Coverage Assessment (SLEAC Report)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PDMC Laghman Meeting Minutes
Laghman Provincial Disaster Management Committee (PDMC) Meeting Minutes Provincial Governor’s Office – Wednesday, 04 March, 2015 Participants: WFP, UNICEF, WHO, NCRO, SERVE, IRC, NRC, MADERA, SCA, IOM, DRC, ARCS, OCHA, ANDMA, ANA, ANP, DRRD, DoPH, DoRR, DoEnvironment, DoEducation, DoPW, DoAIL, Governor’s Office and other government officials. A. Introduction and Opening Remarks of Provincial Governor: On Wednesday 04 October 15, the Provincial Governor (PG) for Laghman called a Provincial Disaster Management Committee meeting (PDMC). After a short round of introductions, the PG welcomed PDMC members, further he extend of condolences with families, lost their family members due to recent rainfall, snowfall/avalanches and flood particularly to the people of Laghman province and he also highlighted on recent natural hazards (Rainfall, Flood and Snowfall) occurred on 25 February, 2015. The PG gratitude from humanitarian community’s efforts for there on timely response to the affected families he also appreciated the ANSAF’s on time action in rescued the people in Mehterlam and Qarghayi districts of Laghman province, especially ANA rescued 90 Nomad people Marooned in Qarghayi district of Laghman. The PG also highlighted on devastation caused by rainfall and flood which lifted 5 killed, 13 injured, about more than 500 families affected, 800 Jirebs or 400 Acores Agriculture land/Crops washed away and about 39 irrigation canal and intakes severely damaged or destroyed. The PG calcified devastations in three categories to facilitate the response for both (Humanitarian Community and Government line departments). 1. Response to Emergency need and saves lives. 2. Mid-terms actions as reactivation of irrigation system (cleaning of intakes and irrigation canal) opening the routs. -

Afghanistan: Annual Report 2014
AFGHANISTAN ANNUAL REPORT 2014 PROTECTION OF CIVILIANS IN ARMED CONFLICT © 2014/Ihsanullah Mahjoor/Associated Press United Nations Assistance Mission United Nations Office of the High in Afghanistan Commissioner for Human Rights Kabul, Afghanistan February 2015 Kabul, Afghanistan July 2014 Source: UNAMA GIS January 2012 AFGHANISTAN ANNUAL REPORT 2014 PROTECTION OF CIVILIANS IN ARMED CONFLICT United Nations Assistance Mission United Nations Office of the High in Afghanistan Commissioner for Human Rights Kabul, Afghanistan February 2015 Photo on Front Cover © 2014/Ihsanullah Mahjoor/Associated Press. Bodies of civilians killed in a suicide attack on 23 November 2014 in Yahyakhail district, Paktika province that caused 138 civilian casualties (53 killed including 21 children and 85 injured including 26 children). Photo taken on 24 November 2014. "The conflict took an extreme toll on civilians in 2014. Mortars, IEDs, gunfire and other explosives destroyed human life, stole limbs and ruined lives at unprecedented levels. The thousands of Afghan children, women and men killed and injured in 2014 attest to failures to protect civilians from harm. All parties must uphold the values they claim to defend and make protecting civilians their first priority.” Nicholas Haysom, United Nations Special Representative of the Secretary-General in Afghanistan, December 2014, Kabul “This annual report shows once again the unacceptable price that the conflict is exacting on the civilian population in Afghanistan. Documenting these trends should not be regarded -
An Annotated Bibliography of Nuristan (Kafiristan) and the Kalash Kafirs of Chitral Part One
Historisk-filosofiske Meddelelser udgivet af Det Kongelige Danske Videnskabernes Selskab Bind 41, nr. 3 Hist. Filos. Medd. Dan. Vid. Selsk. 41, no. 3 (1966) AN ANNOTATED BIBLIOGRAPHY OF NURISTAN (KAFIRISTAN) AND THE KALASH KAFIRS OF CHITRAL PART ONE SCHUYLER JONES With a Map by Lennart Edelberg København 1966 Kommissionær: Munksgaard X Det Kongelige Danske Videnskabernes Selskab udgiver følgende publikationsrækker: The Royal Danish Academy of Sciences and Letters issues the following series of publications: Bibliographical Abbreviation. Oversigt over Selskabets Virksomhed (8°) Overs. Dan. Vid. Selsk. (Annual in Danish) Historisk-filosofiske Meddelelser (8°) Hist. Filos. Medd. Dan. Vid. Selsk. Historisk-filosofiske Skrifter (4°) Hist. Filos. Skr. Dan. Vid. Selsk. (History, Philology, Philosophy, Archeology, Art History) Matematisk-fysiske Meddelelser (8°) Mat. Fys. Medd. Dan. Vid. Selsk. Matematisk-fysiske Skrifter (4°) Mat. Fys. Skr. Dan. Vid. Selsk. (Mathematics, Physics, Chemistry, Astronomy, Geology) Biologiske Meddelelser (8°) Biol. Medd. Dan. Vid. Selsk. Biologiske Skrifter (4°) Biol. Skr. Dan. Vid. Selsk. (Botany, Zoology, General Biology) Selskabets sekretariat og postadresse: Dantes Plads 5, København V. The address of the secretariate of the Academy is: Det Kongelige Danske Videnskabernes Selskab, Dantes Plads 5, Köbenhavn V, Denmark. Selskabets kommissionær: Munksgaard’s Forlag, Prags Boulevard 47, København S. The publications are sold by the agent of the Academy: Munksgaard, Publishers, 47 Prags Boulevard, Köbenhavn S, Denmark. HISTORI SK-FILOSO FISKE MEDDELELSER UDGIVET AF DET KGL. DANSKE VIDENSKABERNES SELSKAB BIND 41 KØBENHAVN KOMMISSIONÆR: MUNKSGAARD 1965—66 INDHOLD Side 1. H jelholt, H olger: British Mediation in the Danish-German Conflict 1848-1850. Part One. From the MarCh Revolution to the November Government. -

