Applied Anatomy of the Knee
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Synovial Joints Permit Movements of the Skeleton
8 Joints Lecture Presentation by Lori Garrett © 2018 Pearson Education, Inc. Section 1: Joint Structure and Movement Learning Outcomes 8.1 Contrast the major categories of joints, and explain the relationship between structure and function for each category. 8.2 Describe the basic structure of a synovial joint, and describe common accessory structures and their functions. 8.3 Describe how the anatomical and functional properties of synovial joints permit movements of the skeleton. © 2018 Pearson Education, Inc. Section 1: Joint Structure and Movement Learning Outcomes (continued) 8.4 Describe flexion/extension, abduction/ adduction, and circumduction movements of the skeleton. 8.5 Describe rotational and special movements of the skeleton. © 2018 Pearson Education, Inc. Module 8.1: Joints are classified according to structure and movement Joints, or articulations . Locations where two or more bones meet . Only points at which movements of bones can occur • Joints allow mobility while preserving bone strength • Amount of movement allowed is determined by anatomical structure . Categorized • Functionally by amount of motion allowed, or range of motion (ROM) • Structurally by anatomical organization © 2018 Pearson Education, Inc. Module 8.1: Joint classification Functional classification of joints . Synarthrosis (syn-, together + arthrosis, joint) • No movement allowed • Extremely strong . Amphiarthrosis (amphi-, on both sides) • Little movement allowed (more than synarthrosis) • Much stronger than diarthrosis • Articulating bones connected by collagen fibers or cartilage . Diarthrosis (dia-, through) • Freely movable © 2018 Pearson Education, Inc. Module 8.1: Joint classification Structural classification of joints . Fibrous • Suture (sutura, a sewing together) – Synarthrotic joint connected by dense fibrous connective tissue – Located between bones of the skull • Gomphosis (gomphos, bolt) – Synarthrotic joint binding teeth to bony sockets in maxillae and mandible © 2018 Pearson Education, Inc. -

Chapter Nine- Joints and Articulations
Chapter 9 Activity: Joints 1. List the three structural categories of joints and briefly describe the criteria used for structural classification of joints. 2. List the three functional classifications of joints, and briefly describe the basis for the functional classification of joints. 3. Which functional class of joints contains joints that are freely movable? 1. Synarthrosis 2. Amphiarthrosis 3. Diarthrosis a) 1 only c) 3 only e) All of these choices b) 2 only d) Both 2 and 3 4. Which of the following is a type of fibrous joint composed of a thin layer of dense irregular fibrous connective tissue found between the bones of the skull? 1. Syndesmoses 2. Gomphosis 3. Suture a) 1 only c) 3 only e) None of these choices b) 2 only d) Both 1 and 2 5. The epiphyseal plate in a long bone is an example of which type of joint? a) Gomphosis c) Symphysis e) Synchondrosis b) Suture d) Synovial 6. The joint between the first rib and the manubrium of the sternum is classified as a) a synchondrosis. c) a cartilaginous joint. e) None of these choices. b) a synarthrosis. d) All of these choices. 7. Which of the following is(are) made from dense regular connective tissue? a) Ligaments c) Articular fat pads e) Synovial fluid b) Articular cartilage d) Synovial membrane 8. What unique characteristics would a person who is "double-jointed” possess? Answer: 9. Briefly describe the functions of synovial fluid. Answer: 10. Briefly describe what is happening when a person “cracks their knuckles”. Answer: 11. Which of the following structures include the fibular and tibial collateral ligaments of the knee joint? a) Synovial membranes c) Menisci e) Tendon sheath b) Articular fat pads d) Extracapsular ligaments 12. -

The Anatomy of the Posterolateral Aspect of the Rabbit Knee
