Intravenous Alfaxalone Anaesthesia in Two Squamate Species: Eublepharis Macularius and Morelia Spilota Cheynei
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

268 Part 522—Implantation Or Injectable Dosage Form
§ 520.2645 21 CFR Ch. I (4–1–18 Edition) (ii) Indications for use. For the control 522.82 Aminopropazine. of American foulbrood (Paenibacillus 522.84 Beta-aminopropionitrile. larvae). 522.88 Amoxicillin. 522.90 Ampicillin injectable dosage forms. (iii) Limitations. The drug should be 522.90a Ampicillin trihydrate suspension. fed early in the spring or fall and con- 522.90b Ampicillin trihydrate powder for in- sumed by the bees before the main jection. honey flow begins, to avoid contamina- 522.90c Ampicillin sodium. tion of production honey. Complete 522.144 Arsenamide. treatments at least 4 weeks before 522.147 Atipamezole. main honey flow. 522.150 Azaperone. 522.161 Betamethasone. [40 FR 13838, Mar. 27, 1975, as amended at 50 522.163 Betamethasone dipropionate and FR 49841, Dec. 5, 1985; 59 FR 14365, Mar. 28, betamethasone sodium phosphate aque- 1994; 62 FR 39443, July 23, 1997; 68 FR 24879, ous suspension. May 9, 2003; 70 FR 69439, Nov. 16, 2005; 73 FR 522.167 Betamethasone sodium phosphate 76946, Dec. 18, 2008; 75 FR 76259, Dec. 8, 2010; and betamethasone acetate. 76 FR 59024, Sept. 23, 2011; 77 FR 29217, May 522.204 Boldenone. 17, 2012; 79 FR 37620, July 2, 2014; 79 FR 53136, 522.224 Bupivacaine. Sept. 8, 2014; 79 FR 64116, Oct. 28, 2014; 80 FR 522.230 Buprenorphine. 34278, June 16, 2015; 81 FR 48702, July 26, 2016] 522.234 Butamisole. 522.246 Butorphanol. § 520.2645 Tylvalosin. 522.275 N-Butylscopolammonium. 522.300 Carfentanil. (a) Specifications. Granules containing 522.304 Carprofen. 62.5 percent tylvalosin (w/w) as 522.311 Cefovecin. -

The Laryngeal Mask Airway: Potential Applications in Neonates
F485 Arch Dis Child Fetal Neonatal Ed: first published as 10.1136/adc.2003.038430 on 21 October 2004. Downloaded from PERSONAL PRACTICE The laryngeal mask airway: potential applications in neonates D Trevisanuto, M Micaglio, P Ferrarese, V Zanardo ............................................................................................................................... Arch Dis Child Fetal Neonatal Ed 2004;89:F485–F489. doi: 10.1136/adc.2003.038430 The laryngeal mask airway is a safe and reliable airway 2.5–5 kg.11 It has been postulated that a smaller size (0.5) could be useful in preterm management device. This review describes the insertion newborns. However, there are reports of techniques, advantages, limitations, and potential successful use of size 1 in preterm neonates applications of the laryngeal mask airway in neonates. weighing 0.8–1.5 kg.12–15 ........................................................................... (2) Fully deflate the cuff as described in the manual, and lubricate the back of the mask tip (for neonates in the labour ward, he ability to maintain a patent airway and lubrication may not be necessary, as oral provide effective positive pressure ventilation and pharyngeal secretions may reproduce T(PPV) is the main objective of neonatal this function). resuscitation and all anaesthesiological proce- (3) Press (flatten) the tip of the LMA against the dures.1–6 This is currently achieved with the use hard palate. During this manoeuvre, the of a face mask or an endotracheal tube. Both of these devices have major limitations from a operator should grasp the LMA like a pen strictly anatomical point of view and require with the index finger at the junction adequate operator skills. In certain situations, between the mask and the distal end of the both face mask ventilation and tracheal intuba- airway tube. -
Exploring Our Frogs (Years 7–8)
Exploring our frogs (Years 7–8) Lesson plan Victorian Curriculum F–101 links: Introduction Science Investigating the frogs of your local area provides a great context for developing student Levels 7 and 8 understanding about biological classification, Science Understanding ecosystem processes and the impact that humans have on the natural environment. It is Science as a Human Endeavour also a great way to encourage students to Science and technology contribute to finding explore, develop their observational skills and to solutions to a range of contemporary issues; enjoy the natural world around them. these solutions may impact on other areas of society and involve ethical considerations These activities use digital applications such as (VCSSU090) Melbourne Water’s Frog Census and the Atlas Biological sciences of Living Australia (ALA) to develop students’ ICT skills. There are differences within and between groups of organisms; classification helps The Frog Census app is a powerful citizen organise this diversity (VCSSU091) science tool that enables students, their families and the wider community to improve our Interactions between organisms can be understanding of the biology and distribution of described in terms of food chains and food webs and can be affected by human activity frog species in Melbourne; information that will (VCSSU093) help to develop effective policy and management strategies to conserve and Digital technologies enhance these populations. Data and information Activity 1: Finding our frogs Analyse and visualise data using a range of software to create information, and use Students explore local frogs using the Atlas of structured data to model objects or events Living Australia and learn about how frogs are (VCDTDI038) named and classified by biologists. -

