Trigger Point from Wikipedia, the Free Encyclopedia Jump To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

History of Tae Kwon Do.Pdf
Tae Kwon Do History Introduction: Although modern Taekwondo has actually only existed for about 50 years (the martial art known Tae Kwon Do was developed between 1945 and 1955 and only became known as Tae Kwon Do in 1955.), it is based upon Shotokan Karate, another 20th century martial art, and ancient Korea martial arts, such as Taekkyon and Subak, that have lost favor in modern times. Tae Kwon Do is a martial art that means "The Way of the Feet and Hands". Writings on Taekwondo history usually portray Taekwondo as an unique product of Korean culture, developed over the long course of Korean history since the Three Kingdoms Era. However, Taekwondo's primary influence came from Japanese Karate that was introduced into Korea during the Japanese occupation of Korea during the early 1900s. Few written records on ancient Korean history exist, so factual information on Korean martial arts is scarce and sketchy. Because of this, most Korean martial arts writers find something in Korean history to support their claims; writers on Tae Kwon Do included. If one researches the history of Tae Kwon Do, in the research they will find differing and sometimes contradictory information. Majority of this information is a summary taken from Reference 1. For more details, please review the entire material on history of Tae Kwon Do from Reference 1. Origins of Tae Kwon Do: Empty-hand fighting did not originate wholly in only one country, but it developed naturally in every place humans settled. In each country, people adapted their fighting techniques to deal with the dangers in their local environments. -

D2492609215cd311123628ab69
Acknowledgements Publisher AN Cheongsook, Chairperson of KOFIC 206-46, Cheongnyangni-dong, Dongdaemun-gu. Seoul, Korea (130-010) Editor in Chief Daniel D. H. PARK, Director of International Promotion Department Editors KIM YeonSoo, Hyun-chang JUNG English Translators KIM YeonSoo, Darcy PAQUET Collaborators HUH Kyoung, KANG Byeong-woon, Darcy PAQUET Contributing Writer MOON Seok Cover and Book Design Design KongKam Film image and still photographs are provided by directors, producers, production & sales companies, JIFF (Jeonju International Film Festival), GIFF (Gwangju International Film Festival) and KIFV (The Association of Korean Independent Film & Video). Korean Film Council (KOFIC), December 2005 Korean Cinema 2005 Contents Foreword 04 A Review of Korean Cinema in 2005 06 Korean Film Council 12 Feature Films 20 Fiction 22 Animation 218 Documentary 224 Feature / Middle Length 226 Short 248 Short Films 258 Fiction 260 Animation 320 Films in Production 356 Appendix 386 Statistics 388 Index of 2005 Films 402 Addresses 412 Foreword The year 2005 saw the continued solid and sound prosperity of Korean films, both in terms of the domestic and international arenas, as well as industrial and artistic aspects. As of November, the market share for Korean films in the domestic market stood at 55 percent, which indicates that the yearly market share of Korean films will be over 50 percent for the third year in a row. In the international arena as well, Korean films were invited to major international film festivals including Cannes, Berlin, Venice, Locarno, and San Sebastian and received a warm reception from critics and audiences. It is often said that the current prosperity of Korean cinema is due to the strong commitment and policies introduced by the KIM Dae-joong government in 1999 to promote Korean films. -

The Necessity to Know History. in 1945, Moo Duk Kwan Was Found in Order to Spread, Prosper and Create Understanding of Soo Bahk