Journal of Orthopaedic Research ELSEVIER Journal of Orthopaedic Research 2 I (2003) 723-729 www.elsevier.com/locate/orthres The anatomy of the posterolateral aspect of the rabbit knee Joshua A. Crum, Robert F. LaPrade *, Fred A. Wentorf Dc~~ur/niiviiof Orthopuer/ic Surgery. Unicrrsity o/ Minnesotu. MMC 492, 420 Dcluwur-c Si. S. E., Minnwpoli,s, MN 55455, tiSA Accepted 14 November 2002 Abstract The purpose of this study was to determine the anatomy of the posterolateral aspect of the rabbit knee to serve as a basis for future in vitro and in vivo posterolateral knee biomechanical and injury studies. Twelve nonpaired fresh-frozen New Zealand white rabbit knees were dissected to determine the anatomy of the posterolateral corner. The following main structures were consistently identified in the rabbit posterolateral knee: the gastrocnemius muscles, biceps femoris muscle, popliteus muscle and tendon, fibular collateral ligament, posterior capsule, ligament of Wrisberg, and posterior meniscotibial ligament. The fibular collateral ligament was within the joint capsule and attached to the femur at the lateral epi- condyle and to the fibula at the midportion of the fibular head. The popliteus muscle attached to the medial edge of the posterior tibia and ascended proximally to give rise to the popliteus tendon, which inserted on the proximal aspect of the popliteal sulcus just anterior to the fibular collateral ligament. The biceps femoris had no attachment to the fibula and attached to the anterior com- partment fascia of the leg. This study increased our understanding of these structures and their relationships to comparative anatomy in the human knee. -
Isaac Newton Academy Revision Booklet- Exam 1
Isaac Newton Academy Revision Booklet- Exam 1 Component 01: Physical factors affecting performance 1.1 Applied anatomy and physiology 1.2 Physical training. Functions of the skeleton Location of Major Bones Bone stores crucial nutrients, minerals, and lipids and produces blood cells that nourish the body and play a vital role in protecting the body against infection. Bones have many functions, including the following: Support: Bones provide a framework for the attachment of muscles and other tissues. Bone Location Arm - humerus, radius and ulna. Hand - Carpals, Metacarpals and Phalanges. Sternum and Ribs. Femur – the thigh bone. Patella – the knee cap. Tibia – the shin bone, the larger of the two leg bones located below the knee cap. Fibula – the smaller of the two leg bones located below the knee cap. The OCR Spec expects us to know the following regarding synovial joints: The definition of a synovial joint, Articulating bones of the knee and elbow hinge joints and also the articulating bones of the shoulder and hip Ball and socket joints Hinge Joint- A hinge joint is found at the knee and the elbow, Synovial Joint- This is a freely moveable joint in thich the bones’ surfaces are covered Articulating bones of the elbow by cartilage and connected by joint are the Humerus radius fibrous connective tissue and Ulna . Articulating bones of capsule lines with synovial the knee are the Femur and fluid Tibia. Ball and socket joint- Allows a wide range of movement, they can be Articulating bones- These found at the hip and shoulder. are bones that move within a joint Articulating bones of the shoulder are Humerus and Scapula. -

Skier Tibia (Leg) Fractures
Skier Tibia (Leg) Fractures In years past, the prototypical ski fracture was sustained at the lower part of the outside of the leg in the region of the ankle. However, in the past 10 years, with the advent of the modern ski boots and improvements in binding, the most commonly seen lower leg skier fracture is the tibia (or shinbone) fracture. 10% of these fractures are associated with a collision. Thus, 90 % are associated with an isolated fall or noncontact type of injury, which is generally the result of binding malfunctions and inappropriate release. The most common mechanism leading to a tibia (leg) fracture is a forward fall. Risk factors for sustaining a skier tibia fracture include: beginners or novice skiers, less than 20 years of age, higher outdoor temperatures, and increased snow depth. Non-risk factors include ski lengths, icy conditions, and male versus female sex. The modern ski boot very closely resembles an extremely well padded short leg cast in the treatment of many orthopaedic lower extremity fractures. It of course goes to a much higher level than the former shorter boot top-level varieties. The binding release and designs have been based on the fracture strength of the adult tibia (shin) bone at the top of the modern ski boot. The treatment of most skier leg fractures includes a closed reduction and cast application for variable periods of time, with or without weight bearing allowed. However, severe misalignments of the bones can lead to later bony prominences that may be incompatible with snug, rigid, high fitting ski boots. -

