Synovial Joints Permit Movements of the Skeleton
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Structure and Function of Breathing
CHAPTERCONTENTS The structure-function continuum 1 Multiple Influences: biomechanical, biochemical and psychological 1 The structure and Homeostasis and heterostasis 2 OBJECTIVE AND METHODS 4 function of breathing NORMAL BREATHING 5 Respiratory benefits 5 Leon Chaitow The upper airway 5 Dinah Bradley Thenose 5 The oropharynx 13 The larynx 13 Pathological states affecting the airways 13 Normal posture and other structural THE STRUCTURE-FUNCTION considerations 14 Further structural considerations 15 CONTINUUM Kapandji's model 16 Nowhere in the body is the axiom of structure Structural features of breathing 16 governing function more apparent than in its Lung volumes and capacities 19 relation to respiration. This is also a region in Fascla and resplrstory function 20 which prolonged modifications of function - Thoracic spine and ribs 21 Discs 22 such as the inappropriate breathing pattern dis- Structural features of the ribs 22 played during hyperventilation - inevitably intercostal musculature 23 induce structural changes, for example involving Structural features of the sternum 23 Posterior thorax 23 accessory breathing muscles as well as the tho- Palpation landmarks 23 racic articulations. Ultimately, the self-perpetuat- NEURAL REGULATION OF BREATHING 24 ing cycle of functional change creating structural Chemical control of breathing 25 modification leading to reinforced dysfunctional Voluntary control of breathing 25 tendencies can become complete, from The autonomic nervous system 26 whichever direction dysfunction arrives, for Sympathetic division 27 Parasympathetic division 27 example: structural adaptations can prevent NANC system 28 normal breathing function, and abnormal breath- THE MUSCLES OF RESPIRATION 30 ing function ensures continued structural adap- Additional soft tissue influences and tational stresses leading to decompensation. -

Chapter Nine- Joints and Articulations
Chapter 9 Activity: Joints 1. List the three structural categories of joints and briefly describe the criteria used for structural classification of joints. 2. List the three functional classifications of joints, and briefly describe the basis for the functional classification of joints. 3. Which functional class of joints contains joints that are freely movable? 1. Synarthrosis 2. Amphiarthrosis 3. Diarthrosis a) 1 only c) 3 only e) All of these choices b) 2 only d) Both 2 and 3 4. Which of the following is a type of fibrous joint composed of a thin layer of dense irregular fibrous connective tissue found between the bones of the skull? 1. Syndesmoses 2. Gomphosis 3. Suture a) 1 only c) 3 only e) None of these choices b) 2 only d) Both 1 and 2 5. The epiphyseal plate in a long bone is an example of which type of joint? a) Gomphosis c) Symphysis e) Synchondrosis b) Suture d) Synovial 6. The joint between the first rib and the manubrium of the sternum is classified as a) a synchondrosis. c) a cartilaginous joint. e) None of these choices. b) a synarthrosis. d) All of these choices. 7. Which of the following is(are) made from dense regular connective tissue? a) Ligaments c) Articular fat pads e) Synovial fluid b) Articular cartilage d) Synovial membrane 8. What unique characteristics would a person who is "double-jointed” possess? Answer: 9. Briefly describe the functions of synovial fluid. Answer: 10. Briefly describe what is happening when a person “cracks their knuckles”. Answer: 11. Which of the following structures include the fibular and tibial collateral ligaments of the knee joint? a) Synovial membranes c) Menisci e) Tendon sheath b) Articular fat pads d) Extracapsular ligaments 12. -

Peripartum Pubic Symphysis Diastasis—Practical Guidelines
