywords: Restraint/Ethics/Mental Nursing Practice health/Dementia/Stroke care Discussion ●This article has been double-blind Restraint peer reviewed How to use the “four-quadrant” approach to analyse different restraint situations Ethical issues in patient restraint These comments suggest how chal- In this article... lenging the issues are; the head of patient The use of restraint in nursing practice safety at the National Patient Safety The four-quadrant approach to analysing ethical dilemmas Agency acknowledges that there are situa- tions when nurses have to intervene to Using this model to analyse different restraint situations prevent harm to a patient (Healey, 2010). However, according to Healey, vests, as well as belt and cuff devices are unaccept- Author Ann Gallagher is a reader in nursing by restraint by describing a “posey vest”. able and have resulted in deaths and ethics, director of the International Centre This fits over a patient’s clothing and has a serious harm. for Nursing Ethics, University of Surrey, and zip at the back and cloth ties at either side. As well as an ethical imperative to pre- editor of Nursing Ethics. Arms and legs can move freely, and the vent unjustifiable restraint, there is also a Abstract Gallagher A (2011) Ethical issues waist ties are attached to a bed or chair to legal framework that includes: Offences in patient restraint. Nursing Times; 107: prevent the patient from getting up. Against the Person Act 1961; the Mental 9, 18-20. Ms Morgan concluded: “I would rather Capacity Act 2005; Adults with Incapacity This article examines the ethical issues that have a conversation with a patient or their (Scotland) Act 2000; Human Rights Act arise in relation to restraint in mental health, family about why a posey vest is a good 1998; and the Mental Health Act 1983 (see dementia care and stroke care. -

The Inpatient Fall: Not Just an Incident Report
Inpatient Times January 2005 The Inpatient Fall: Not just an Incident Report By: Erica Bernstein, MD, MPH, Geriatrics Section You have doubtless received the RN call stating that Mr. Nameless fell while escaping from his posey vest, and that -you need to examine him and fill out the incident report. Importantly, the workup for the fall does not end here. Falls are a symptom, not a diagnosis. Understanding why someone fell is the first step to prevention. Falls are common in the elderly: • 1/3 of community dwelling elders fall yearly • 50% of nursing home elderly fall yearly • Falls account for 89% of inpatient incident reports • Rate of falls in inpatient elders: 1.5 falls per bed annually • 50% of inpatient fallers fall repeatedly Falls increase the length of hospital stay. Elders who have fallen once are 3-20 times more likely to require a skilled nursing facility admission. Fifty percent of elders hospitalized for a fall will be dead within one year. Falls occur when environmental demands exceed a person’s ability to compensate. Therefore, both intrinsic and extrinsic risk factors need to be addressed. Interventions can occur as early as the admission assessment by identifying high-risk patients. Risk factors for falls include: • age 65 yrs or older • past falls history • cognitive impairment (i.e. dementia, delirium) • urinary/fecal incontinence • balance problems, lower extremity weakness, arthritis • psychotropic drug use • ETOH PT/OT evaluation of all high-risk patients on admission allows early identification of modifiable risks, gait retraining, or balance training. Review medication lists to remove unnecessary medications or choose less dangerous alternatives. -

Petitioner's Brief, Wanda Williams V. CMO Management, LLC, No. 15-0553
.. IN THE SUPREME COURT OF APPEALS OF WEST VIR NO. 15-0553 o 11 ~ ~II,! SEP 1 4 2015 ~ Wanda Williams, Individually and on behalf RORY L PERRY n, CLERK I of the Estate and Wrongful Death Beneficiaries SUPREME COURT OF APPEALS , of Robert Thompson, ,-__=OF-",W=ES..;,..;TV..;.;.;IR=G!~ ____ PETITIONER I PLAINTIFF BELOW v. On Appeal from Nicholas County Civil Action No. 13-C-92 CMO Management, LLC; (as to Nicholas County Nursing & Rehabilitation) Defendant Below RESPONDENT I DEFENDANT BELOW PETITIONER'S BRIEF McHUGH FULLER LAW GROUP, PLLC James B. McHugh, WV BarNo. 10350 [email protected] Michael J. Fuller, Jr., WV Bar No. 101501 [email protected] D. Bryant Chaffm, WV Bar No. 11069 [email protected] Amy J. Quezon, WV BarNo. 11036 [email protected] A. Lance Reins, WV Bar No. 11548 [email protected] 97 Elias Whiddon Rd. Hattiesburg, MS 39402 Phone: 601-261-2220 Facsimile: 601-261-2481 Counselfor Petitioner / Plaintiff 1 Counsel of Record pursuant to W. Va. R. App. P. 3(a). TABLE OF CONTENTS Table of Contents..............................................................................................i Table ofAuthorities.........................................................................................iii Cases..................................................................................................iii Statutes and Other Authorities...................................................................iv Assignments of Error........................................................................................1 -
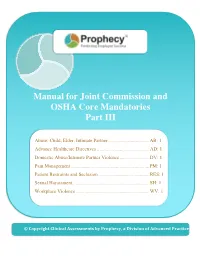
Manual for Joint Commission and OSHA Core Mandatories Part III
Manual for Joint Commission and OSHA Core Mandatories Part III Abuse: Child, Elder, Intimate Partner ................................. AB: 1 Advance Healthcare Directives .......................................... AD: 1 Domestic Abuse/Intimate Partner Violence ........................ DV: 1 Pain Management ............................................................... PM: 1 Patient Restraints and Seclusion ......................................... RES: 1 Sexual Harassment ............................................................. SH: 1 Workplace Violence ........................................................... WV: 1 © Copyright Clinical Assessments by Prophecy, a Division of Advanced Practice Strategies © Copyright Clinical Assessments by Prophecy, a Division of Advanced Practice Strategies AB: 1 Abuse: Child, Elder, Intimate Partner INTRODUCTION Three types of abuse that may be seen in the healthcare setting are child abuse, elder abuse, and intimate partner violence, also known as domestic violence. The abuse of one person by another can take many forms – physical, emotional, psychological, sexual, and more. The statistics regarding abuse are disturbing: In 2014, more than 700,000 children were abused and/or neglected in the U.S. In 2015, more than 2.1 million cases of elder abuse were reported in the U.S. On average, nearly 20 people per minute are physically abused by an intimate partner in the U.S. Many victims end up seeking medical care at hospitals, physician offices, and clinics. Healthcare providers are likely to encounter victims of abuse from time to time, and they can play a critical role in recognizing, reporting, and helping victims of abuse. PURPOSE/OVERALL GOAL This module outlines what providers need to know about child abuse, elder abuse, and intimate partner violence. It explains the types of abuse that can be experienced by each, how to recognize the signs, and what providers should do if abuse is suspected. -

