Application of Biodegradable PLGA-PEG-PLGA/CPC Composite Bone Cement in the Treatment of Osteoporosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -

ICRS Heritage Summit 1
ICRS Heritage Summit 1 20th Anniversary www.cartilage.org of the ICRS ICRS Heritage Summit June 29 – July 01, 2017 Gothia Towers, Gothenburg, Sweden Final Programme & Abstract Book #ICRSSUMMIT www.cartilage.org Picture Copyright: Zürich Tourismus 2 The one-step procedure for the treatment of chondral and osteochondral lesions Aesculap Biologics Facing a New Frontier in Cartilage Repair Visit Anika at Booth #16 Easy and fast to be applied via arthroscopy. Fixation is not required in most cases. The only entirely hyaluronic acid-based scaffold supporting hyaline-like cartilage regeneration Biologic approaches to tissue repair and regeneration represent the future in healthcare worldwide. Available Sizes Aesculap Biologics is leading the way. 2x2 cm Learn more at www.aesculapbiologics.com 5x5 cm NEW SIZE Aesculap Biologics, LLC | 866-229-3002 | www.aesculapusa.com Aesculap Biologics, LLC - a B. Braun company Website: http://hyalofast.anikatherapeutics.com E-mail: [email protected] Telephone: +39 (0)49 295 8324 ICRS Heritage Summit 3 The one-step procedure for the treatment of chondral and osteochondral lesions Visit Anika at Booth #16 Easy and fast to be applied via arthroscopy. Fixation is not required in most cases. The only entirely hyaluronic acid-based scaffold supporting hyaline-like cartilage regeneration Available Sizes 2x2 cm 5x5 cm NEW SIZE Website: http://hyalofast.anikatherapeutics.com E-mail: [email protected] Telephone: +39 (0)49 295 8324 4 Level 1 Study Proves Efficacy of ACP in -

Occasional Articles Histology of Normal Haemopoiesis: Bone Marrow
I Clin Pathol 1992;45:645-649 645 Occasional articles Histology of normal haemopoiesis: Bone marrow J Clin Pathol: first published as 10.1136/jcp.45.8.645 on 1 August 1992. Downloaded from histology I B S Wilkins Introduction trabecular spaces,2 but little is known about The bone marrow trephine biopsy specimen the dynamics of blood flow through human holds an unusual position among pathological bone marrow. Arterioles and venules tend to lie specimens. Having been obtained in most towards the centres of intertrabecular spaces. cases by a haematologist, the biopsy specimen They are usually seen in only a small propor- is processed in a histopathology laboratory and tion of intertrabecular spaces in any one biopsy is then reported either by a haematologist or a specimen, suggesting that each may supply or histopathologist, depending on local custom. drain a number of such spaces. Individual practitioners may acquire great skill The trabeculae, arterioles, and venules form in the interpretation of trephine biopsy speci- the structural framework around which mens, but others in both branches ofpathology granulopoiesis develops. Erythropoiesis and are sometimes perplexed when faced with megakaryopoiesis occur in apposition to the tissue appearances for which other experience fine, branching sinusoids. within their individual disciplines may not have prepared them fully. Ideally, interpretation MARROW STROMA should be a collaborative procedure, combin- The trabecular and vascular architecture of ing the clinical and cytological knowledge of medullary bone provides the basic framework, the haematologist with the histopathologist's nutritional supply, and waste removal system skills in analysis ofnormal and abnormal tissue for haemopoiesis, but specialised support of structure. -