The necessity to know history. In 1945, Moo Duk Kwan was found in order to spread, prosper and create understanding of Soo Bahk Do (now called Tang Soo Do), which is the special martial art of Korea, and has a long history and tradition. The foundation of Moo Duk Kwan has remained unshakable by the cooperation and efforts of all members and persons who are interested. The fame of Moo Duk Kwan has grown not only in Korea, but all over the world. Now, although technique is very important, theory has to be taught for the purpose of the increase of Tang Soo Do and the martial arts. First of all, therefore, all members must perfectly understand the foundation theory of rational history about the art. From time to time some members who have excellent skills deviate from the right path because they do not know and understand it's true history and the foundation. So it is very important to study history and the foundation theory. The theory of it's origin. The exact origin of Tang Soo Do, as well as karate in general, is obscure. However, there are many equally beautiful theories. An argument continues to rage about the origin of both weapon using and weaponless fighting techniques. Some Japanese karate experts insist that the art is of Japanese origin; some say it came from Okinawa; others say it began in China and spread from there. Although there are various theories and views explaining it's history in Korea, we will consider the Moo Duk Kwan's assertion as described in Moo Duk Kwan's major text book Soo Bahk Do Dae Kam, written by Grand Master Hwang Kee, president. -

Kwan's Name: “Bluewaves” Meaning a Youngster's Spirit and Vitality
The Development of the “Kwan’s” Kwan: in Korean literally means building or hall, but when used in martial arts it can also refer to a school or clan of martial artists who follow the same style and/or leader. At the time, there were 9 major Kwans throughout Korea and once someone joined a particular Kwan, it was very difficult to transfer to another Kwan. When someone wanted to transfer to another Kwan, his original Kwan Jang had to authorize and approve the transfer, but in reality, the Kwan Jang usually threatened the member using authoritative means in an effort to persuade the potential transferee to not leave. This was a critical issue in those days. Chung Do Kwan Established by Won Kuk Lee, seated in the middle and next led by Duk Sung Son, the back row, second from the right. After the independence of Korea, the Chung Do Kwan, one of the five key Dojangs, was founded first. It symbolized Chung Do Kwan's name: “Bluewaves” meaning a youngster's spirit and vitality. Chung Do Kwan's founder, LEE Won Kuk, moved to Japan when he was 19 years old in 1926. While in Japan, he first attended middle and high school, and then entered the Law School of Chuo University. Then he entered Japan's Karate headquarters, the Song Do Kwan (Shotokan). He received Karate instruction from Karate's father, Gichin Funakoshi. There, he learned Karate with Song Moo Kwan's founder, RO Byung Jick. Later, he moved back to Korea and taught Tang Soo Do in the Yong Shin school hall in Suh Dae Moon Gu's Ochun Dong, Seoul because he had a good relationship with Japan's Cho-sun Governor General Abe in 1944. -
Yu Gup Ja Training Manual
Independent Tang Soo Do Association YU GUP JA TRAINING MANUAL © Copyright South Hills Karate Academy (Gene Garbowsky) No part of this document may be reproduced, copied or distributed without express permission from Master Gene Garbowsky Published May, 2013 A Message from Sa Bom Nim Gene Garbowsky, Kwan Jang Nim, Independent Tang Soo Do Association As a member of the Independent Tang Soo Do Association, I hope that you will come to re- alize the benefits of training in Tang Soo Do. As you may know, I have been teaching this Martial Art to hundreds of students over the past 30 years. I truly believe that every man, women, and child can benefit in many ways from practicing Martial Arts and Tang Soo Do. What are Martial Arts? It is the name given to the traditional systems of self-defense that have been practiced in Eastern and Western societies for thousands of years. Masters of the ancient Martial Arts ultimately discovered that mastery of the body comes through mas- tery of the mind. Therefore, the practice of Martial Arts is a way to a more fulfilling life. It is a path to freedom from self-confinement and the ultimate goal to mental and physical har- mony. Martial Arts training can absolutely change a person physically, psychologically, and emo- tionally in a very positive way. Regular physi- cal activity energizes the body, and since martial arts are based on natural law, the body can quickly reach top conditioning. Once physical changes develop, they soon lead to the mental and emotional improve- ments that many seek through the martial arts. -