Federal Register/Vol. 64, No. 127/Friday, July 2, 1999/Rules and Regulations
36070 Federal Register / Vol. 64, No. 127 / Friday, July 2, 1999 / Rules and Regulations DEPARTMENT OF HEALTH AND medical and surgical care) and (f) assess compliance with the CoPs. The HUMAN SERVICES (Standard: Seclusion and restraint for SAs conduct these surveys using the behavior management) will be State Operations Manual (SOM) (HCFA Health Care Financing Administration considered if we receive them at the Publication No. 7). The SOM contains appropriate address as provided in the the regulatory language of the CoPs as 42 CFR Part 482 ADDRESSES section, no later than 5 p.m. well as interpretive guidelines and [HCFA±3018±IFC] on August 31, 1999. We will not survey probes that elaborate on consider comments on provisions of the regulatory intent and give in-depth RIN 0938±AJ56 regulation that remain unchanged from detail about how to maintain compliance. The SOM also outlines the Medicare and Medicaid Programs; the December 19, 1997 proposed rule or survey process and provides guidance Hospital Conditions of Participation: on provisions that were changed based for State administration of the survey Patients' Rights on our consideration of public comments. program. Under § 489.10(d), the SAs AGENCY: Health Care Financing ADDRESSES: Mail comments (an original determine whether hospitals meet the Administration (HCFA), HHS. and three copies) to the following CoPs and make corresponding recommendations to us about the ACTION: Interim final rule with address: Health Care Financing comment. Administration, Department of Health hospital's certification, (that is, whether and Human Services, Attention: HCFA± the hospital has met the standards SUMMARY: This rule introduces a new 3018±IFC, P.O. -

Hearing Before the Special Committee on Aging United States Senate One Hundred Fourth Congress First Session
S. HRG. 104-384 MEDICAID REFORM: QUALITY OF... CARE IN NURSING HOMES AT RISK HEARING BEFORE THE SPECIAL COMMITTEE ON AGING UNITED STATES SENATE ONE HUNDRED FOURTH CONGRESS FIRST SESSION WASHINGTON, DC OCTOBER 26, 1995 Serial No. 104-7 Printed for the use of the Special Committee on Aging U.S. GOVERNMENT PRINTING OFFICE 21-092 CC WASHINGTON: 1996 For sale by the U.S. Government Priming Office Superintendent of Documents, Congressional Sales Office, Waslington, DC 20402 ISBN 0-16-052450-4 SPECIAL COMMITTEE ON AGING WILLIAM S. COHEN, Maine, Chairman LARRY PRESSLER, South Dakota DAVID PRYOR, Arkansas CHARLES E. GRASSLEY, Iowa JOHN GLENN, Ohio ALAN K. SIMPSON, Wyoming BILL BRADLEY, New Jersey JAMES M. JEFFORDS, Vermont J. BENNETT JOHNSTON, Louisiana * LARRY CRAIG, Idaho JOHN B. BREAUX, Louisiana CONRAD BURNS, Montana HARRY REID, Nevada RICHARD SHELBY, Alabama HERB KOHL, Wisconsin RICK SANTORUM, Pennsylvania RUSSELL D. FEINGOLD, Wisconsin FRED THOMPSON, Tennessee CAROL MOSELEY-BRAUN, Illinois MARY BERRY GERWIN, Staff Director/Chief Counsel THERESA M. FoRSTER, Minority Staff Director (11) CONTENTS Page Opening statement of Senator William S. Cohen .............................. ................... 1 Statement of: Senator David Pryor ............................................................ 6 Senator Conrad Burns ................. ........................................... 8 Senator Russ Feingold ................. ........................................... 10 Senator Harry Reid ............. ..............................................