Checklist of Required Tasks for the Rotation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

APPENDIX of DICTATION TEMPLATES Undergraduate Medical Education Approved By: Clerkship & Electives Commi
APPENDIX OF DICTATION TEMPLATES Undergraduate Medical Education Approved by: Clerkship & Electives Committee Date of original approval: August, 2013 Date of last review: N/A Date of next scheduled review: August, 2014 I. PURPOSE The following dictation samples are included to provide clinical clerks with guidance. II. DEFINITIONS CTU Clinical Teaching Unit MRP Most Responsible Physician PCCU Paediatric Critical Care Unit III. APPENDIX CTU - Discharge Summary Dictation Template All patients who 1) were admitted for seven or more days, and/or 2) had been admitted to the PCCU (Paediatric Critical Care Unit), and/or 3) had a complex condition or complicated course in hospital require a dictated (or typed) discharge summary. 1. Required initial information: Your name and position, most responsible physician (MRP) on the day of discharge, patient’s first and last name, PIN, who should receive this discharge summary (the MRP, the referring physician if one is known, the paediatrician or family physician of the patient (if not the referring physician), and other consultants who are going to see the patient in follow-up. Example: “This is John Smith, clinical clerk for Dr. X, dictating on patient Getme Outofhere, PIN 00000000. Please forward copies to Dr. X, Victoria Hospital, Dr. Y, family physician in London, Dr. Z, Paediatrician in London.” 2. Most responsible diagnosis: Diagnosis primarily responsible for the patient’s current admission. 3. History of present illness: Essential history of chief complaint as given by patient and/or care providers. It should include a concise summary of the relevant information from the time the symptoms started and up to the arrival at the Emergency Department. -

Musculoskeletal Diagnosis Utilizing History and Physical Examination: Focus on Spine
NYU Long Island School of Medicine MUSCULOSKELETAL DIAGNOSIS UTILIZING HISTORY AND PHYSICAL EXAMINATION: FOCUS ON SPINE Ralph K. Della Ratta, MD, FACP Kevin J. Curley, MD, FACP Division of General Internal Medicine, NYU Winthrop Hospital NYU Long Island School of Medicine, SUNY Stony Brook School of Medicine Board Certified in IM and Primary Care Sports Medicine Learning Objectives 1. Identify components of the focused history and physical examination that will guide musculoskeletal diagnosis 2. Utilize musculoskeletal examination provocative maneuvers to aide differential diagnosis 3. Review the evidence base (likelihood ratios etc.) that is known about musculoskeletal physical examination 2 NYU Long Island School of Medicine * ¾ of medical diagnoses are still made on history and exam despite technological Musculoskeletal Physical Exam advances of modern medicine • Physical examination is key to musculoskeletal diagnosis • Unlike many other organ systems, the diagnostic standard for many musculoskeletal disorders is the exam finding (e.g. diagnosis of epicondylitis, see below) • “You may think you have not seen it, but it has seen you!” Lateral Epicondylitis confirmed on exam by reproducing pain at lateral epicondyle with resisted dorsiflexion at wrist **not diagnosed with imaging** 3 NYU Long Island School of Medicine Musculoskeletal Physical Exam 1. Inspection – symmetry, swelling, redness, deformity 2. Palpation – warmth, tenderness, crepitus, swelling 3. Range of motion *most sensitive for joint disease Bates Pocket Guide to Physical -

EPA Quick Reference Guide
EPA Quick Reference Guide EPAs 1 & 2 – Professionalism Unacceptable • Unreliable • Dishonest • Avoids responsibility • Commitment uncertain • Dresses inappropriately • Unexplained absences • Verbal and non-verbal disrespect towards preceptor • Does not recognize own limitations and the need to seek assistance • Unable to comprehend the point of view and emotional state of other people • Judgmental of others • Fails to recognize and respect cross-cultural and gender differences Minimally Competent • Sometimes late • Not consistently able to complete assignments or tasks • Not consistently considerate of the feelings and emotional needs of others • Sometimes judgmental Competent • Punctual • Dependable • Accepts responsibilities • Demonstrates