Bronce Til Fikret Filicki VM
ok t O b e r · 2 0 1 0 TAEKWONDO M e d l e M s b l a d f O r d a N s K t a e kwon d O f O r b u N d VM 2009 I dette nummer · VM 2009 - det bedste hidtil · bronce til fikret filicki VM - en organisatorisk succes · VM - de frivilliges sejr · dansk teakwondo forbund vokser familien sveder sammen · børn lokker forældre til kamptræning jKytu dang vinder 8. eM titel · Koreansk kampsports historie Taekwondo · ok T o b e r 2 0 1 0 af Murad ahmed, 5. dan, Team olederendense · redaktør Vi starter med en undskyldning kære Taekwondovenner, så er vi her endelig med et en lIlle bøn nyt blad. Vi er kede af, at det har taget så lang tid at bladet er som sagt skrevet færdigt for længe siden, og få bladet lagt ud på taekwondo.dk, og fra forbundets jeg beder jer derfor om, at I læser bladet med nogle side vil jeg gerne starte med en undskyldning. ”februar 2010 briller” for, at I ikke tænker, at vi med bladet var sådan set allerede skrevet færdig i februar i vilje bringer ”gamle” nyheder. Trods alt har en del af år, men på grund af omstruktureringer i forbundets in- jer sendt artikler og stof ind til bladet, og det fortjener formationsstrategi havnede bladet i en sprække, hvor at blive læst. og selvom det ikke længere er aktuelt det har ligget indtil nu. og hvad betyder det så: syntes jeg alligevel i blandt andet skal læse artiklen Samtidig med, at bladet ikke længere udkommer i fra VM og glæde jer over, at vi I danmark afholdt det papirform har man fra forbundets side haft stor fokus bedste VM nogensinde! på at lancere www.taekwondo.dk som informations- portal som alle har kunnet benytte sig af. -

2015 United States Martial Arts Hall of Fame Inductees KARMINA
2015 United States Martial Arts Hall of Fame Inductees YOUTH KARMINA BEDIONES…………………………………………………………………………BLACKBELT OF THE YEAR Karmina holds the rank of Black Belt in Traditional Kung Fu. She is also certified in Liu He Bafa. She has studied Northern and Southern Kung Fu, Tai Chi and Chen Style Tai Chi. She is an avid competitor and has won 8 North American Titles and numerous AKA Grand Champions. She is an active Instructor at China Tai Chi Kung Fu under Sifu Wes Letioa. ISAAC CLARK …………………………………………………………………………………….BLACKBELT OF THE YEAR Isaac holds a Black Belt in Tae Kwon Do under Master Scott Rutter. He has trained in the Martial Arts for 5 years and has received the All Star Triple Crown. JORDAN CLARK……………………………………….…………………………………………BLACKBELT OF THE YEAR Jordan holds the rank of Black Belt in Tae Kwon Do under Master James Goodwin. At the age of 16 he is an active Instructor at the new 4 Mile Hill Tae Kwon Do School in Judsonia Arkansas under the guidance of Mr. Goodwin. Jordan possesses quality leadership abilities and is an outstanding Black Belt role model for all students. RYAN CROSBY…………………………………..……………………………………………….BLACKBELT OF THE YEAR Ryan holds a 3rd Degree Black Belt in Shorinji Kempo Karate under Master Amy Hawkins. He has also studied Kempo Jujitsu. He is a member of the Martial Arts Training International and International Shorinji Kempo Karate Federation. He has received 2 Leadership Awards, Assistant Instructor Award. SIERRA GORSKI………………………………………………….………………………………BLACKBELT OF THE YEAR Sierra was born on August 9th, 1998 in Buffalo New York. At the age of 9 she began to study Tae Kwon Do under Grandmaster Eric Von Brandt at Brandt’s Martial Arts Program. -

Historique Hapkido