Journal of Clinical Medicine Review Peripartum Pubic Symphysis Diastasis—Practical Guidelines Artur Stolarczyk , Piotr St˛epi´nski* , Łukasz Sasinowski, Tomasz Czarnocki, Michał D˛ebi´nski and Bartosz Maci ˛ag Department of Orthopedics and Rehabilitation, Medical University of Warsaw, 02-091 Warsaw, Poland; [email protected] (A.S.); [email protected] (Ł.S.); [email protected] (T.C.); [email protected] (M.D.); [email protected] (B.M.) * Correspondence: [email protected] Abstract: Optimal development of a fetus is made possible due to a lot of adaptive changes in the woman’s body. Some of the most important modifications occur in the musculoskeletal system. At the time of childbirth, natural widening of the pubic symphysis and the sacroiliac joints occur. Those changes are often reversible after childbirth. Peripartum pubic symphysis separation is a relatively rare disease and there is no homogeneous approach to treatment. The paper presents the current standards of diagnosis and treatment of pubic diastasis based on orthopedic and gynecological indications. Keywords: pubic symphysis separation; pubic symphysis diastasis; pubic symphysis; pregnancy; PSD 1. Introduction The proper development of a fetus is made possible due to numerous adaptive Citation: Stolarczyk, A.; St˛epi´nski,P.; changes in women’s bodies, including such complicated systems as: endocrine, nervous Sasinowski, Ł.; Czarnocki, T.; and musculoskeletal. With regard to the latter, those changes can be observed particularly D˛ebi´nski,M.; Maci ˛ag,B. Peripartum Pubic Symphysis Diastasis—Practical in osteoarticular and musculo-ligamento-fascial structures. Almost all of those changes Guidelines. J. Clin. Med. -

Synovial Fluidfluid 11
LWBK461-c11_p253-262.qxd 11/18/09 6:04 PM Page 253 Aptara Inc CHAPTER SynovialSynovial FluidFluid 11 Key Terms ANTINUCLEAR ANTIBODY ARTHROCENTESIS BULGE TEST CRYSTAL-INDUCED ARTHRITIS GROUND PEPPER HYALURONATE MUCIN OCHRONOTIC SHARDS RHEUMATOID ARTHRITIS (RA) RHEUMATOID FACTOR (RF) RICE BODIES ROPE’S TEST SEPTIC ARTHRITIS Learning Objectives SYNOVIAL SYSTEMIC LUPUS ERYTHEMATOSUS 1. Define synovial. VISCOSITY 2. Describe the formation and function of synovial fluid. 3. Explain the collection and handling of synovial fluid. 4. Describe the appearance of normal and abnormal synovial fluids. 5. Correlate the appearance of synovial fluid with possible cause. 6. Interpret laboratory tests on synovial fluid. 7. Suggest further testing for synovial fluid, based on preliminary results. 8. List the four classes or categories of joint disease. 9. Correlate synovial fluid analyses with their representative disease classification. 253 LWBK461-c11_p253-262.qxd 11/18/09 6:04 PM Page 254 Aptara Inc 254 Graff’s Textbook of Routine Urinalysis and Body Fluids oint fluid is called synovial fluid because of its resem- blance to egg white. It is a viscous, mucinous substance Jthat lubricates most joints. Analysis of synovial fluid is important in the diagnosis of joint disease. Aspiration of joint fluid is indicated for any patient with a joint effusion or inflamed joints. Aspiration of asymptomatic joints is beneficial for patients with gout and pseudogout as these fluids may still contain crystals.1 Evaluation of physical, chemical, and microscopic characteristics of synovial fluid comprise routine analysis. This chapter includes an overview of the composition and function of synovial fluid, and laboratory procedures and their interpretations. -

Traumatologia Hiztegia
Traumatologia HIZTEGIA KULTURA ETA HIZKUNTZA POLITIKA SAILA DEPARTAMENTO DE CULTURA Y POLÍTICA LINGÜÍSTICA Vitoria-Gasteiz, 2017 Lan honen bibliografia-erregistroa Eusko Jaurlaritzaren Bibliotekak sarearen katalogoan aurki daiteke: http://www.bibliotekak.euskadi.eus/WebOpac Argitaraldia: 1.a, 2017ko xxxx Ale-kopurua: 1.500 ale © argitaraldi honena: Euskal Autonomia Erkidegoko Administrazio Orokorra Argitaratzailea: Eusko Jaurlaritzaren Argitalpen Zerbitzu Nagusia Servicio Central de Publicaciones del Gobierno Vasco Donostia-San Sebastián, 1 - 01010 Vitoria-Gasteiz Internet: http://www.euskara.euskadi.eus/euskalterm Azala: Concetta Probanza Inprimaketa: XXXXXXXXXXXXXXXXXXX ISBN: XXXXXXXXXXXXXX Lege gordailua: XXXXXXXXX HITZAURREA Beste edozein hizkuntza bezalaxe, euskara ere berritzen eta modernizatzen doa egunetik egunera, bizirik dagoen seinale. Bide horretan ezinbestekoa da euskararen aberastasun lexikoa elikatzea, zaintzea eta sustatzea, bai hizkuntza bera normalizatzeko, bai erabiltzaileen premietara egokitzeko. Hain zuzen ere, helburu horiek bete nahian ikusi du argia eskuartean duzun hiztegi honek, orrialde hauetan jorratzen den eremuko erabiltzaile eta hiztunek lanabes erabilgarria izan dezaten beren egunerokoan. Hiztegi honetan aurkituko duzun terminologia Euskararen Aholku Batzordearen Terminologia Batzordeak gomendatutakoa da. Batzordeari dagokio, besteak beste, terminologia-alorrean dauden lehentasunak finkatzea, lan-proposamenak egitea, terminologia- lanerako irizpideak ezartzea, ponderazio-markak finkatuta termino lehiakideen -

About Your Knee