a willingness to accept feedback regarding necessary change(s) • Appropriately shows concern for others’ feelings and interacts accordingly • Recognizes and respects cross-cultural and gender differences Office of Medical Education 306 Liberty View Lane, Lynchburg, Va. 24502 [email protected] EPAs 3 & 4 – Data Gathering / Interviewing & Physical Examination Skills Unacceptable • Inefficient, disorganized • Weak prioritization skills • Misses major findings • Fails to appreciate physical findings and pertinent information • History and/or physical exam incomplete or inaccurate • Insufficient attention to psychosocial issues • Needs to work on establishing rapport with patients • Needs to work on awareness of appropriate boundaries with patients • Needs to improve demonstration of compassion • -
Clinical Reasoning - the Process of Thinking and Decision Making, Consciously & Unconsciously Guide Practice Actions
Diagnostic Reasoning “DR” Toolbox for Hospitalist Faculty Heather Hofmann, MD Department of Medicine 2017-18 2 Goal Increase faculty familiarity with diagnostic reasoning principles and tools so as to improve its teaching. Three Parts: I: Introduction to Diagnostic Reasoning II: DR Toolbox III: Structured Reflection Exercise (SRE) 4 Part I: Introduction to Diagnostic Reasoning Learning Objectives - Understand the “what” and “why” of Diagnostic Reasoning - Recognize dual-process theory’s role in “how” we reason 6 What is Diagnostic Reasoning? - Clinical reasoning - The process of thinking and decision making, consciously & unconsciously guide practice actions 25yo female G1P0, 2m gestation returns from Rio. - Diagnostic reasoning: - The process of collecting & analyzing information establish a diagnosis chest pain STEMI in proximal LAD abdominal pain acute appendicitis 7 Why teach diagnostic reasoning? - Incorrect diagnoses are often at the root of medical errors - DR is a means to apply basic science to clinical problems - Central to being a physician 8 Patient’s perspective What’s wrong with me? Is it bad? What can we do about it? 9 Why now? Never too early for practice 10 From Novice to Expert 11 How do we reason? Information processing theory 12 How do we reason? Information processing theory: Dual process theory. Analytical Non-analytical Conscious Unconscious Type/System 2 Type/System 1 Slow Fast Effortful Automatic Deliberative Involuntary Logical Emotional Requires attention, Executes skilled self-control, time. response and -
Adm Notepreophp
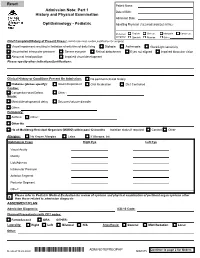
Patient Name: Admission Note: Part 1 Date of Birth: History and Physical Examination Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: Chief Complaint/History of Present Illness: (admit note must contain justification for surgery) Visual impairment resulting in limitation of activities of daily living Diplopia Asthenopia Glare/Light sensitivity Uncontrolled intraocular pressure Severe eye pain Retinal detachment Eyes not aligned Impaired binocular vision Abnormal head position Impaired visual development Please specify other indications/justifications: Clinical History or Conditions Present On Admission: No pertinent clinical history Diabetes (please specify): Insulin Dependent Oral Medication Diet Controlled Cardiac: Congenital Heart Defect Other : Neuro: Mental/developmental delay Seizures/seizure disorder Other: Pulmonary: Asthma Other : Other Hx: Hx of Multidrug-Resistant Organism (MDRO) within past 12 months Isolation status if required: Contact Other Allergies: No Known Allergies Latex If Allergies, list: Ophthalmic Exam Right Eye Left Eye Visual Acuity Motility Lids/Adnexa Intraocular Pressure Anterior Segment Posterior Segment Other: Please refer to Pediatric Medical Evaluation for review of systems and physical examination of pertinent organ systems other X than those related to admission diagnosis ASSESMENT/PLAN Admission Diagnosis: ICD-10 Code: Planned Procedure(s) with CPT codes: FemtoSecond ORA OTHER: Laterality: Right Left Bilateral N/A Anesthesia: General MAC/Sedation Local Other: Continue to page 2 for Orders Revised 10.22.2020 *ADM NOTEPREOPHP* ADM NOTEPREOPHP ADM.075 Patient Name: Admission Note: Part 2 History and Physical Examination Date of Birth: Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: 1. -

General Rules of the Marquette General Health System Medical Staff