Effects of Alfaxalone Or Propofol on Giant-Breed Dog Neonates Viability
animals Article Effects of Alfaxalone or Propofol on Giant-Breed Dog Neonates Viability During Elective Caesarean Sections Monica Melandri 1, Salvatore Alonge 1,* , Tanja Peric 2, Barbara Bolis 3 and Maria C Veronesi 3 1 Società Veterinaria “Il Melograno” Srl, 21018 Sesto Calende, Varese, Italy; [email protected] 2 Department of Agricultural, Food, Environmental and Animal Sciences, University of Udine, 33100 Udine, Italy; [email protected] 3 Department of Veterinary Medicine, Università degli Studi di Milano, 20100 Milan, Italy; [email protected] (B.B.); [email protected] (M.C.V.) * Correspondence: [email protected]; Tel.: +39-392-805-8524 Received: 20 September 2019; Accepted: 7 November 2019; Published: 13 November 2019 Simple Summary: Nowadays, thanks to the increased awareness of owners and breeders and to the most recent techniques available to veterinarians, the management of parturition, especially of C-sections, has become a topic of greater importance. Anesthesia is crucial and must be targeted to both the mother and neonates. The present study aimed to evaluate the effect of the induction agent alfaxalone on the vitality of puppies born from elective C-section, in comparison to propofol. After inducing general anesthesia for elective C-section, puppies from the mothers induced with alfaxalone had higher 5-min Apgar scores than those induced with propofol. The concentration of cortisol in fetal fluids collected at birth is neither influenced by the anesthetic protocol used, nor does it differ between amniotic and allantoic fluids. Nevertheless, the cortisol concentration in fetal fluids affects the relationship between anesthesia and the Apgar score: the present study highlights a significant relationship between the anesthetic protocol used and Apgar score in puppies, and fetal fluids cortisol concentration acts as a covariate of this relationship. -

The Cardiorespiratory and Anesthetic Effects of Clinical and Supraclinical
THE CARDIORESPIRATORY AND ANESTHETIC EFFECTS OF CLINICAL AND SUPRA CLINICAL DOSES OF ALF AXALONE IN CYCLODEXTRAN IN CATS AND DOGS DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of The Ohio State University By Laura L. Nelson, B.S., D.V.M. * * * * * The Ohio State University 2007 Dissertation Committee: Professor Jonathan Dyce, Adviser Professor William W. Muir III Professor Shane Bateman If I have seen further, it is by standing on the shoulders of giants. lmac Ne1vton (1642-1727) Copyright by Laura L. Nelson 2007 11 ABSTRACT The anesthetic properties of steroid hormones were first identified in 1941, leading to the development of neurosteroids as clinical anesthetics. CT-1341 was developed in the early 1970’s, featuring a combination of two neurosteroids (alfaxalone and alphadolone) solubilized in Cremophor EL®, a polyethylated castor oil derivative that allows hydrophobic compounds to be carried in aqueous solution as micelles. Though also possessing anesthetic properties, alphadolone was included principally to improve the solubility of alfaxalone. CT-1341, marketed as Althesin® and Saffan®, was characterized by smooth anesthetic induction and recovery in many species, a wide therapeutic range, and no cumulative effects with repeated administration. Its cardiorespiratory effects in humans and cats were generally mild. However, it induced severe hypersensitivity reactions in dogs, with similar reactions occasionally occurring in cats and humans. The hypersensitivity reactions associated with this formulation were linked to Cremophor EL®, leading to the discontinuation of Althesin® and some other Cremophor®-containing anesthetics. More recently, alternate vehicles for hydrophobic drugs have been developed, including cyclodextrins. -

