ICRS Heritage Summit 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -

Regeneration of the Epiphysis Including the Articular Cartilage in the Injured Knees of the Lizard Podarcis Muralis
J. Dev. Biol. 2015, 3, 71-89; doi:10.3390/jdb3020071 OPEN ACCESS Journal of Developmental Biology ISSN 2221-3759 www.mdpi.com/journal/jdb/ Article Regeneration of the Epiphysis Including the Articular Cartilage in the Injured Knees of the Lizard Podarcis muralis Lorenzo Alibardi Comparative Histolab and Dipartimento of Bigea, University of Bologna, 40126 Bologna, Italy; E-Mail: [email protected] Academic Editors: Robin C. Muise-Helmericks and Andy Wessels Received: 13 March 2015 / Accepted: 6 May 2015 / Published: 12 May 2015 Abstract: Cartilage regeneration is massive during tail regeneration in lizards but little is known about cartilage regeneration in other body regions of the skeleton. The recovery capability of injured epiphyses of femur and tibia of lizard knees has been studied by histology and 5BrdU immunohistochemistry in lizards kept at high environmental temperatures. Lizard epiphyses contain a secondary ossified center of variable extension surrounded peripherally by an articular cartilage and basally by columns of chondrocytes that form the mataphyseal or growth plate. After injury of the knee epiphyses, a broad degeneration of the articular cartilage during the first days post-injury is present. However a rapid regeneration of cartilaginous tissue is observed from 7 to 14 days post-injury and by 21 days post-lesions, a large part of the epiphyses are reformed by new cartilage. Labeling with 5BrdU indicates that the proliferating cells are derived from both the surface of the articular cartilage and from the metaphyseal plate, two chondrogenic regions that appear proliferating also in normal, uninjured knees. Chondroblasts proliferate by interstitial multiplication forming isogenous groups with only a scant extracellular matrix that later increases. -

Occasional Articles Histology of Normal Haemopoiesis: Bone Marrow
I Clin Pathol 1992;45:645-649 645 Occasional articles Histology of normal haemopoiesis: Bone marrow J Clin Pathol: first published as 10.1136/jcp.45.8.645 on 1 August 1992. Downloaded from histology I B S Wilkins Introduction trabecular spaces,2 but little is known about The bone marrow trephine biopsy specimen the dynamics of blood flow through human holds an unusual position among pathological bone marrow. Arterioles and venules tend to lie specimens. Having been obtained in most towards the centres of intertrabecular spaces. cases by a haematologist, the biopsy specimen They are usually seen in only a small propor- is processed in a histopathology laboratory and tion of intertrabecular spaces in any one biopsy is then reported either by a haematologist or a specimen, suggesting that each may supply or histopathologist, depending on local custom. drain a number of such spaces. Individual practitioners may acquire great skill The trabeculae, arterioles, and venules form in the interpretation of trephine biopsy speci- the structural framework around which mens, but others in both branches ofpathology granulopoiesis develops. Erythropoiesis and are sometimes perplexed when faced with megakaryopoiesis occur in apposition to the tissue appearances for which other experience fine, branching sinusoids. within their individual disciplines may not have prepared them fully. Ideally, interpretation MARROW STROMA should be a collaborative procedure, combin- The trabecular and vascular architecture of ing the clinical and cytological knowledge of medullary bone provides the basic framework, the haematologist with the histopathologist's nutritional supply, and waste removal system skills in analysis ofnormal and abnormal tissue for haemopoiesis, but specialised support of structure. -