General Rules of the Marquette General Health System Medical Staff I. PATIENT ADMISSION, ALTERNATE COVERAGE, TRANSFER, DISCHARGE AND DEATH 1.1 ADMISSION CRITERIA 1.1-1 Who may admit patients. Only a Member with admitting privileges may admit or co-admit a patient to the Hospital. Except as provided for Qualified Oral Surgeons, Podiatrists and Independent Allied Health Professionals in the Medical Staff Bylaws, a physician Member will be responsible for the general medical care and treatment of every patient admitted to the Hospital. Medical care may be provided by a Resident, other specified professional personnel or Allied Health Staff members provided they are working under the supervision of a Practitioner with clinical privileges. Medical care will be provided only by Members and Hospital support staff authorized to perform such services. 1.1-2 Admission Information. An admitting Practitioner will provide the following information in the patient’s medical record, if such information is available to the admitting Practitioner: (a) Provisional diagnosis. (b) A valid reason for admitting the patient, including information to support the medical necessity and the appropriateness of the admission. (c) Information needed to properly care for the patient being admitted. (d) Information needed to protect the patient from himself/herself. (e) Information needed to protect Hospital personnel and others from potential problems or dangers presented by the patient. (f) Information deemed necessary by the Hospital. 1.1-3 Admission of potentially suicidal or dangerous patients. If an admitting Practitioner reasonably believes a patient admitted for other purposes is potentially suicidal or dangerous to himself/herself or others, the admitting Practitioner will promptly obtain a consultation from a suitable mental health professional. -
Diagnosis and Management of Chlamydia: a Guide for Gps
■ PRESCRIBING IN PRACTICE Diagnosis and management of chlamydia: a guide for GPs ELEANOR DRAEGER SPL Chlamydia is a common sexually- transmitted infection caused by Chlamydia trachomatis bacteria. This article discusses its diagnosis and treatment, and considers the GP’s role in management. hlamydia is the most common sexually-transmitted infection C(STI) in the UK, with 203,116 new diagnoses in England in 2017, of which 126,828 (62%) were in young people aged 15–24 years.1 Chlamydia is transmitted primarily through penetrative sex and infects the urethra and endocervix. It can also infect the throat and the rectum, and in some cases the conjunctiva. It is very infectious, with a concordance of up to 75% between sexual partners. There are many risk factors for chlamydia infection, including being under the age of 25 years, having a new sexual partner and inconsistent use of condoms. If a woman contracts chlamydia during pregnancy it can be transmitted to the baby at delivery, causing conjunctivitis or pneumonia. Classification of chlamydia infections There are three species of chlamydia bacteria that can cause disease in humans: • Chlamydia psittaci – the natural host is birds, especially par- rots, but it can be transmitted to humans, causing psittacosis • Chlamydia pneumoniae – causes respiratory disease in humans • Chlamydia trachomatis – several different serovars can cause disease (including STIs) in humans, as detailed in Figure 1. Symptoms The majority of genital chlamydia infections are asymptomatic, but they can cause significant symptoms. In women, chlamydia can cause vaginal discharge, dysuria, abdominal and pelvic pain, post-coital and intermenstrual bleeding, and deep dys- pareunia. -
Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents
U.S. DEPARTMENT OF VETERANS AFFAIRS Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents “Supervising Practitioner” (synonymous with “Attending”): Responsible for all care in which interns, residents or fellows are involved. “Resident” is used to apply to physician, dentist, optometrist, and podiatrist residents and fellows, regardless of training level. Documentation of all patient encounters must identify the supervising practitioner (attending) by name and indicate the level of involvement. Depending upon the clinical situation, Four types of documentation of resident supervision are allowed: 1. Attending’s progress note or other entry into the patient health record. 2. Attending’s addendum to the resident admission or progress note. 3. Co-signature by the attending implies that the attending has reviewed the resident note or other health record entry, and absent an addendum to the contrary, concurs with the content of the resident note or entry. Use of CPRS function "Additional Signer" is not acceptable for documenting supervision. 4. Resident documentation of attending supervision. [Includes involvement of the attending and the attending’s level of supervision or oversight responsibility (e.g., "I have seen and discussed the patient with my attending, Dr. 'X', and Dr. 'X' agrees with my assessment and plan"), at a minimum, the responsible attending should be identified (e.g., "The attending of record for this patient encounter is Dr. 'X'")] Outpatient: New Patient Visit (includes Emergency Department visits) Attending must be physically present in the clinic. Every patient who is new to the facility must be seen by or discussed with an attending. Documentation: An independent note, addendum to the resident's note, or resident note description of attending involvement. -

Student Clerkship Guide a Comprehensive Guide to Clerkship at the Ottawa Hospital
STUDENT CLERKSHIP GUIDE A COMPREHENSIVE GUIDE TO CLERKSHIP AT THE OTTAWA HOSPITAL Gemma Cox and Stephanie Lubchansky MD 2015 CANDIDATES SPECIAL THANKS To Dr. Krista Wooller for her guidance, support, and feedback during the writing process. The Faculty of Medicine at the University of Ottawa for supporting this endeavor. EDITORS-IN-CHIEF EDITORS Gemma Cox, MD Candidate 2015 Pierre-Olivier Auclair, Mandatory Selectives Coordinator Stephanie Lubchansky, MD Candidate 2015 Dr. Contreras-Dominguez, Internal Medicine Rotation Director FACULTY SUPERVISOR Kelly Frydrych, MD Candidate 2015 Dr. Krista Wooller Julie Ghatalia, Department of Anesthesiology CONTRIBUTORS Celine Giordano, MD Candidate 2015 Kevin Dong, MD Candidate 2015 Hilary Gore, Department of Obstetrics and Bani Falcon, MD Candidate 2015 Gynecology Kelly Frydrych, MD Candidate 2015 Dr. Laura Hopkins, Obstetrics and Habibat Garuba, PGY-2 Internal Medicine Gynecology Rotation Director Celine Giordano, MD Candidate 2015 Dr. B.K. Lam, Surgery Rotation Director Anne McHale, MD Candidate 2015 Dr. Tim Lau, Department of Psychiatry Department of Pediatrics, Children’s Dr. Safeena Kherani, Mandatory Selectives Hospital of Eastern Ontario (CHEO) Rotation Director Department of Surgery, The Ottawa Anne McHale, MD Candidate 2015 Hospital Dr. Eoghan O’Shea, Family Medicine Rotation Diector Dr. Nikhil Rastogi, Anesthesiology Rotation Director Brigitte Rutherford, Department of Psychiatry Denis Vadeboncoeur, 3rd year Liaison Officer Dr. Krista Wooller, Department of Internal Medicine Amy Whyte, Department of Surgery Donna Williams, Department of Family Medicine Dr. Stella Yiu, Emergency Medicine Rotation Director Dr. Marc Zucker, Pediatrics Rotation Director A FEW WORDS FROM THE EDITORS IN CHIEF… This guide was created to help orient you, the incoming clerkship class, to the many experiences that you will encounter over the course of this year. -

The Contribution of the Medical History for the Diagnosis of Simulated Cases by Medical Students
International Journal of Medical Education. 2012;3:78-82 ISSN: 2042-6372 DOI: 10.5116/ijme.4f8a.e48c The contribution of the medical history for the diagnosis of simulated cases by medical students Tomoko Tsukamoto, Yoshiyuki Ohira, Kazutaka Noda, Toshihiko Takada, Masatomi Ikusaka Department of General Medicine, Chiba University Hospital, Japan Correspondence: Tomoko Tsukamoto, Department of General Medicine, Chiba University Hospital, 1-8-1 Inohana, Chuo-ku, Chiba city, Chiba, 260-8677 Japan. Email: [email protected] Accepted: April 15, 2012 Abstract Objectives: The case history is an important part of diag- rates were compared using analysis of the χ2-test. nostic reasoning. The patient management problem method Results: Sixty students (63.8%) made a correct diagnosis, has been used in various studies, but may not reflect the which was based on the history in 43 students (71.7%), actual reasoning process because a list of choices is given to physical findings in 11 students (18.3%), and laboratory the subjects in advance. This study investigated the contri- data in 6 students (10.0%). Compared with students who bution of the history to making the correct diagnosis by considered the correct diagnosis in their differential diagno- using clinical case simulation, in which students obtained sis after taking a history, students who failed to do so were clinical information by themselves. 