Frogs & Reptiles NE Vic 2018 Online
Reptiles and Frogs of North East Victoria An Identication and Conservation Guide Victorian Conservation Status (DELWP Advisory List) cr critically endangered en endangered Reptiles & Frogs vu vulnerable nt near threatened dd data deficient L Listed under the Flora and Fauna Guarantee Act (FFG, 1988) Size: of North East Victoria Lizards, Dragons & Skinks: Snout-vent length (cm) Snakes, Goannas: Total length (cm) An Identification and Conservation Guide Lowland Copperhead Highland Copperhead Carpet Python Gray's Blind Snake Nobbi Dragon Bearded Dragon Ragged Snake-eyed Skink Large Striped Skink Frogs: Snout-vent length male - M (mm) Snout-vent length female - F (mm) Austrelaps superbus 170 (NC) Austrelaps ramsayi 115 (PR) Morelia spilota metcalfei – en L 240 (DM) Ramphotyphlops nigrescens 38 (PR) Diporiphora nobbi 8.4 (PR) Pogona barbata – vu 25 (DM) Cryptoblepharus pannosus Snout-Vent 3.5 (DM) Ctenotus robustus Snout-Vent 12 (DM) Guide to symbols Venomous Lifeform F Fossorial (burrows underground) T Terrestrial Reptiles & Frogs SA Semi Arboreal R Rock-dwelling Habitat Type Alpine Bog Montane Forests Alpine Grassland/Woodland Lowland Grassland/Woodland White-lipped Snake Tiger Snake Woodland Blind Snake Olive Legless Lizard Mountain Dragon Marbled Gecko Copper-tailed Skink Alpine She-oak Skink Drysdalia coronoides 40 (PR) Notechis scutatus 200 (NC) Ramphotyphlops proximus – nt 50 (DM) Delma inornata 13 (DM) Rankinia diemensis Snout-Vent 7.5 (NC) Christinus marmoratus Snout-Vent 7 (PR) Ctenotus taeniolatus Snout-Vent 8 (DM) Cyclodomorphus praealtus -

Tracheal Intubation
//Tracheal Intubation http://www.expertconsultbook.com/expertconsult/b/book.do?m... Tracheal Intubation Technique As previously discussed, because of differences in anatomy, there are differences in techniques for intubating the trachea of infants and children compared with adults.[1–4,17–19,99,114,115] Because of the smaller dimensions of the pediatric airway there is increased risk of obstruction with trauma to the airway structures. A technique to be avoided is that in which the blade is advanced into the esophagus and then laryngeal visualization is achieved during withdrawal of the blade. This maneuver may result in laryngeal trauma when the tip of the blade scrapes the arytenoids and aryepiglottic folds. There are several approaches to exposing the glottis in infants with a Miller blade. One philosophy consists of advancing the laryngoscope blade under constant vision along the surface of the tongue, placing the tip of the blade directly in the vallecula and then using this location to pivot or rotate the blade to the right to sweep the tongue to the left and adequately lift the tongue to expose the glottic opening. This avoids trauma to the arytenoid cartilages. One can thus lift the base of the tongue, which in turn lifts the epiglottis, exposing the glottic opening. If this technique is unsuccessful, one may then directly lift the epiglottis with the tip of the blade (see Video Clip 12-1, Coming Soon). Another approach is to insert the Miller blade into the mouth at the right commissure over the lateral bicuspids/incisors (paraglossal approach). The blade is advanced down the right gutter of the mouth aiming the blade tip toward the midline while sweeping the tongue to the left. -