Hap Ki Do: art martial coréen. Le HapKiDo est un art martial coréen. Il signifie "la voie de la coordination et de la puissance Interne". Il comprend une grande variété de techniques dynamiques : Clés, immobilisations, projections, balayages, percussions pieds poings, chutes. Les 2 principales figures coréennes qui ont contribué au développement du HapKiDo sont Me Choi Yong Sul (1904 - 1986) souvent considéré comme le fondateur du HapKiDo et Me Ji Han Jae, élève du 1er, mais qui a apporté sa propre contribution en intégrant nombre de techniques de percussion de pieds. Me Ji est souvent considéré comme le "père" du HapKiDo Moderne, même si le fondateur Choi Yong Sul avait d'autres élèves directs qui ont suivi des voies parallèles à Me Ji et qui lui contestent certaines de ses affirmations. Les origines. Me Choi Yong Sul Il est acquis que les techniques de clés et projections du HapKiDo sont largement influencées par l'art martial japonais : Daito-Ryu Aiki-Jutsu. Le fondateur Choi Yong Sul a pratiqué le Daito-Ryu Aiki-Jutsu pendant son séjour au Japon avec un maître de cette discipline : Sokaku Takeda. Les liens exacts (Maître/disciple ou Maître/serviteur) entre les 2 hommes varient selon les versions. Il était cependant reconnu une grande proximité technique sur une longue période qui a servi Choi Yong Sul. Quand on connaît les relations difficiles entre les peuples Japonais et Coréens, on peut comprendre l'extraordinaire chemin parcouru par le jeune orphelin Choi, qui a grandi au Japon sous le nom d'emprunt japonais de Tatujutu Yoshida et qui a réussi à gagner la confiance d'un grand maître d'arts martiaux japonais pendant presque 30 ans. -

Terminology.Pdf
Copyright 2008 Yang’s Kuk Sul Do Federation® General Terminology General Names and Titles Korean Word English Translation Kuk Ki National Flag Kwon Ki Association Flag Chong Jae Nym Grandmaster Chong Kwan Jang Nym Chief master Kwan Jang Nym Fifth degree black belt Boo Kwan Jang Nym Fourth degree black belt Sa Bum Nym Third degree black belt Kyo Sa Nym Second degree black belt Jo Kyo Nym First degree black belt Yoo Dahn Jah Black belt holder Jae Jah Martial arts student Dahn Boh Black-brown belt Ja Di Brown belt Hohng Di Red belt Chuhng Di Blue belt Noh Rahng Di Yellow belt Hin Di White belt More General Terms Korean Word English Translation Di Belt Doh Bohk Martial arts uniform Eue Bohk Clothing Jah Seh Stance – posture Ki Hahp Martial arts yell Eum Yahng Yin & Yang Yoo Won Hwa Flow Circle Harmony Buhb Principle or law Maek Pressure point Soo Technique Hyung Form Kyuhk Pah Breaking Ahn Inside Ahp Front Yuhp Side Dwee Back Jwah Left (Direction) When Left Woo Right (Direction) Wron Right Juhng Straight Ssahng Double Yuhk Reverse - 1 - Copyright 2008 Yang’s Kuk Sul Do Federation® Sahng High Joong Middle Hah Low Ki Bohn Fundamental – basic Ki Cho Foundation – basic Cho Geup Elementary level Joong Geup Middle level Goh Geup High level Dae Geup Advanced level Commands and Stances Korean English Juhng Jwah Kneel Kyung Neh Salute / Bow Kuk Ki Ae Dae (Hah Yuh) Kyung Neh Salute to the National Flag Kwon Ki Ae Dae Hah Kyung Neh Salute to the Association Flag Chong Jea Nym Kae Kyung Neh Salute to Grandmaster Soo Ryuhn Practice Shi Jahk Begin Soo Ryuhn -
Unificação Dos Kwans Grão-Mestre Sylvio Cruz
Seminário de TaeKwondo Chang Moo Kwan Tradicional Parte 2 – Unificação dos Kwans Grão-Mestre Sylvio Cruz Julho 2017 8º Dan WTCF As 5 Kwans Principais • 1944 – Chung Do Kwan • Fundador: Won Kuk Lee – Karatê Shotokan (aluno de Gichin Funakoshi) • 1945 - Song Moo Kwan • Fundador: Ro Byung Jick - Karatê Shotokan (aluno de Gichin Funakoshi) • 1945 - Moo Duk Kwan • Fundador: Hwang Kee – Estudou Tai’chi, Tekkyon e Kung-Fu • Sentindo a dificuldade dos coreanos em aprender artes chinesas adotou as formas do Kong Soo Do em seu currículo • 1946 – Chang Moo Kwan (YMCA Kwon Bop Club) • Fundandor: Yoon, Byung-In – Karatê Shudokan (aluno de Kanken Tōyama) • 1946 – Ji Do Kwan (Chosun Yun Mu Kwan Kong Soo Do Club) • Fundador: Chun Sang Sup - Karatê Shotokan (aluno de Gichin Funakoshi) • Era tão amigo de Yoon Byung-In que os dois eram considerados irmãos Primeiras tentativas de unificação • Era preciso padronizar os exames e Oficializar as graduações de Dan • De 1947 a 1950 várias