OrthoInfo Basics About Your Knee What are the parts of the knee? Your knee is Your knee is made up of four main things: bones, cartilage, ligaments, the largest joint and tendons. in your body Bones. Three bones meet to form your knee joint: your thighbone and one of the (femur), shinbone (tibia), and kneecap (patella). Your patella sits in most complex. front of the joint and provides some protection. It is also vital Articular cartilage. The ends of your thighbone and shinbone are covered with articular cartilage. This slippery substance to movement. helps your knee bones glide smoothly across each other as you bend or straighten your leg. Because you use it so Two wedge-shaped pieces of meniscal cartilage act as much, it is vulnerable to Meniscus. “shock absorbers” between your thighbone and shinbone. Different injury. Because it is made from articular cartilage, the meniscus is tough and rubbery to help up of so many parts, cushion and stabilize the joint. When people talk about torn cartilage many different things in the knee, they are usually referring to torn meniscus. can go wrong. Knee pain or injury Femur is one of the most (thighbone) common reasons people Patella (kneecap) see their doctors. Most knee problems can be prevented or treated with simple measures, such as exercise or Articular cartilage training programs. Other problems require surgery Meniscus to correct. Tibia (shinbone) 1 OrthoInfo Basics — About Your Knee What are ligaments and tendons? Ligaments and tendons connect your thighbone Collateral ligaments. These are found on to the bones in your lower leg. -

Monitoring Methods of Human Body Joints: State-Of-The-Art and Research Challenges
sensors Review Monitoring Methods of Human Body Joints: State-of-the-Art and Research Challenges Abu Ilius Faisal 1, Sumit Majumder 1 , Tapas Mondal 2, David Cowan 3, Sasan Naseh 1 and M. Jamal Deen 1,* 1 Department of Electrical and Computer Engineering, McMaster University, Hamilton, ON L8S 4L8, Canada; [email protected] (A.I.F.); [email protected] (S.M.); [email protected] (S.N.) 2 Department of Pediatrics, McMaster University, Hamilton, ON L8S 4L8, Canada; [email protected] 3 Department of Medicine, St. Joseph’s Healthcare Hamilton, Hamilton, ON L8N 4A6, Canada; [email protected] * Correspondence: [email protected]; Tel.: +1-905-5259-140 (ext. 27137) Received: 26 April 2019; Accepted: 4 June 2019; Published: 10 June 2019 Abstract: The world’s population is aging: the expansion of the older adult population with multiple physical and health issues is now a huge socio-economic concern worldwide. Among these issues, the loss of mobility among older adults due to musculoskeletal disorders is especially serious as it has severe social, mental and physical consequences. Human body joint monitoring and early diagnosis of these disorders will be a strong and effective solution to this problem. A smart joint monitoring system can identify and record important musculoskeletal-related parameters. Such devices can be utilized for continuous monitoring of joint movements during the normal daily activities of older adults and the healing process of joints (hips, knees or ankles) during the post-surgery period. A viable monitoring system can be developed by combining miniaturized, durable, low-cost and compact sensors with the advanced communication technologies and data processing techniques. -
Joints Classification of Joints
Joints Classification of Joints . Functional classification (Focuses on amount of movement) . Synarthroses (immovable joints) . Amphiarthroses (slightly movable joints) . Diarthroses (freely movable joints) . Structural classification (Based on the material binding them and presence or absence of a joint cavity) . Fibrous mostly synarthroses . Cartilagenous mostly amphiarthroses . Synovial diarthroses Table of Joint Types Functional across Synarthroses Amphiarthroses Diarthroses (immovable joints) (some movement) (freely movable) Structural down Bony Fusion Synostosis (frontal=metopic suture; epiphyseal lines) Fibrous Suture (skull only) Syndesmoses Syndesmoses -fibrous tissue is -ligaments only -ligament longer continuous with between bones; here, (example: radioulnar periosteum short so some but not interosseous a lot of movement membrane) (example: tib-fib Gomphoses (teeth) ligament) -ligament is periodontal ligament Cartilagenous Synchondroses Sympheses (bone united by -hyaline cartilage -fibrocartilage cartilage only) (examples: (examples: between manubrium-C1, discs, pubic epiphyseal plates) symphesis Synovial Are all diarthrotic Fibrous joints . Bones connected by fibrous tissue: dense regular connective tissue . No joint cavity . Slightly immovable or not at all . Types . Sutures . Syndesmoses . Gomphoses Sutures . Only between bones of skull . Fibrous tissue continuous with periosteum . Ossify and fuse in middle age: now technically called “synostoses”= bony junctions Syndesmoses . In Greek: “ligament” . Bones connected by ligaments only . Amount of movement depends on length of the fibers: longer than in sutures Gomphoses . Is a “peg-in-socket” . Only example is tooth with its socket . Ligament is a short periodontal ligament Cartilagenous joints . Articulating bones united by cartilage . Lack a joint cavity . Not highly movable . Two types . Synchondroses (singular: synchondrosis) . Sympheses (singular: symphesis) Synchondroses . Literally: “junction of cartilage” . Hyaline cartilage unites the bones . Immovable (synarthroses) . -
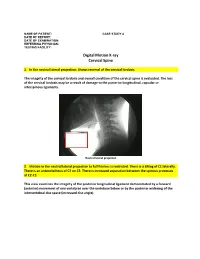
Digital Motion X-Ray Cervical Spine
NAME OF PATIENT: CASE STUDY 4 DATE OF REPORT: DATE OF EXAMINATION: REFERRING PHYSICIAN: TESTING FACILITY: Digital Motion X-ray Cervical Spine 1. In the neutral lateral projection: Shows reversal of the cervical lordosis. The integrity of the cervical lordosis and overall condition of the cervical spine is evaluated. The loss of the cervical lordosis may be a result of damage to the posterior longitudinal, capsular or interspinous ligaments. Neutral lateral projection 2. Motion in the neutral lateral projection to full flexion: Is restricted. There is a tilting of C1 laterally. There is an anterolisthesis of C2 on C3. There is increased separation between the spinous processes at C2-C3. This view examines the integrity of the posterior longitudinal ligament demonstrated by a forward (anterior) movement of one vertebrae over the vertebrae below or by the posterior widening of the intervertebral disc space (increased disc angle). Widening of posterior disc space Anterolisthesis The integrity of the interspinous ligament is evaluated in the lateral flexion view. Damage to this ligament results in increased separation of the spinous processes in flexion. Damaged Interspinous Ligament Full flexion projection 3. Motion in the neutral lateral projection to full extension: Is restricted. There is a retrolisthesis of C4 on C5. This view examines the integrity of the anterior longitudinal ligament demonstrated by a backward (posterior) movement of one vertebrae over the vertebrae below or by the anterior widening of the intervertebral disc space (increased disc angle). Retrolisthesis Widening of the anterior disc Full Extension 4. Motion in the oblique flexion projection: Is restricted. There is gapping of the facet joints at C6-C7 bilaterally and C7-T1 bilaterally. -
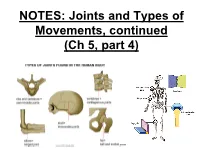
NOTES: Joints and Types of Movements, Continued (Ch 7, Part 4)
NOTES: Joints and Types of Movements, continued (Ch 5, part 4) *Joints are functional junctions between bones. TYPES OF JOINTS **Joints can be classified according to the type of tissue that binds the bones together.** FIBROUS JOINTS: • bones at fibrous joints are tightly joined by a layer of dense connective tissue. • little or no movement occurs at a fibrous joint • Example: the sutures between the flat bones of the skull CARTILAGINOUS JOINTS: • a layer of hyaline cartilage, or fibrocartilage, joins bones of cartilaginous joints • allow limited movement • Example: the joints that separate the vertebrae SYNOVIAL JOINTS: • most joints in the body are synovial joints • allow free movement • bones at synovial joints are covered with hyaline cartilage (“articular cartilage”) and held together by a fibrous JOINT CAPSULE. SYNOVIAL JOINTS: • the joint capsule consists of an outer layer of ligaments and an inner lining of synovial membrane (which secretes synovial fluid to lubricate the joint). • some synovial joints have flattened, shock- absorbing pads of fibrocartilage called MENISCI between the articulating surfaces of the bones SYNOVIAL JOINTS: • some synovial joints may also have BURSAE, which are fluid-filled sacs located between the skin and the underlying bony prominences. • Example: at the knee joint, the patella is sandwiched between 2 bursae. TYPES OF SYNOVIAL JOINTS: • Ball-and-socket - round head of one bone rests within a cup-shaped depression of another - all angular and rotational movements, including circumduction can be performed by this joint TYPES OF SYNOVIAL JOINTS: • Gliding (planar) – Have flattened or slightly curved faces – Flat articular surfaces slide across one another – Amount of movements is slightly TYPES OF SYNOVIAL JOINTS: • Condylar (ellipsoid) – Oval articular face nests within a depression in opposing surface – Angular movements occur in 2 planes: along or across length of oval TYPES OF SYNOVIAL JOINTS: • Hinge – Permits angular motion in single plane (e.g. -