Royal Entomological Society
Royal Entomological Society HANDBOOKS FOR THE IDENTIFICATION OF BRITISH INSECTS To purchase current handbooks and to download out-of-print parts visit: http://www.royensoc.co.uk/publications/index.htm This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 2.0 UK: England & Wales License. Copyright © Royal Entomological Society 2012 ROYAL ENTOMOLOGICAL , SOCIETY OF LONDON Vol. I. Part 1 (). HANDBOOKS FOR THE IDENTIFICATION OF BRITISH INSECTS SIPHONAPTERA 13y F. G. A. M. SMIT LONDON Published by the Society and Sold at its Rooms - 41, Queen's Gate, S.W. 7 21st June, I9S7 Price £1 os. od. ACCESSION NUMBER ....... ................... British Entomological & Natural History Society c/o Dinton Pastures Country Park, Davis Street, Hurst, OTS - Reading, Berkshire RG 10 OTH .•' Presented by Date Librarian R EGULATIONS I.- No member shall be allowed to borrow more than five volumes at a time, or to keep any of tbem longer than three months. 2.-A member shall at any time on demand by the Librarian forthwith return any volumes in his possession. 3.-Members damaging, losing, or destroying any book belonging to the Society shall either provide a new copy or pay such sum as tbe Council shall tbink fit. ) "1' > ) I .. ··•• · ·• "V>--· .•. .t ... -;; ·· · ·- ~~- -~· · · ····· · · { · · · l!i JYt.11'ian, ,( i-es; and - REGU--LATIONS dthougll 1.- Books may b - ~dapted, ; ~ 2 -~ . e borrowed at . !.l :: - --- " . ~ o Member shall b . all Meeflfll(s of the So J t Volumes at a time o; ,IJJowed to borrow more c e y . 3.- An y Mem ber r t '. to keep them lonl{er th than three b.ecorn_e SPecified f e a Jn!ng a \'oJume a n one m on th. -

Defining Osteoblast and Adipocyte Lineages in the Bone Marrow
Bone 118 (2019) 2–7 Contents lists available at ScienceDirect Bone journal homepage: www.elsevier.com/locate/bone Full Length Article Defining osteoblast and adipocyte lineages in the bone marrow T ⁎ J.L. Piercea, D.L. Begunb, J.J. Westendorfb,c, M.E. McGee-Lawrencea,d, a Department of Cellular Biology and Anatomy, Medical College of Georgia, Augusta University, Augusta, GA, USA b Department of Orthopedic Surgery, Mayo Clinic, Rochester, MN, USA c Department of Biochemistry and Molecular Biology, Mayo Clinic, Rochester, MN, USA d Department of Orthopaedic Surgery, Augusta University, Augusta, GA, USA ARTICLE INFO ABSTRACT Keywords: Bone is a complex endocrine organ that facilitates structural support, protection to vital organs, sites for he- Bone marrow mesenchymal/stromal cell matopoiesis, and calcium homeostasis. The bone marrow microenvironment is a heterogeneous niche consisting Osteogenesis of multipotent musculoskeletal and hematopoietic progenitors and their derivative terminal cell types. Amongst Osteoblast these progenitors, bone marrow mesenchymal stem/stromal cells (BMSCs) may differentiate into osteogenic, Adipogenesis adipogenic, myogenic, and chondrogenic lineages to support musculoskeletal development as well as tissue Adipocyte homeostasis, regeneration and repair during adulthood. With age, the commitment of BMSCs to osteogenesis Marrow fat Aging slows, bone formation decreases, fracture risk rises, and marrow adiposity increases. An unresolved question is whether osteogenesis and adipogenesis are co-regulated in the bone marrow. Osteogenesis and adipogenesis are controlled by specific signaling mechanisms, circulating cytokines, and transcription factors such as Runx2 and Pparγ, respectively. One hypothesis is that adipogenesis is the default pathway if osteogenic stimuli are absent. However, recent work revealed that Runx2 and Osx1-expressing preosteoblasts form lipid droplets under pa- thological and aging conditions. -
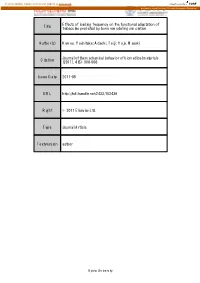
Effects of Loading Frequency on the Functional Adaptation of Title Trabeculae Predicted by Bone Remodeling Simulation
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Kyoto University Research Information Repository Effects of loading frequency on the functional adaptation of Title trabeculae predicted by bone remodeling simulation. Author(s) Kameo, Yoshitaka; Adachi, Taiji; Hojo, Masaki Journal of the mechanical behavior of biomedical materials Citation (2011), 4(6): 900-908 Issue Date 2011-08 URL http://hdl.handle.net/2433/152436 Right © 2011 Elsevier Ltd. Type Journal Article Textversion author Kyoto University Effects of loading frequency on the functional adaptation of trabeculae predicted by bone remodeling simulation Yoshitaka Kameoa, b, Taiji Adachib, c, and Masaki Hojoa a: Department of Mechanical Engineering and Science, Kyoto University b: Computational Cell Biomechanics Team, VCAD System Research Program, RIKEN c: Department of Biomechanics, Institute for Frontier Medical Sciences, Kyoto University Corresponding author: Taiji Adachi, Ph.D. Mailing Address: Department of Biomechanics, Institute for Frontier Medical Sciences, Kyoto University 53, Syogoin-kawaramachi, Sakyo, Kyoto 606-8507, Japan Telephone & Fax: +81 (75) 751-4853 E-mail: [email protected] Submitted to Journal of the Mechanical Behavior of Biomedical Materials Key words: Bone remodeling, Functional adaptation, Loading frequency, Cellular mechanosensing, Computational simulation 1 Abstract The process of bone remodeling is regulated by metabolic activities of many bone cells. While osteoclasts and osteoblasts are responsible for bone resorption and formation, respectively, activities of these cells are believed to be controlled by a mechanosensory system of osteocytes embedded in the extracellular bone matrix. Several experimental and theoretical studies have suggested that the strain-derived interstitial fluid flow in lacuno-canalicular porosity serves as the prime mover for bone remodeling. -