Assessment, Management and Decision Making in the Treatment Of
Pediatric Ankle Fractures Anthony I. Riccio, MD Texas Scottish Rite Hospital for Children Update 07/2016 Pediatric Ankle Fractures The Ankle is the 2nd most Common Site of Physeal Injury in Children 10-25% of all Physeal Injuries Occur About the Ankle Pediatric Ankle Fractures Primary Concerns Are: • Anatomic Restoration of Articular Surface • Restoration of Symmetric Ankle Mortise • Preservation of Physeal Growth • Minimize Iatrogenic Physeal Injury • Avoid Fixation Across Physis in Younger Children Salter Harris Classification Prognosis and Treatment of Pediatric Ankle Fractures is Often Dictated by the Salter Harris Classification of Physeal Fractures Type I and II Fractures: Often Amenable to Closed Tx / Lower Risk of Physeal Arrest Type III and IV: More Likely to Require Operative Tx / Higher Risk of Physeal Arrest Herring JA, ed. Tachdjian’s Pediatric Orthopaedics, 5th Ed. 2014. Elsevier. Philadelphia, PA. ISOLATED DISTAL FIBULA FRACTURES Distal Fibula Fractures • The Physis is Weaker than the Lateral Ankle Ligaments – Children Often Fracture the Distal Fibula but…. – …ligamentous Injuries are Not Uncommon • Mechanism of Injury = Inversion of a Supinated Foot • SH I and II Fractures are Most Common – SH I Fractures: Average Age = 10 Years – SH II Fractures: Average Age = 12 Years Distal Fibula Fractures Lateral Ankle Tenderness SH I Distal Fibula Fracture vs. Lateral Ligamentous Injury (Sprain) Distal Fibula Fractures • Sankar et al (JPO 2008) – 37 Children – All with Open Physes, Lateral Ankle Tenderness + Normal Films – 18%: Periosteal -

About Your Knee
OrthoInfo Basics About Your Knee What are the parts of the knee? Your knee is Your knee is made up of four main things: bones, cartilage, ligaments, the largest joint and tendons. in your body Bones. Three bones meet to form your knee joint: your thighbone and one of the (femur), shinbone (tibia), and kneecap (patella). Your patella sits in most complex. front of the joint and provides some protection. It is also vital Articular cartilage. The ends of your thighbone and shinbone are covered with articular cartilage. This slippery substance to movement. helps your knee bones glide smoothly across each other as you bend or straighten your leg. Because you use it so Two wedge-shaped pieces of meniscal cartilage act as much, it is vulnerable to Meniscus. “shock absorbers” between your thighbone and shinbone. Different injury. Because it is made from articular cartilage, the meniscus is tough and rubbery to help up of so many parts, cushion and stabilize the joint. When people talk about torn cartilage many different things in the knee, they are usually referring to torn meniscus. can go wrong. Knee pain or injury Femur is one of the most (thighbone) common reasons people Patella (kneecap) see their doctors. Most knee problems can be prevented or treated with simple measures, such as exercise or Articular cartilage training programs. Other problems require surgery Meniscus to correct. Tibia (shinbone) 1 OrthoInfo Basics — About Your Knee What are ligaments and tendons? Ligaments and tendons connect your thighbone Collateral ligaments. These are found on to the bones in your lower leg. -

Anterior (Cranial) Cruciate Ligament Rupture
Cranial Cruciate Ligament Rupture in Dogs The cruciate ligaments are tough fibrous bands that connect the distal femur (thigh bone) to the proximal tibia (shin bone). Two cruciate ligaments, the cranial (anterior) and the posterior cruciate ligaments, are found in the knee joint of dogs and cats (and most other domestic animals). These ligaments work like a hinge joint in the knee and are responsible for providing anterior-posterior stability to the knee joint. Normal Knee Joint of a Dog Rupture of the cranial cruciate ligament is rare in cats. It occurs frequently in overweight, middle- and older-aged dogs. Certain dog breeds appear to be predisposed to cranial cruciate ligament rupture. Most commonly, the cocker spaniel and rottweiler are affected. The miniature and toy poodle, Lhasa apso, bichon frise, golden retriever, Labrador retriever, German shepherd and mastiff seem to be predisposed as well. The normal knee joint works as a hinge, keeping the