A MODEL of SYNOVIAL FLUID LUBRICANT COMPOSITION in NORMAL and INJURED JOINTS ME Blewis1, GE Nugent-Derfus1, TA Schmidt1, BL Schumacher1, and RL Sah1,2*
MEEuropean Blewis Cells et al .and Materials Vol. 13. 2007 (pages 26-39) DOI: 10.22203/eCM.v013a03 Model of Synovial Fluid Lubricant ISSN Composition 1473-2262 A MODEL OF SYNOVIAL FLUID LUBRICANT COMPOSITION IN NORMAL AND INJURED JOINTS ME Blewis1, GE Nugent-Derfus1, TA Schmidt1, BL Schumacher1, and RL Sah1,2* Departments of 1Bioengineering and 2Whitaker Institute of Biomedical Engineering, University of California-San Diego, La Jolla, CA Abstract Introduction The synovial fluid (SF) of joints normally functions as a The synovial fluid (SF) of natural joints normally biological lubricant, providing low-friction and low-wear functions as a biological lubricant as well as a biochemical properties to articulating cartilage surfaces through the pool through which nutrients and regulatory cytokines putative contributions of proteoglycan 4 (PRG4), traverse. SF contains molecules that provide low-friction hyaluronic acid (HA), and surface active phospholipids and low-wear properties to articulating cartilage surfaces. (SAPL). These lubricants are secreted by chondrocytes in Molecules postulated to play a key role, alone or in articular cartilage and synoviocytes in synovium, and combination, in lubrication are proteoglycan 4 (PRG4) concentrated in the synovial space by the semi-permeable (Swann et al., 1985) present in SF at a concentration of synovial lining. A deficiency in this lubricating system may 0.05-0.35 mg/ml (Schmid et al., 2001a), hyaluronan (HA) contribute to the erosion of articulating cartilage surfaces (Ogston and Stanier, 1953) at 1-4 mg/ml (Mazzucco et in conditions of arthritis. A quantitative intercompartmental al., 2004), and surface-active phospholipids (SAPL) model was developed to predict in vivo SF lubricant (Schwarz and Hills, 1998) at 0.1 mg/ml (Mazzucco et al., concentration in the human knee joint. -

Epithelia Joitns
NAME LOCATION STRUCTURE FUNCTION MOVEMENT Temporomandibular joint Condylar head of ramus of Synovial Diarthrosis Modified hinge joint mandible and glenoid fossa of Rotation and gliding temporal bone Biaxial Zygapophyseal joint Between articular processes of Synovial Diarthrosis Gliding 2 adjacent vertebrae Non axial Atlanto-Occipital joints Atlas and occipital condyle of Synovial Diarthrosis Ellipsoid occipital bone Biaxial Atlantoaxial joints Atlas and axis Synovial Diarthrosis Pivot Uniaxial Joints of vertebral arches Ligaments Fibrous Amphiarthrosis Syndesmoses Intervertebral symphyseal Intervertebral disk between 2 Cartilaginous Amphiarthrosis joints vertebrae Symphysis Costovertebral Head of ribs and body of Synovial Diarthrosis Gliding thoracic vertebra Non axial Costotrasnverse joints Tubercle of rib and transverse Synovial Diarthrosis Gliding process of thoracic vertebra Non axial Lumbosacral Joint Left and right zygopophyseal Laterally Synovial joint Intervertebral symphyseal joint Symphysis SternoclavicularJoint Clavicular notch articulates Synovial Diarthrosis Gliding with medial ends of clavicle Non Axial Manubriosternal Joint Hyaline cartilage junction Cartilaginous Synarthrosis Sternal Angle between manubrium and body Symphysis Xiphisternal Joint Cartilage between xiphoid Synchondrosis Synarthrosis process and body Synostoses Sternocostal Joint (1st) Costocartilage 1 with sternum Cartilaginous Synchondrosis Synarthrosis NAME Location Section Anterior longitudinal runs down anterior surface of vertebral body Vertebral column ligament Posterior longitudinal in canal, runs down posterior surface of vertebral body ligament Interspinous ligament Connects spinous processes Ligamentum flavum Connects laminae ! Intra-articular Disc Between articulating surface of sternum and clavicle Sternoclavicular Joint Costoclavicular ligament 1st rib to clavicle !.