Small Leucine Rich Proteoglycans, a Novel Link to Osteoclastogenesis Vardit Kram1, Tina M
www.nature.com/scientificreports OPEN Small leucine rich proteoglycans, a novel link to osteoclastogenesis Vardit Kram1, Tina M. Kilts1, Nisan Bhattacharyya2, Li Li1 & Marian F. Young1 Biglycan (Bgn) and Fibromodulin (Fmod) are subtypes of the small leucine-rich family of proteoglycans Received: 1 February 2017 (SLRP). In this study we examined the skeletal phenotype of BgnFmod double knockout (BgnFmod KO) Accepted: 13 September 2017 mice and found they were smaller in size and have markedly reduced bone mass compared to WT. The Published: xx xx xxxx low bone mass (LBM) phenotype is the result of both the osteoblasts and osteoclasts from BgnFmod KO mice having higher diferentiation potential and being more active compared to WT mice. Using multiple approaches, we showed that both Bgn and Fmod directly bind TNFα as well as RANKL in a dose dependent manner and that despite expressing higher levels of both TNFα and RANKL, BgnFmod KO derived osteoblasts cannot retain these cytokines in the vicinity of the cells, which leads to elevated TNFα and RANKL signaling and enhanced osteoclastogenesis. Furthermore, adding either Bgn or Fmod to osteoclast precursor cultures signifcantly attenuated the cells ability to form TRAP positive, multinucleated giant cells. In summary, our data indicates that Bgn and Fmod expressed by the bone forming cells, are novel coupling ECM components that control bone mass through sequestration of TNFα and/or RANKL, thereby adjusting their bioavailability in order to regulate osteoclastogenesis. As life expectancy continues to rise, the burden of age-related diseases is expected to increase. One such age-related disease is osteoporosis. Te skeleton is a dynamic tissue undergoing continuous remodeling - old bone is being resorbed by osteoclasts and new bone is laid down by osteoblasts- at multiple foci at the same time. -

Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-Tailed Opossum (Monodelphis Domestica) and North American Opossum (Didelphis Virginiana)
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 12-2001 Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana) Lee Anne Cope University of Tennessee - Knoxville Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Animal Sciences Commons Recommended Citation Cope, Lee Anne, "Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana). " PhD diss., University of Tennessee, 2001. https://trace.tennessee.edu/utk_graddiss/2046 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Lee Anne Cope entitled "Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana)." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Doctor of Philosophy, with a major in Animal Science. Robert W. Henry, Major Professor We have read this dissertation and recommend its acceptance: Dr. R.B. Reed, Dr. C. Mendis-Handagama, Dr. J. Schumacher, Dr. S.E. Orosz Accepted for the Council: Carolyn R. -