Royal Entomological Society
Royal Entomological Society HANDBOOKS FOR THE IDENTIFICATION OF BRITISH INSECTS To purchase current handbooks and to download out-of-print parts visit: http://www.royensoc.co.uk/publications/index.htm This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 2.0 UK: England & Wales License. Copyright © Royal Entomological Society 2012 ROYAL ENTOMOLOGICAL , SOCIETY OF LONDON Vol. I. Part 1 (). HANDBOOKS FOR THE IDENTIFICATION OF BRITISH INSECTS SIPHONAPTERA 13y F. G. A. M. SMIT LONDON Published by the Society and Sold at its Rooms - 41, Queen's Gate, S.W. 7 21st June, I9S7 Price £1 os. od. ACCESSION NUMBER ....... ................... British Entomological & Natural History Society c/o Dinton Pastures Country Park, Davis Street, Hurst, OTS - Reading, Berkshire RG 10 OTH .•' Presented by Date Librarian R EGULATIONS I.- No member shall be allowed to borrow more than five volumes at a time, or to keep any of tbem longer than three months. 2.-A member shall at any time on demand by the Librarian forthwith return any volumes in his possession. 3.-Members damaging, losing, or destroying any book belonging to the Society shall either provide a new copy or pay such sum as tbe Council shall tbink fit. ) "1' > ) I .. ··•• · ·• "V>--· .•. .t ... -;; ·· · ·- ~~- -~· · · ····· · · { · · · l!i JYt.11'ian, ,( i-es; and - REGU--LATIONS dthougll 1.- Books may b - ~dapted, ; ~ 2 -~ . e borrowed at . !.l :: - --- " . ~ o Member shall b . all Meeflfll(s of the So J t Volumes at a time o; ,IJJowed to borrow more c e y . 3.- An y Mem ber r t '. to keep them lonl{er th than three b.ecorn_e SPecified f e a Jn!ng a \'oJume a n one m on th. -
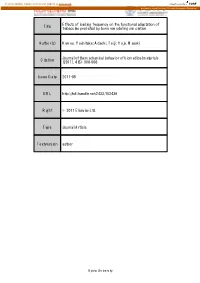
Effects of Loading Frequency on the Functional Adaptation of Title Trabeculae Predicted by Bone Remodeling Simulation
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Kyoto University Research Information Repository Effects of loading frequency on the functional adaptation of Title trabeculae predicted by bone remodeling simulation. Author(s) Kameo, Yoshitaka; Adachi, Taiji; Hojo, Masaki Journal of the mechanical behavior of biomedical materials Citation (2011), 4(6): 900-908 Issue Date 2011-08 URL http://hdl.handle.net/2433/152436 Right © 2011 Elsevier Ltd. Type Journal Article Textversion author Kyoto University Effects of loading frequency on the functional adaptation of trabeculae predicted by bone remodeling simulation Yoshitaka Kameoa, b, Taiji Adachib, c, and Masaki Hojoa a: Department of Mechanical Engineering and Science, Kyoto University b: Computational Cell Biomechanics Team, VCAD System Research Program, RIKEN c: Department of Biomechanics, Institute for Frontier Medical Sciences, Kyoto University Corresponding author: Taiji Adachi, Ph.D. Mailing Address: Department of Biomechanics, Institute for Frontier Medical Sciences, Kyoto University 53, Syogoin-kawaramachi, Sakyo, Kyoto 606-8507, Japan Telephone & Fax: +81 (75) 751-4853 E-mail: [email protected] Submitted to Journal of the Mechanical Behavior of Biomedical Materials Key words: Bone remodeling, Functional adaptation, Loading frequency, Cellular mechanosensing, Computational simulation 1 Abstract The process of bone remodeling is regulated by metabolic activities of many bone cells. While osteoclasts and osteoblasts are responsible for bone resorption and formation, respectively, activities of these cells are believed to be controlled by a mechanosensory system of osteocytes embedded in the extracellular bone matrix. Several experimental and theoretical studies have suggested that the strain-derived interstitial fluid flow in lacuno-canalicular porosity serves as the prime mover for bone remodeling. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Download File
Cartilage Development and Maturation In Vitro and In Vivo Johnathan Ng Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences Columbia University 2017 © 2017 Johnathan Ng All rights reserved Abstract Cartilage Development and Maturation In Vitro and In Vivo Johnathan Ng The articular cartilage has a limited capacity to regenerate. Cartilage lesions often result in degeneration, leading to osteoarthritis. Current treatments are mostly palliative and reparative, and fail to restore cartilage function in the long term due to the replacement of hyaline cartilage with fibrocartilage. Although a stem-cell based approach towards regenerating the articular cartilage is attractive, cartilage generated from human mesenchymal stem cells (hMSCs) often lack the function, organization and stability of the native cartilage. Thus, there is a need to develop effective methods to engineer physiologic cartilage tissues from hMSCs in vitro and assess their outcomes in vivo. This dissertation focused on three coordinated aims: establish a simple in vivo model for studying the maturation of osteochondral tissues by showing that subcutaneous implantation in a mouse recapitulates native endochondral ossification (Aim 1), (ii) develop a robust method for engineering physiologic cartilage discs from self-assembling hMSCs (Aim 2), and (iii) improve the organization and stability of cartilage discs by implementing spatiotemporal control during induction in vitro (Aim 3). First, the usefulness of subcutaneous implantation in mice for studying the development and maintenance of osteochondral tissues in vivo was determined. By studying juvenile bovine osteochondral tissues, similarities in the profiles of endochondral ossification between the native and ectopic processes were observed. -