3A7b666d3616ccc5492576df
DISEASES EARLY WARNING SYSTEM th February 22, 2010 WEEKLY MORBIDITY & MORTALITY REPORT 4 Year , Issue –07 Flu Updates: The following Activities have been done Epid Week 07, 2010 HIGHLIGHTS - So far we have 953 confirmed cases of AH1N1 in the country. ¾ Out of 182 Sentinel sites, 182 sentinel sites have sent their -The total number of deaths reported till now is 17. reports in Week-07 of 2010; 22 treatment sites activated in Kabul province and all provincial and regional ¾ Out of total 169,766 events recorded in week-07 of 2010, hospitals have facilities for treatment and sample collection, the tamiflu and PPEs distributed to all provinces. 53,311(31.4%) consultations were reported due to DEWS target diseases. The positive cases reported from the below provinces: Kabul,Balkh,Hirat,Kandahar,Nangarhar,Bamyan,Hilmand,Takhar, ¾ Main causes of consultations this week are ARI (26.5%) and Panjsher,Baghlan,,Ghazni,Parwan,Kundoz,Badakhshan,Faryab,Ghor, ADD (3.9%) from total clients in a continuing trend from Badghis,Jawzjan,Nooristan,Konar, Daikundi, Samangan the week before. - CCC (command and control center) is functional ¾ 80 death cases caused due to Pneumonia, Meningitis/SIC - Three telephone hotlines are open to help people, 0798644004 and Diarrheal diseases, so that 67 cases due to 0798665085 – 0798660829 - Intensive surveillance to detect A H1N1 in the country is functional; daily pneumonia/ARI, 1 death cases due to diarrheal diseases and 12 deaths cases reported due to Meningitis and Severely reports are allocated, compiled and shared with all stakeholders. - 177 sentinel sites are functional in the country and reporting on the Ill Children. -

Eric Newby Worked Briefly in Advertising Before Joininga Finnish Four-Masted Bark in 1938, an Experience He Described in the Last Grain Race
PENGUIN BOOKS A SHORT WALK IN THE HINDU RUSH Born in London in 1919 and educated at St. Paul's School, Eric Newby worked briefly in advertising before joininga Finnish four-masted bark in 1938, an experience he described in The Last Grain Race. In 1942 he was captured off Sicily while trying to rejoin the submarine from which he had landed to attack a German airfield. When the Snow Comes, They Will Take You Away describes how he escaped with the aid of the woman he subsequently married. For nine years or so he worked in the wholesale fashion business, "tottering up the back stairs of stores with armfuls of stock" (of which he wrote in Something Wholesale), and in a Mayfair couture house. Then he left to explore wildest Nuristan, an expedition hilariously chronicled in A Short Walk in the Hindu Kush. In 1963—after some years as fashion buyer to a chai n of department stores-—together with his wife, Wanda, he made a 1,200-mile descent of the Ganges, described in Slowly down the Ganges. On his return he became travel editor of the Observer. Other books by Eric Newby include Love and War in the Apennines, The World Atlas of Exploration, and Great Ascents. His most recent book, The Big Red Train Ride, an account of his journey from Moscow to the Pacific on the Trans-Siberian Railway, is also published by Penguin Books. He and his wife now live in Devonshire when not traveling abroad. ERIC NEWBY A Short Walk in the Hindu Kush Preface by Evelyn Waugh PENGUIN BOOKS Penguin Books Ltd, Harmondsworth, Middlesex, England Penguin Books, 625 Madison Avenue, New York, New York 10022, U.S.A. -