Eif2α Signaling Regulates Autophagy of Osteoblasts and the Development of Osteoclasts in OVX Mice
Li et al. Cell Death and Disease (2019) 10:921 https://doi.org/10.1038/s41419-019-2159-z Cell Death & Disease ARTICLE Open Access eIF2α signaling regulates autophagy of osteoblasts and the development of osteoclasts in OVX mice Jie Li1,2, Xinle Li1,2,DaquanLiu1,2, Kazunori Hamamura3, Qiaoqiao Wan3,SungsooNa3, Hiroki Yokota3 and Ping Zhang1,2,3,4 Abstract Bone loss in postmenopausal osteoporosis is induced chiefly by an imbalance of bone-forming osteoblasts and bone- resorbing osteoclasts. Salubrinal is a synthetic compound that inhibits de-phosphorylation of eukaryotic translation initiation factor 2 alpha (eIF2α). Phosphorylation of eIF2α alleviates endoplasmic reticulum (ER) stress, which may activate autophagy. We hypothesized that eIF2α signaling regulates bone homeostasis by promoting autophagy in osteoblasts and inhibiting osteoclast development. To test the hypothesis, we employed salubrinal to elevate the phosphorylation of eIF2α in an ovariectomized (OVX) mouse model and cell cultures. In the OVX model, salubrinal prevented abnormal expansion of rough ER and decreased the number of acidic vesiculars. It regulated ER stress- associated signaling molecules such as Bip, p-eIF2α, ATF4 and CHOP, and promoted autophagy of osteoblasts via regulation of eIF2α, Atg7, LC3, and p62. Salubrinal markedly alleviated OVX-induced symptoms such as reduction of bone mineral density and bone volume fraction. In primary bone-marrow-derived cells, salubrinal increased the differentiation of osteoblasts, and decreased the formation of osteoclasts by inhibiting nuclear factor of activated T-cells cytoplasmic 1 (NFATc1). Live cell imaging and RNA interference demonstrated that suppression of osteoclastogenesis is in part mediated by Rac1 GTPase. Collectively, this study demonstrates that ER stress-autophagy axis plays an important role in OVX mice. -

Ex Vivo Systems to Study Chondrogenic Differentiation and Cartilage Integration
Journal of Functional Morphology and Kinesiology Review Ex Vivo Systems to Study Chondrogenic Differentiation and Cartilage Integration Graziana Monaco 1,2, Alicia J. El Haj 2,3, Mauro Alini 1 and Martin J. Stoddart 1,2,* 1 AO Research Institute Davos, Clavadelerstrasse 8, CH-7270 Davos Platz, Switzerland; [email protected] (G.M.); [email protected] (M.A.) 2 School of Pharmacy & Bioengineering Research, University of Keele, Keele ST5 5BG, UK; [email protected] 3 Healthcare Technology Institute, Translational Medicine, School of Chemical Engineering, University of Birmingham, Birmingham B15 2TH, UK * Correspondence: [email protected]; Tel.: +41-81-414-2448 Abstract: Articular cartilage injury and repair is an issue of growing importance. Although common, defects of articular cartilage present a unique clinical challenge due to its poor self-healing capacity, which is largely due to its avascular nature. There is a critical need to better study and understand cellular healing mechanisms to achieve more effective therapies for cartilage regeneration. This article aims to describe the key features of cartilage which is being modelled using tissue engineered cartilage constructs and ex vivo systems. These models have been used to investigate chondrogenic differentiation and to study the mechanisms of cartilage integration into the surrounding tissue. The review highlights the key regeneration principles of articular cartilage repair in healthy and diseased joints. Using co-culture models and novel bioreactor designs, the basis of regeneration is aligned with recent efforts for optimal therapeutic interventions. Keywords: bioreactors; osteochondral; integration; tissue engineering Citation: Monaco, G.; El Haj, A.J.; Alini, M.; Stoddart, M.J. -