First Case of Plasma Cell Myeloma with Brown Tumor Features Unrelated to Hyperparathyroidism
Letter to the Editor Diagnostic Hematology CROSSMARK_logo_3_Test 1 / 1 Ann Lab Med 2019;39:96-98 https://doi.org/10.3343/alm.2019.39.1.96 ISSN 2234-3806 • eISSN 2234-3814 https://crossmark-cdn.crossref.org/widget/v2.0/logos/CROSSMARK_Color_square.svg 2017-03-16 First Case of Plasma Cell Myeloma With Brown Tumor Features Unrelated to Hyperparathyroidism Heyjin Kim, M.D.1, Kihyun Kim, M.D.2, Sung Ran Cho, M.D.3, Hee-Jin Kim, M.D.1, and Sun-Hee Kim , M.D.1 Departments of 1Laboratory Medicine and Genetics and 2Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea; 3Department of Laboratory Medicine, Ajou University Hospital of School of Medicine, Suwon, Korea Dear Editor, in some PCM cases [1], there has been only one report so far of Plasma cell myeloma (PCM) is multifocal neoplastic proliferation a PCM patient with brown tumor features and severe osteoclas- of plasma cells originating from the bone marrow (BM) and tic activity in BM, associated with secondary hyperparathyroid- damaging other organs by production of a monoclonal protein ism in response to drug-induced hypocalcemia, and exhibiting (M protein) in the serum and/or urine [1]. PCM is diagnosed serological complete response (CR) [9]. We report the first case based on comprehensive clinical, morphological, immunologi- of PCM with brown tumor features unrelated to hyperparathy- cal, and radiological evidence [1]. PCM-related end-organ dam- roidism. age typically includes hypercalcemia, renal insufficiency, ane- A 50-year-old female presented with right pleuritic chest pain, mia, and bone lesions (CRAB criteria) [1]. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -

Bone Cartilage Dense Fibrous CT (Tendons & Nonelastic Ligaments) Dense Elastic CT (Elastic Ligaments)
Chapter 6 Content Review Questions 1-8 1. The skeletal system consists of what connective tissues? Bone Cartilage Dense fibrous CT (tendons & nonelastic ligaments) Dense elastic CT (elastic ligaments) List the functions of these tissues. Bone: supports the body, protects internal organs, provides levers on which muscles act, store minerals, and produce blood cells. Cartilage provides a model for bone formation and growth, provides a smooth cushion between adjacent bones, and provides firm, flexible support. Tendons attach muscles to bones and ligaments attach bone to bone. 2. Name the major types of fibers and molecules found in the extracellular matrix of the skeletal system. Collagen Proteoglycans Hydroxyapatite Water Minerals How do they contribute to the functions of tendons, ligaments, cartilage and bones? The collagen fibers of tendons and ligaments make these structures very tough, like ropes or cables. Collagen makes cartilage tough, whereas the water-filled proteoglycans make it smooth and resistant. As a result, cartilage is relatively rigid, but springs back to its original shape if it is bent or slightly compressed, and it is an excellent shock absorber. The extracellular matrix of bone contains collagen and minerals, including calcium and phosphate. Collagen is a tough, ropelike protein, which lends flexible strength to the bone. The mineral component gives the bone compression (weight-bearing) strength. Most of the mineral in the bone is in the form of hydroxyapatite. 3. Define the terms diaphysis, epiphysis, epiphyseal plate, medullary cavity, articular cartilage, periosteum, and endosteum. Diaphysis – the central shaft of a long bone. Epiphysis – the ends of a long bone. Epiphyseal plate – the site of growth in bone length, found between each epiphysis and diaphysis of a long bone and composed of cartilage. -