5.0 times (95%CI = 2.5-9.8) more likely to make a final Methods: A prospective study was conducted. Ninety-four misdiagnosis (χ2(1) = 30.73; p<0.001). fifth-year medical students from Chiba University who Conclusions: History taking is especially important for underwent supervised clinical clerkships in 2009 were making a correct diagnosis when students perform clinical surveyed. -

Peripheral Arterial Disease | Piedmont Healthcare
Peripheral Arterial Disease CLAUDICATION TO LIMB THREATENING ISCHEMIA THE HOW AND WHEN TO EVALUATE AND TREAT Brian M Freeman MD FACS Nothing to Disclose PAD: Peripheral Arterial Disease Obstruction of any “peripheral artery” Causes – Atherosclerosis – Emboli – Extrinsic compression – Vasculitis PAD Effects more than 15 million Americans Majority of patients are asymptomatic African Americans and Hispanics are at risk Diabetics with PAD are at significant risk for amputations (Neuropathy + PAD) PAD Risk Factors PAD: PREVALENCE vs AGE PAD: More Prevalent and More Deadly Than Many Leading Diseases Disease Prevalence (Millions) Five-Year Mortality Rate 5 50% 17.0 4 40% 39% 30% 3 30% 28% 12.6 12.0 8.9 21% 2 4.8 20% 5.0 14% 4.0 1 10% 0 0% Diabetes Coronary PAD Cancer CHF Stroke Alzheimers Colorectal PAD Stroke CAD Breast Heart Cancer Cancer Disease Source: American Cancer Society, American Heart Association, Alzheimers Disease Education/Referral Center, American Diabetes Association, SAGE Group PAD: LONG-TERM MORTALITY Atherosclerosis is a Systemic Disease Lesion Location Consequence Carotid, cerebral Stroke Aorta, arch Aneurysm Coronary artery MI Renal artery HTN, CRF Mesenteric Bowel infarct Iliac artery Impotence Femoral artery Claudication Tibial artery Limb loss PAD There is a 5 fold increase in the relative risk of a Cardiovascular ischemic event Total Mortality is increased 2-3 X Visual Cues to PAD and Arterial Insufficiency Cool, dry, atrophic skin on legs Thickened or deformed nails-dystrophic Hair loss or uneven distribution on legs -

Junior Doctor Skill in the Art of Physical Examination: a Retrospective Study of the Medical Admission Note Over Four Decades
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2012-002257 on 3 April 2013. Downloaded from Junior doctor skill in the art of physical examination: a retrospective study of the medical admission note over four decades Charlotte M Oliver,1 Selena A Hunter,2 Takayoshi Ikeda,3 Duncan C Galletly2 To cite: Oliver CM, ABSTRACT et al ARTICLE SUMMARY Hunter SA, Ikeda T, . Objectives: To investigate the hypothesis that junior Junior doctor skill in the art doctors’ examination skills are deteriorating by assessing of physical examination: a Article focus the medical admission note examination record. retrospective study ▪ There is well-documented international evidence of the medical admission Design: Retrospective study of the admission record. supporting a declining standard in junior note over four decades. BMJ Setting: Tertiary care hospital. doctors’ physical examination skills in recent Open 2013;3:e002257. Methods: The admission records of 266 patients years. doi:10.1136/bmjopen-2012- admitted to Wellington hospital between 1975 and 2011 ▪ This study was conducted to address the 002257 were analysed, according to the total number of physical research question that this deterioration has examination observations (PEOtot), examination of the occurred locally in Wellington, New Zealand. ▸ Prepublication history for relevant system pertaining to the presenting complaint this paper are available (RelSystem) and the number of body systems examined Key messages ▪ There has been a decline in the quantity and online. To view these files (Nsystems). Subgroup analysis proceeded according to quality of the medical admission note examin- please visit the journal online admission year, level of experience of the admitting (http://dx.doi.org/10.1136/ ation records in this tertiary care centre between doctor (registrar, house surgeon (HS) and trainee intern bmjopen-2012-002257).