Chicago Academy of Sciences, Vol. 7, No. 2
BULLETIN OF THE CHICAGO ACADEMY OF SCIENCES A SYNOPSIS OF THE AMERICAN FORMS OF AGKISTRODON (COPPERHEADS AND MOCCASINS) BY HOWARD K. GLOYD Chicago Academy of Sciences AND ROGER CONANT Philadelphia Zoological Society CHICAGO Published by the Academy 1943 The Bulletin of the Chicago Academy of Sciences was initiated in 1883 and volumes 1 to 4 were published prior to June, 1913. During the following twenty-year period it was not issued. Volumes 1, 2, and 4 contain technical or semi-technical papers on various subjects in the natural sciences. Volume 3 contains museum reports, descriptions of museum exhibits, and announcements. Publication of the Bulletin was resumed in 1934 with volume 5 in the present format. It is now regarded as an outlet for short to moderate-sized original papers on natural history, in its broad sense, by members of the museum staff, members of the Academy, and for papers by other authors which are based in considerable part upon the collections of the Academy. It is edited by the Director of the Museum with the assistance of a committee from the Board of Scientific. Governors.. The separate numbers are issued at irregular intervals and distributed to libraries and scientific organizations, and to specialists with whom the Academy maintains exchanges. A reserve is set aside for future need as exchanges and the remainder of the edition offered for sale at a nominal price. When a suffi- cient number of pages have been printed to form a volume of convenient size, a title page, table of contents, and index are supplied to libraries and institutions which receive the entire series. -

240 Part 522—Implantation Or Injectable Dosage Form
§ 520.2645 21 CFR Ch. I (4–1–14 Edition) feed; and for the control of porcine pro- (3) Limitations. Federal law restricts liferative enteropathies (PPE, ileitis) this drug to use by or on the order of a associated with Lawsonia intracellularis licensed veterinarian. when followed immediately by tylosin [77 FR 55415, Sept. 10, 2012] phosphate medicated feed. (B) For the treatment and control of PART 522—IMPLANTATION OR swine dysentery associated with Brachyspira hyodysenteriae. INJECTABLE DOSAGE FORM NEW (iii) Limitations. Prepare a fresh solu- ANIMAL DRUGS tion daily. Do not administer within 48 Sec. hours of slaughter. As indicated in 522.23 Acepromazine. paragraph (d)(3)(ii)(A) of this section, 522.52 Alfaxalone. follow with tylosin phosphate medi- 522.56 Amikacin. cated feed as in § 558.625(f)(1)(vi)(c) of 522.62 Aminopentamide. this chapter. 522.82 Aminopropazine. (4) Honey bees—(i) Amount. Mix 200 522.84 Beta-aminopropionitrile. milligrams tylosin in 20 grams confec- 522.88 Amoxicillin. 522.90 Ampicillin injectable dosage forms. tioners’/powdered sugar. Use imme- 522.90a Ampicillin trihydrate suspension. diately. Apply (dust) this mixture over 522.90b Ampicillin trihydrate powder for in- the top bars of the brood chamber once jection. weekly for 3 weeks. 522.90c Ampicillin sodium. (ii) Indications for use. For the control 522.144 Arsenamide. of American foulbrood (Paenibacillus 522.147 Atipamezole. 522.150 Azaperone. larvae). 522.161 Betamethasone. (iii) Limitations. The drug should be 522.163 Betamethasone dipropionate and fed early in the spring or fall and con- betamethasone sodium phosphate aque- sumed by the bees before the main ous suspension. -