Selected Papers Hindukush Cultural Conference Moesgard 1970
BEITRAGE ZUR SODASIENFORSCHUNG SODASIEN - INSTITUT UNIVERSITAT HEIDELBERG BAND 1 FRANZ STEINER VERLAG . WIESBADEN 1974 ISBN 3-515-01217-6 Alle Rechte vorbehalten Ohne ausdriickliche Genehmigung des Verlages ist es auch nicht gestattet, das Werk oder einzelne Teile daraus nachzudrucken oder auf photomechanischem Wege (Photoko~ie,Mikrokopie usw.) zu ~ervielfalti~en @ 19 74 by Franz Steiner Verlag GmbH, Wiesbaden Satz und Druck: Druckerei Wolf, Heppenheim Printed in Germany This photo may symbolize the Conferenee: From right to left Professor Georg Morgenstierne, Oslo, President of the Conferenee, Ahmad Ali Motamedi, Director General of the Antiquitie~ of Afghbt~I- stan, Ahmad Yusuf Nuristani fro~~NisheigFom,student of the Umiversi- ty of Kabul, ~ittfngmound a the elentss o2€ 9 reaaam4mzok- iom af r WaFg~aliiArmem im %he pa Mws,vlse; (Pkmh~P~sban '&3.re$rug ram 9, CONTENTS Page INTRODUCTION (K.Jettmar) .................................... IX I. LINGUISTIC INTRODUCTION G.Morgenstierne: Languages of Nuristan and Surrounding Regions ...................................... 1 11. CONTRIBUTIONS TO THE HISTORY OF NURISTAN K.Kristiansen: A Kafir on KAfir History and Festivals .................................... 11 R.F.Strand: Native Accounts of Kom History ............ 22 Wazir Ali Shah: Invasions Preceding the Conquest of Nuristan ..................................... 24 111. CONTRIBUTIONS TO THE PROBLEM OF THE PRE-MUSLIM RELIGION OF NURISTAN Shahzada Hussam-ul-Mulk: The Cosmology of the Red Kafirs ....................................... 26 G.Buddruss: Some Reflections on a Kafir Myth .......... 31 W.Lentz: Western Parallels to the Deeds of Imra ....... 37 K.Jettmar: Iranian Influence on the Cultures of the Hindukush .................................... 39 IV. CONTRIBUTIONS TO A SOCIOLOGY OF NURISTAN S.Jones: Kalashum Political Organisation .............. 44 R.F.Strand: Principles of Kinship Organisation among the Kom Nuristani ............................... -

Annual Report 2014
DACAAR Annual Report 2014 Cover photo: Senior staff members cutting the cake at DACAAR’s 30th anniversary ceremony, Kabul, August 28, 2014 CONTENTS ABOUT DACAAR 1 BASIC FACTS 1 MISSION, VISION AND VALUES 2 DIRECTOR’S INTRODUCTION 3 DACAAR’S APPROACH AND AREAS OF INTERVENTION 4 DACAAR’S BENEFICIARIES 5 DACAAR’S COMMUNITY BASED APPROACH 5 CROSS-CUTTING ISSUES AND OTHER STRATEGIC PRIORITIES 5 DACAAR’S CONTRIBUTION TO NATIONAL PLANS 6 OVERALL ACHIEVEMENTS DURING 2014 6 DACAAR’S ACTIVITIES IN AFGHANISTAN 7 WATER, SANITATION AND HYGIENE (WASH) 9 NATURAL RESOURCES MANAGEMENT (NRM) 13 SMALL SCALE ENTERPRISE DEVELOPMENT (SSED) 15 WOMEN’S EMPOWERMENT (WE) 17 NATIONAL SOLIDARITY PROGRAMME (NSP) 19 ORGANISATIONAL DEVELOPMENT 21 USE OF FUNDS 22 THE FUTURE 23 Access full PDF downloads from www.dacaar.org/resources/annual-report Copyright © 2015 | All rights reserved. Reproduction: Contents of this publication may be reproduced with prior permission. 1 | DACAAR | Annual Report 2014 ABOUT DACAAR DACAAR is a non-political, non-governmental, non-profit development/humanitarian organisation that has been working to improve the lives of the Afghan people since 1984. DACAAR works in rural and peri-urban areas and aims at improving livelihoods through sustainable activities that engage Afghan communities to be agents of their own development process. DACAAR employs a holistic approach to all its rural development activities in order to ensure long-term sustainability of projects. While the bulk of DACAAR’s programming is development focused, the organisation continues to maintain a strong humanitarian presence in order to respond to the various humanitarian needs across its geographical areas of intervention. -