knee stable as it bends. Tearing of the cranial cruciate ligament causes instability of the knee joint and it ceases to function properly. Most cranial cruciate ligament tears in dogs occur gradually, resulting in a low-level lameness that may or nay not improve over time. After the ligament tears, inflammation occurs within the joint. Continued use and weight bearing by the dog often causes the ligament to rupture completely. Dogs that rupture one cruciate ligament have about a fifty percent chance of rupturing the other. Normal Knee Joint of a Dog Rupture of the cranial cruciate ligament in dogs can also occur acutely. Similar to cranial cruciate ligament rupture in humans, resulting from athletic injuries to the knee, dogs can tear this ligament by jumping up to catch a ball or Frisbee or by jumping out of a truck or off a porch. -
Joints Classification of Joints
Joints Classification of Joints . Functional classification (Focuses on amount of movement) . Synarthroses (immovable joints) . Amphiarthroses (slightly movable joints) . Diarthroses (freely movable joints) . Structural classification (Based on the material binding them and presence or absence of a joint cavity) . Fibrous mostly synarthroses . Cartilagenous mostly amphiarthroses . Synovial diarthroses Table of Joint Types Functional across Synarthroses Amphiarthroses Diarthroses (immovable joints) (some movement) (freely movable) Structural down Bony Fusion Synostosis (frontal=metopic suture; epiphyseal lines) Fibrous Suture (skull only) Syndesmoses Syndesmoses -fibrous tissue is -ligaments only -ligament longer continuous with between bones; here, (example: radioulnar periosteum short so some but not interosseous a lot of movement membrane) (example: tib-fib Gomphoses (teeth) ligament) -ligament is periodontal ligament Cartilagenous Synchondroses Sympheses (bone united by -hyaline cartilage -fibrocartilage cartilage only) (examples: (examples: between manubrium-C1, discs, pubic epiphyseal plates) symphesis Synovial Are all diarthrotic Fibrous joints . Bones connected by fibrous tissue: dense regular connective tissue . No joint cavity . Slightly immovable or not at all . Types . Sutures . Syndesmoses . Gomphoses Sutures . Only between bones of skull . Fibrous tissue continuous with periosteum . Ossify and fuse in middle age: now technically called “synostoses”= bony junctions Syndesmoses . In Greek: “ligament” . Bones connected by ligaments only . Amount of movement depends on length of the fibers: longer than in sutures Gomphoses . Is a “peg-in-socket” . Only example is tooth with its socket . Ligament is a short periodontal ligament Cartilagenous joints . Articulating bones united by cartilage . Lack a joint cavity . Not highly movable . Two types . Synchondroses (singular: synchondrosis) . Sympheses (singular: symphesis) Synchondroses . Literally: “junction of cartilage” . Hyaline cartilage unites the bones . Immovable (synarthroses) . -

38.3 Joints and Skeletal Movement.Pdf
1198 Chapter 38 | The Musculoskeletal System Decalcification of Bones Question: What effect does the removal of calcium and collagen have on bone structure? Background: Conduct a literature search on the role of calcium and collagen in maintaining bone structure. Conduct a literature search on diseases in which bone structure is compromised. Hypothesis: Develop a hypothesis that states predictions of the flexibility, strength, and mass of bones that have had the calcium and collagen components removed. Develop a hypothesis regarding the attempt to add calcium back to decalcified bones. Test the hypothesis: Test the prediction by removing calcium from chicken bones by placing them in a jar of vinegar for seven days. Test the hypothesis regarding adding calcium back to decalcified bone by placing the decalcified chicken bones into a jar of water with calcium supplements added. Test the prediction by denaturing the collagen from the bones by baking them at 250°C for three hours. Analyze the data: Create a table showing the changes in bone flexibility, strength, and mass in the three different environments. Report the results: Under which conditions was the bone most flexible? Under which conditions was the bone the strongest? Draw a conclusion: Did the results support or refute the hypothesis? How do the results observed in this experiment correspond to diseases that destroy bone tissue? 38.3 | Joints and Skeletal Movement By the end of this section, you will be able to do the following: • Classify the different types of joints on the basis of structure • Explain the role of joints in skeletal movement The point at which two or more bones meet is called a joint, or articulation. -