Anesthesia During Gestation and Its Effects on Newborn
Scientific Works. Series C. Veterinary Medicine. Vol. LXIII (1) ISSN 2065-1295; ISSN 2343-9394 (CD-ROM); ISSN 2067-3663 (Online); ISSN-L 2065-1295 increased cardiac work, and decreased an endotheliochorial and zonary type of peripheral vascular resistance. Other changes placenta (Miglino et al., 2006; Furukawa et al., ANESTHESIA DURING GESTATION AND ITS EFFECTS are respiratory, represented by decreased FRC, 2014). Most anesthetics cross the placenta and ON NEWBORN VIABILITY decreased total lung volume, increased minute the blood-brain barrier of the fetus. The ventilation and oxygen consumption, and permeability of the placenta differs depending Andra DEGAN, Dragoș BÎRȚOIU, Alexandru ȘONEA, Ruxandra COSTEA decreased PaCO2 (Ryan, Wagner, 2006; on type of placenta and the physicochemical Lemke, 2007; Branson, 2007). Dams and properties of the drugs. The endotheliochorial University of Agronomic Science and Veterinary Medicine, Faculty of Veterinary Medicine fetuses have an increased metabolic demand, placenta present in canines allows close Bucharest, 59 Marasti Blvd., District 1, Bucharest, Romania leading to a maternal blood volume increases maternal-fetal contact which facilitates the of approximately 40%. Plasma volume increase passive passage of drugs. Placental transfer of Corresponding author email: [email protected] is proportionally greater than the increase in drugs can occur by several mechanisms; by far, erythrocytes, leading to hemodilution and the most important is simple diffusion. Abstract: relative anemia (Seymour, 1999; Pascoe, Diffusion across the placenta is determined by During the gestation period, canine females go through physiological changes which can influence the way the Moon, 2001). A greater number of fetuses will molecular weight, the degree to which the drug anesthetics are absorbed, metabolized and excreted. -
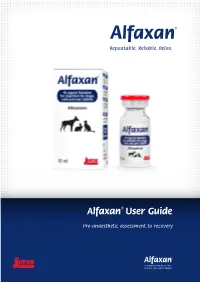
Alfaxan® User Guide
Repeatable. Reliable. Relax. Alfaxan® User Guide Pre-anaesthetic assessment to recovery PRE-ANAESTHETIC ASSESSMENT INDUCTION TRANSITION Full clinical examination Draw up the full dose of Alfaxan® Connect to appropriate breathing system 2 mg/kg (0.2 mL/kg) for dogs CHECK FOR... LOOK OUT Suitable for anaesthesia? 5 mg/kg (0.5mL/kg) for cats FOR... 4 mg/kg (0.4 mL/kg) for rabbits YES NO Label the syringe Spontaneous ventilation? Take a ‘pre-induction’ Assign ASA score Further tests? heart rate YES NO Stabilise ASA PHYSICAL STATUS Re-assess CLASSIFICATION SYSTEM (Consider referral?) Secure IV access Ensure catheter is The five physical risk states are: intravenous and patent Supply maintenance Wait. If SPO2 ASA Physical Status 1 A normal healthy patient • Early plane of sedation agent and / or clinical signs indicate the ASA Physical Status 2 A patient with mild systemic disease Give ¼ of the induction dose • Degree of control Breathing need, start IPPV ASA Physical Status 3 A patient with severe systemic disease over the animal (Likely to be continuous) ASA Physical Status 4 A patient with severe systemic disease that is WAIT 15 SECONDS Heart Rate a constant threat to life (Alfaxan® is thought to LOOK OUT FOR... ASA Physical Status 5 A moribund patient who is not expected to Give another ¼ dose minimally affect cardiac survive without the operation function at clinical doses) If the animal has been presented as an emergency, the letter ‘E’ can be added to the recorded stage. WAIT 15 SECONDS Anaesthetic Depth • Adequate duration of action for It is essential that all patients are classified before any premedication is applied, and that smooth & unhurried transition consideration is paid to the classification in developing the patient’s anaesthetic protocol. -

Conservation Advice for the Karst Springs and Associated Alkaline Fens of the Naracoorte Coastal Plain Bioregion
The Threatened Species Scientific Committee provided their advice to the Minister on 31 July 2020. The Minister approved this Conservation Advice on 3 December 2020 and agreed that no recovery plan is required at this time. Conservation Advice1 for the Karst springs and associated alkaline fens of the Naracoorte Coastal Plain Bioregion This document combines the approved conservation advice and listing assessment for the threatened ecological community. It provides a foundation for conservation action and further planning. Karst springs and alkaline fens, Ewen Ponds © Copyright, Anthony Hoffman Conservation Status The Karst springs and associated alkaline fens of the Naracoorte Coastal Bioregion is listed in the Endangered category of the threatened ecological communities list under the Environment Protection and Biodiversity Conservation Act 1999 (EPBC Act). The ecological community was assessed by the Threatened Species Scientific Committee, who found it to be eligible for listing as Endangered and recommended that a recovery plan is not required at this time. The Committee’s assessment and recommendations are at Section 6. The Committee’s assessment of the eligibility against each of the listing criteria is: Criterion 1: Vulnerable Criterion 2: Endangered Criterion 3: Insufficient data Criterion 4: Endangered Criterion 5: Insufficient data Criterion 6: Insufficient data The main factors that make the threatened ecological community eligible for listing in the Endangered category are its historic losses to drainage, clearing and resulting fragmentation, and ongoing threats to its integrity and function, particularly from hydrological changes. The Karst springs and associated alkaline fens of the Naracoorte Coastal Plain Bioregion occurs within country (the traditional lands) of the Boandik and the Gunditjmara peoples.