reuniões aconteceram sem resultado • 1952 Korean Tang Soo Do Association (KTA) • Moo Duk Kwan • Maio 25, 1953 - Korean Kong Soo Do Association (KKA), • Chung Do Kwan • Ji Do Kwan • Song Moo Kwan • Chang Moo Kwan Famosa Demonstração de 1954 • Nam, Tae-Hi realiza uma série de quebramentos e impression o Presidente • Presidente Syngman Rhee questiona que arte marcial era aquela e se era Tekkyion... • Kong Soo Do? • Tang Soo Do? • Hwa Soo Do? • Soo Bak Do? • Tae Soo Do? • Presidente Syngman Rhee ordena que todas as unidades militares recebam treinamento • Gen. Choi funda a Oh Do Kwan • Braço Militar da Chung Do Kwan • Convoca Nam, Tae-Hi para ser seu braço direito • Inicia a criação dos hyungs Comitê para nomeação da arte (1955) • Local: Kisaeng House (Casa de Gueixas) • Organizador: Gen. -

History-TKD and Hapkido-Scott Shaw
The History of the Korean Martial Arts By Scott Shaw Copyright 1979, 1982, 1987, 2001 - All Rights Reserved Ancient Korea and the Foundations for the Korean Martial Arts Korea is a predominantly mountainous peninsula, 320 kilometers (200 miles) wide by 965 kilometers (600 miles) in length. It extends Southward from the Chinese mainland. The East Sea, also known as the Sea of Japan, borders Korea to the East and the Yellow Sea frames it to the West. Only twenty percent of the Korean Peninsula is lowland suitable for cultivation and mass settlement. The remaining eighty percent is too rugged for agriculture. Due to these geographic factors, the majority of the Korean population is concentrated along inland valleys and coastal plains which open up to its Western Coast. Koreans are an ethnically homogeneous Mongoloid people. The Korean Peninsula was first inhabited by Tungusic tribes from central Asia in about 3000 B.C.E. These people had a Paleolithic culture, using stones as tools and followed a shamanistic religion. The legendary figure Tan'gun is said to have formed the first Korean Kingdom in 2333 B.C.E. The Tungusic tribes spoke a Ural-Altaic language. This language group extends from Scandinavia and the Balkans in the West, through Central, North, and Northwest Asia in the East. Though dialects of the Ural-Altaic languages vary greatly, they each share similar characteristics of syntax (the way in which words are put together). This language group set the foundation for the modern Korean language. Korea is bounded to the North by China. The Chinese language comes from the Sino-Tibetan language group. -
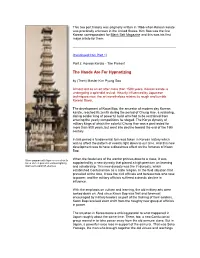
History of Korean Karate Part 2
This two part history was originally written in 1966 when Korean karate was practically unknown in the United States. Kim Soo was the first Korean correspondent for Black Belt Magazine and this was his first major article for them. (Continued from Part 1) Part 2: Korean Karate - The Present The Hands Are For Hypnotizing by (Then) Master Kim Pyung Soo Almost lost as an art after more than 1500 years, Korean karate is undergoing a splendid revival. Heavily influenced by Japanese techniques now, the art nonetheless retains its rough and tumble Korean flavor. The development of Kwon Bop, the ancestor of modern day Korean karate, reached its zenith during the period of Chung Hae, a roistering, daring soldier king of powerful build who had to be restrained from entering the yearly competitions he staged. The Koryo dynasty of military kings of which the colorful Chung Hae was a part lasted for more than 500 years, but went into decline toward the end of the 15th century. In this period a fundamental turn was taken in Korean history which was to affect the pattern of events right down to our time. And this new development was to have a disastrous effect on the fortunes of Kwon Bop. Stone pagoda with figures carved on its When the feudal era of the warrior princes drew to a close, it was faces of men posed in various fighting supplanted by a new dynasty that placed a high premium on learning stances to ward off enemies. and scholarship. This new dynasty was the Yi dynasty, which established Confucianism as a state religion.