Anthropometric Nutrition Survey and IYCF Study-Laghman Province
Anthropometric nutrition survey Children from 6 to 59 months Pregnant - Lactating women And Infant and Young Child Feeding Practices study Children from 0 to 23 months Final Report Mihtarlam and Qarghayi districts Laghman province, Afghanistan From the 22 nd to the 28 th of May 2011 Funded by UNICEF Islamic Republic of Afghanistan 1 Anthropometric nutrition survey and Infant and Young Child Feeding Study Mihtarlam and Qarghayi districts - Laghman province – May 2011 - Afghanistan ACKNOWLEDGEMENT With funding from UNICEF, this anthropometric nutrition survey and Infant and Young Child Feeding study could be undertaken in Mihtarlam and Qarghayi districts, Laghman province. The coordinator of this project was Ms Brigitte Tonon, ACF Health - Nutrition Coordinator highly supported by M. Tariq Khan, ACF Nutrition Program Manager. This work would not have been possible without the dedicated efforts of the nutrition community and the local population in Afghanistan. These partners included: • The Ministry of Public Health and particularly the Public Nutrition Department, for their collaboration in this project; • The Nutrition Cluster body for their support; • The community representatives of the surveyed villages who have supported the nutrition survey teams during the data field collection; • The community members in the surveyed villages for welcoming and supporting the nutrition survey teams during the field work ; • The numerous Non Governmental Organizations and United Nations agencies for sharing information on the general situation in -
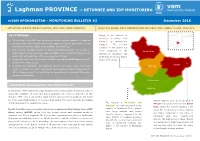
Laghman PROVINCE — RETURNEE and IDP MONITORING Mvam AFGHANISTAN - MONITORING BULLETIN #2 December 2016
Laghman PROVINCE — RETURNEE AND IDP MONITORING mVAM AFGHANISTAN - MONITORING BULLETIN #2 December 2016 SITUATION UPDATE ON RETURNEES, IDPS AND FOOD MARKETS ANALYSIS BASED ON A COMBINATION OF FIELD AND PHONE (mVAM) SURVEYS KEY FINDINGS Supply to the markets of Alishang is mainly from The majority of the IDPs and returnees in all the assessed districts of Laghman traders in Mehterlam province access their food through credit, reliance on friends and family or from markets. The security humanitarian assistance. Only a few purchase food with cash. conditions in this district are Both returnees and IDPs in all the 5 districts of Laghman province are relying on Daulat Shah worse compared to the Daulat Shah casual labour to generate income, but availability is very limited (1-2 days/week) situation in Qarghayi and particularly during this time of the year (post harvest time). Mehterlam and better than in The priority needs for both returnees and IDPs were Food and Shelter particularly Daulat Shah district. in light of the winter season. Alingar In Mehterlam, Qarghayi and Alishang districts, the traders and households Alishang reported relying on credit to buy stocks from suppliers/retailers. Compared to 2015, reliance on credit for traders has decreased in Mehterlam and Alishang but increased in Qarghayi. Asad Abad Mehterlam (province ASSESSMENT BACKGROUND AND METHODOLOGY center) Qarghayi In September, WFP conducted a rapid market survey in Nangarhar Province in order to assess the suitability of using cash-based assistance for returnees and IDPs. In late October, WFP carried out another rapid market survey in Kunar, Laghman and Kabul provinces where high numbers of returnees had settled. -