CKD: Bone Mineral Metabolism Peter Birks, Nephrology Fellow
CKD: Bone Mineral Metabolism Peter Birks, Nephrology Fellow CKD - KDIGO Definition and Classification of CKD ◦ CKD: abnormalities of kidney structure/function for > 3 months with health implications ≥1 marker of kidney damage: ACR ≥30 mg/g Urine sediment abnormalities Electrolyte and other abnormalities due to tubular disorders Abnormalities detected by histology Structural abnormalities (imaging) History of kidney transplant OR GFR < 60 Parathyroid glands 4 glands behind thyroid in front of neck Parathyroid physiology Parathyroid hormone Normal circumstances PTH: ◦ Increases calcium ◦ Lowers PO4 (the renal excretion outweighs the bone release and gut absorption) ◦ Increases Vitamin D Controlled by feedback ◦ Low Ca and high PO4 increase PTH ◦ High Ca and low PO4 decrease PTH In renal disease: Gets all messed up! Decreased phosphate clearance: High Po4 Low 1,25 OH vitamin D = Low Ca Phosphate binds calcium = Low Ca Low calcium, high phosphate, and low VitD all feedback to cause more PTH release This is referred to as secondary hyperparathyroidism Usually not seen until GFR < 45 Who cares Chronically high PTH ◦ High bone turnover = renal osteodystrophy Osteoporosis/fractures Osteomalacia Osteitis fibrosa cystica High phosphate ◦ Associated with faster progression CKD ◦ Associated with higher mortality Calcium-phosphate precipitation ◦ Soft tissue, blood vessels (eg: coronary arteries) Low 1,25 OH-VitD ◦ Immune status, cardiac health? KDIGO KDIGO: Kidney Disease Improving Global Outcomes Most recent update regarding -

The Challenge of Articular Cartilage Repair
Doctoral Program of Clinical Research Faculty of Medicine University of Helsinki Finland THE CHALLENGE OF ARTICULAR CARTILAGE REPAIR STUDIES ON CARTILAGE REPAIR IN ANIMAL MODELS AND IN CELL CULTURE Eve Salonius ACADEMIC DISSERTATION To be presented, with the permission of the Faculty of Medicine of the University of Helsinki, for public examination in lecture room PIII, Porthania, Yliopistonkatu 3, on Friday the 22nd of November, 2019 at 12 o’clock. Helsinki 2019 Supervisors: Professor Ilkka Kiviranta, M.D., Ph.D. Department of Orthopaedics and Traumatology Clinicum Faculty of Medicine University of Helsinki Finland Virpi Muhonen, Ph.D. Department of Orthopaedics and Traumatology Clinicum Faculty of Medicine University of Helsinki Finland Reviewers: Professor Heimo Ylänen, Ph.D. Department of Electronics and Communications Engineering Tampere University of Technology Finland Adjunct Professor Petri Virolainen, M.D., Ph.D. Department of Orthopaedics and Traumatology University of Turku Finland Opponent: Professor Leif Dahlberg, M.D., Ph.D. Department of Orthopaedics Lund University Sweden The Faculty of Medicine uses the Urkund system (plagiarism recognition) to examine all doctoral dissertations © Eve Salonius 2019 ISBN 978-951-51-5613-6 (paperback) ISBN 978-951-51-5614-3 (PDF) Unigrafia Helsinki 2019 ABSTRACT Articular cartilage is highly specialized connective tissue that covers the ends of bones in joints. Damage to articulating joint surface causes pain and loss of joint function. The prevalence of cartilage defects is expected to increase, and if untreated, they may lead to premature osteoarthritis, the world’s leading joint disease. Early intervention may cease this process. The first-line treatment of non-surgical management of articular cartilage defects is physiotherapy and pain medication to alleviate symptoms.