Compiled for Lower Limb
Updated: December, 9th, 2020 MSI ANATOMY LAB: STRUCTURE LIST Lower Extremity Lower Extremity Osteology Hip bone Tibia • Greater sciatic notch • Medial condyle • Lesser sciatic notch • Lateral condyle • Obturator foramen • Tibial plateau • Acetabulum o Medial tibial plateau o Lunate surface o Lateral tibial plateau o Acetabular notch o Intercondylar eminence • Ischiopubic ramus o Anterior intercondylar area o Posterior intercondylar area Pubic bone (pubis) • Pectineal line • Tibial tuberosity • Pubic tubercle • Medial malleolus • Body • Superior pubic ramus Patella • Inferior pubic ramus Fibula Ischium • Head • Body • Neck • Ramus • Lateral malleolus • Ischial tuberosity • Ischial spine Foot • Calcaneus Ilium o Calcaneal tuberosity • Iliac fossa o Sustentaculum tali (talar shelf) • Anterior superior iliac spine • Anterior inferior iliac spine • Talus o Head • Posterior superior iliac spine o Neck • Posterior inferior iliac spine • Arcuate line • Navicular • Iliac crest • Cuboid • Body • Cuneiforms: medial, intermediate, and lateral Femur • Metatarsals 1-5 • Greater trochanter • Phalanges 1-5 • Lesser trochanter o Proximal • Head o Middle • Neck o Distal • Linea aspera • L • Lateral condyle • L • Intercondylar fossa (notch) • L • Medial condyle • L • Lateral epicondyle • L • Medial epicondyle • L • Adductor tubercle • L • L • L • L • 1 Updated: December, 9th, 2020 Lab 3: Anterior and Medial Thigh Anterior Thigh Medial thigh General Structures Muscles • Fascia lata • Adductor longus m. • Anterior compartment • Adductor brevis m. • Medial compartment • Adductor magnus m. • Great saphenous vein o Adductor hiatus • Femoral sheath o Compartments and contents • Pectineus m. o Femoral canal and ring • Gracilis m. Muscles & Associated Tendons Nerves • Tensor fasciae lata • Obturator nerve • Iliotibial tract (band) • Femoral triangle: Boundaries Vessels o Inguinal ligament • Obturator artery o Sartorius m. • Femoral artery o Adductor longus m. -
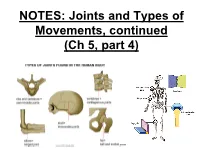
NOTES: Joints and Types of Movements, Continued (Ch 7, Part 4)
NOTES: Joints and Types of Movements, continued (Ch 5, part 4) *Joints are functional junctions between bones. TYPES OF JOINTS **Joints can be classified according to the type of tissue that binds the bones together.** FIBROUS JOINTS: • bones at fibrous joints are tightly joined by a layer of dense connective tissue. • little or no movement occurs at a fibrous joint • Example: the sutures between the flat bones of the skull CARTILAGINOUS JOINTS: • a layer of hyaline cartilage, or fibrocartilage, joins bones of cartilaginous joints • allow limited movement • Example: the joints that separate the vertebrae SYNOVIAL JOINTS: • most joints in the body are synovial joints • allow free movement • bones at synovial joints are covered with hyaline cartilage (“articular cartilage”) and held together by a fibrous JOINT CAPSULE. SYNOVIAL JOINTS: • the joint capsule consists of an outer layer of ligaments and an inner lining of synovial membrane (which secretes synovial fluid to lubricate the joint). • some synovial joints have flattened, shock- absorbing pads of fibrocartilage called MENISCI between the articulating surfaces of the bones SYNOVIAL JOINTS: • some synovial joints may also have BURSAE, which are fluid-filled sacs located between the skin and the underlying bony prominences. • Example: at the knee joint, the patella is sandwiched between 2 bursae. TYPES OF SYNOVIAL JOINTS: • Ball-and-socket - round head of one bone rests within a cup-shaped depression of another - all angular and rotational movements, including circumduction can be performed by this joint TYPES OF SYNOVIAL JOINTS: • Gliding (planar) – Have flattened or slightly curved faces – Flat articular surfaces slide across one another – Amount of movements is slightly TYPES OF SYNOVIAL JOINTS: • Condylar (ellipsoid) – Oval articular face nests within a depression in opposing surface – Angular movements occur in 2 planes: along or across length of oval TYPES OF SYNOVIAL JOINTS: • Hinge – Permits angular motion in single plane (e.g.