The Beautiful and Scenic Surrounding Valleys Are the Natural Attractions of This Province
1st Edition, 1st October 2006 Introductory Edition Contents LAGHMAN INTRODUCTION Laghman province is one of the thirty-four provinces of Afghanistan. It is in the east Alingar , Alishing of the country and Its capital is Mehtar Lam. 2 Laghman is an evergreen region on the northern banks of the Kabul river which run Dawlat shah , Mehterlam parallel to the Kabul-Jalalabad-Peshawar highway. 3 The town is linked with the main Kabul-Jalalabad highway through an 18 km stretch of a paved road which gives it a better geographical situation comparing to Qarghayi other cities of Eastern Afghanistan. 4 The main bazaar of Mehterlam is located at the junction of Ali Nagar; the Ali Nagar replaced the old Tirkery bazaar which is 2 km from Mehterlam on a hillside. In 19th century Tirkery was a walled city and the seat of the local sardaar. In upper Laghman there is a town named Mandror which faces the ancient, walled city of Charbagh; the city of Charbagh was famous for its armament productions in 19th century, and it is the only town in the region which has its ancient structure Contact: and bazaar. Samim Yaquby and Daud Sahar [email protected] In Sorkhrod valley there are smaller bazaars. Generally all the bazaars are crowded during winters because of the mild temperatures. In 19th century most of the bazaars in Laghman were run by Hindus. These ba- zaars were the main routes for travelers and merchants passing between India and Kabul through the Khyber Pass. As a result, many caravansaries were built along this ancient road. -

Soviet-Afghan War Operations 1) Kabul Area
Soviet-Afghan War Operations This document is designed to be used with the Soviet Afghan War Scenario Location Map.pdf file located in the main game directory, which provides an overview map of the nation and general locations of the actions listed here. 1) Kabul area 001.Amin's End.scn - 20 turns, Company (Supported) Level, PBEM Play: Yes, Solo Play: Yes **Important Note: This scenario has special victory conditions. There are no objectives or victory points. Soviet troops must capture/destroy President H. Amin to get Major Victory. Afghan troops will get a Major Victory if they can defend Amin or he can escape the map. There are no other victory levels. 27 December 1979, Tajbeg Palace, 20kms South of Kabul: The Soviet invasion of Afghanistan started with the attempts to capture key government and communication centers to isolate the Afghan political leadership in Kabul. Seeing this president Hafizullah Amin (Who himself had become power after a bloody plot resulted with the assassination of his predecessor Nur Muhammed Taraki) moved the presidential offices to the Tajbeg Palace, believing this location to be more defendable against an invasion. The Palace was located a few kms south of Kabul near the Darulaman gardens; former home of the fallen Pathan Dynasty. Amin gathered a small force from the troops who are still loyal to him including some armor from the Kabul garrison. On December 27, 1979 Soviet troops, including KGB Spetsnaz Special Forces troops from the Alpha Group and Zenith Group, moved to occupy major governmental, military and media buildings in Kabul, including their primary target - the Tajbeg Presidential Palace. -

EASO, Country Guidance: Afghanistan
European Asylum Support Office Country Guidance: Afghanistan Guidance note and common analysis The country guidance represents the common assessment of the situation in the country of origin by EU Member States. June 2019 SUPPORT IS OUR MISSION European Asylum Support Office Country Guidance: Afghanistan Guidance note and common analysis This document updates the ‘Country Guidance: Afghanistan’ published in June 2018. The country guidance represents the common assessment of the situation in the country of origin by senior policy officials from EU Member States, in accordance with current EU legislation and jurisprudence of the Court of Justice of the European Union (CJEU). This guidance note does not release Member States from the obligation to individually, objectively and impartially examine each application for international protection. Each decision should be taken on the basis of the individual circumstances of the applicant and the situation in Afghanistan at the moment of the decision, according to precise and up-to-date country information, obtained from various relevant sources (Article 10 of the Asylum Procedures Directive). The analysis and guidance provided within this document are not exhaustive. June 2019 Europe Direct is a service to help you find answers to your questions about the European Union. Freephone number (*): 00 800 6 7 8 9 10 11 (*) Certain mobile telephone operators do not allow access to 00800 numbers or these calls may be billed. More information on the European Union is available on the Internet (http://europa.eu). ISBN 978-92-9485-055-3 doi: 10.2847/464275 © European Asylum Support Office 2019 Neither EASO nor any person acting on its behalf may be held responsible for the use which may be made of the information contained herein.