Trabecular Bone
Lectures 10-11, T-bone Notes/Slides, 3.054 Trabecular bone • Foam-like structure • Exists at ends of long bones — ends have longer surface area than shafts to reduce stress on cartilage at joints; trabecular bone reduces weight • Also exists in skull, iliac crest (pelvis) — forms sandwich structure — reduces weight • Also makes up core of vertebrae • Trabecular bone of interest: (1) osteoporosis (2) osteoarthritis (3) joint replacement Osteoporosis • Bone mass decreases with age; osteoporosis — extreme bone loss • Most common fractures: hip (proximal femur) vertebrae • At both sites, most of load carried by trabecular bone • Hip fractures especially serious: 40% of elderly patients (>65 years old) die within a year (often due to loss of mobility — pneumonia) • 300,000 hip fractures/year in US • Costs $17 billion in 2005 1 Trabecular bone Gibson, L. J., and M. F. Ashby. Cellular Solids: Structure and Properties. 2nd ed. Cambridge University Press, © 1997. Figures courtesy of Lorna Gibson and Cambridge University Press. 2 Osteo arthritis • Degradation of cartilage at joints • Stress on cartilage affected by moduli of underlying bone • Cortical bone shell can be thin (e.g. < 1mm) • Mechanical properties of trabecular bone can affect stress distribution on cartilage Joint replacement • If osteoarthritis bad and significant damage to cartilage, may require joint replacement • Cut end of bone off and insert stem of metal replacement into hollow of long section of bone • Metals used: titanium, cobalt-chromium, stainless steel • Bone grows in response to loads on it Trabecular bone: density depends on magnitude of σ orientation depends on direction of principal stresses 3 • Mismatch in moduli between metal and bone leads to stress shielding E(GPa) E(GPa) Co - 28Cr - Mo 210 Cortical bone 18 Ti alloys 110 Trab. -

View of the Micro-CT Data, Where the Blue and Green Marked the Spongy Structure Caused by the Cancellous Bone
Liu et al. EURASIP Journal on Image and Video EURASIP Journal on Image Processing (2019) 2019:60 https://doi.org/10.1186/s13640-019-0456-1 and Video Processing RESEARCH Open Access Mice endplate segmentation from micro-CT data through graph-based trabecula recognition Shi-Jian Liu1†, Zheng Zou2†, Jeng-Shyang Pan1,3,4* and Sheng-Hui Liao5 Abstract Though segmentation of spinal column from medical images have been intensively studied for decade, most of the works were concentrated on the segmentation of the vertebral body and arch, instead of the endplate. Recently, the increasing study on degeneration analysis of vertebra and intervertebral disc (IVD) make endplate segmentation as important as others. While the accurately segmentation of mice endplate from micro computed tomography (CT) images is challenging. The major difficulties include potential high system payload and poor run-time efficiency resulting from high-resolution micro-CT data, highly complicated and variable shape of the vertebra tissues, and the ambiguous segmentation boundary due to the similarity of spongy structures inside both the endplate and its adjacent vertebral body. To solve the problems, the core idea of the proposed method is to identify trabeculae between the endplate and the body through a graph-based strategy. In addition, in order to reduce the data complexity, an endplate-targeted region of interest (ROI) extraction method is introduced according to the analysis of spatial relationship and variety of bone density of vertebra. Furthermore, shape priori of endplate in both two-dimensional and three-dimensional are extracted to assist in the segmentation. Finally, an iterative cutting procedure is implemented to produce the final result.