Critical Care Reviews Book 2017 Summarising, Critiquing and Putting in Context the Best Critical Care Trials of 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Calling All Music Lovers!
Plugged In Issue Six • the official school newspaper of Speedway Senior High School • March 1,1 2011 A pro prospect in our midst? Lost Frogs: Junior hockey star just one of the guys Four Found Greatness comes in many shapes and sizes. At Speedway and other east High, it comes in the form of 5’6”, 135-pound junior, Mason coast cities than By Sandy Bauers The Philadelphia Inquirer Jobst. He is one of the top junior hockey prospects in his age in Indianapolis. (MCT) group. Jobst has talked to In August, conservationists and The 17-year old center has lived and breathed hockey recruiters at many biologists launched a five-month nearly his entire life. It all started on his third birthday, when colleges around the search to try to find 100 “lost” species young Mason received a pair of brand new ice skates. Soon country; Colorado, of amphibians. Some 126 researchers after, he was wearing them around constantly. At age four, Minnesota, Yale, combed five continents in search of Jobst enrolled in his first youth hockey league, where he Maine, and Boston frogs, salamanders and others that had played the game for the first time at Pepsi Coliseum. College. not been seen in a decade or longer Nowadays, Mason is still playing hockey at Pepsi Mason spends a and were feared extinct. Coliseum. Recently, he had the chance to play on United lot of time working The good/bad news: They found States Hockey out. He has U18, four. They also made 11 re-discoveries League’s (USHL) Indiana Jr. -

Columbia Chronicle College Publications
Columbia College Chicago Digital Commons @ Columbia College Chicago Columbia Chronicle College Publications 1-8-1990 Columbia Chronicle (01/08/1990) Columbia College Chicago Follow this and additional works at: http://digitalcommons.colum.edu/cadc_chronicle Part of the Journalism Studies Commons This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. Recommended Citation Columbia College Chicago, "Columbia Chronicle (01/8/1990)" (January 8, 1990). Columbia Chronicle, College Publications, College Archives & Special Collections, Columbia College Chicago. http://digitalcommons.colum.edu/cadc_chronicle/286 This Book is brought to you for free and open access by the College Publications at Digital Commons @ Columbia College Chicago. It has been accepted for inclusion in Columbia Chronicle by an authorized administrator of Digital Commons @ Columbia College Chicago. Club mobilizes political bigshots to win members Richardson is seeing is the dif By Mary Johnson lished, we can work with these ficulty people have making a time politicians to seek improvements S14ff Reporter commitment. for our school," Richardson said. In an effon to stimulate stu "He will find a small number dent interest, the newly organized of people who have made [the Those improvements, accord Political Club will host Aldennan Political Club] their top priority, ing to literature posted before the Danny K. Davis on Jan. 10 at 3 and it doesn't mean that the rest meeting, could include better p.m. in the Hokin Center, along of the students are apathetic. It parking facilities for students, with two other politicians who are means that there are other things more lunch space and a student seeking political office. -

5713 Theme Ideas
5713 THEME IDEAS & 1573 Bulldogs, no two are the same & counting 2B part of something > U & more 2 can play that game & then... 2 good 2 b 4 gotten ? 2 good 2 forget ! 2 in one + 2 sides, same story * 2 sides to every story “ 20/20 vision # 21 and counting / 21 and older > 21 and playing with a full deck ... 24/7 1 and 2 make 12 25 old, 25 new 1 in a crowd 25 years and still soaring 1+1=2 decades 25 years of magic 10 minutes makes a difference 2010verland 10 reasons why 2013 a week at a time 10 things I Hart 2013 and ticking 10 things we knew 2013 at a time 10 times better 2013 degrees and rising 10 times more 2013 horsepower 10 times the ________ 2013 memories 12 words 2013 pieces 15 seconds of fame 2013 possibilities 17 reasons to be a Warrior 2013 reasons to howl 18 and counting 2013 ways to be a Leopard 18 and older 2 million minutes 100 plus you 20 million thoughts 100 reasons to celebrate 3D 100 years and counting Third time’s a charm 100 years in the making 3 dimensional 100 years of Bulldogs 3 is a crowd 100 years to get it right 3 of a kind 100% Dodger 3 to 1 100% genuine 3’s company 100% natural 30 years of impossible things 101 and only 360° 140 traditions CXL 4 all it’s worth 150 years of tradition 4 all to see (176) days of La Quinta 4 the last time 176 days and counting 4 way stop 180 days, no two are the same 4ming 180 days to leave your mark 40 years of colorful memories 180° The big 4-0 1,000 strong and growing XL (40) 1 Herff Jones 5713 Theme Ideas 404,830 (seconds from start to A close look A little bit more finish) A closer look A little bit of everything (except 5-star A colorful life girls) 5 ways A Comet’s journey A little bit of Sol V (as in five) A common ground A little give and take 5.4.3.2.1. -

Every Purchase Includes a Free Hot Drink out of Stock, but Can Re-Order New Arrival / Re-Stock
every purchase includes a free hot drink out of stock, but can re-order new arrival / re-stock VINYL PRICE 1975 - 1975 £ 22.00 30 Seconds to Mars - America £ 15.00 ABBA - Gold (2 LP) £ 23.00 ABBA - Live At Wembley Arena (3 LP) £ 38.00 Abbey Road (50th Anniversary) £ 27.00 AC/DC - Live '92 (2 LP) £ 25.00 AC/DC - Live At Old Waldorf In San Francisco September 3 1977 (Red Vinyl) £ 17.00 AC/DC - Live In Cleveland August 22 1977 (Orange Vinyl) £ 20.00 AC/DC- The Many Faces Of (2 LP) £ 20.00 Adele - 21 £ 19.00 Aerosmith- Done With Mirrors £ 25.00 Air- Moon Safari £ 26.00 Al Green - Let's Stay Together £ 20.00 Alanis Morissette - Jagged Little Pill £ 17.00 Alice Cooper - The Many Faces Of Alice Cooper (Opaque Splatter Marble Vinyl) (2 LP) £ 21.00 Alice in Chains - Live at the Palladium, Hollywood £ 17.00 ALLMAN BROTHERS BAND - Enlightened Rogues £ 16.00 ALLMAN BROTHERS BAND - Win Lose Or Draw £ 16.00 Altered Images- Greatest Hits £ 20.00 Amy Winehouse - Back to Black £ 20.00 Andrew W.K. - You're Not Alone (2 LP) £ 20.00 ANTAL DORATI - LONDON SYMPHONY ORCHESTRA - Stravinsky-The Firebird £ 18.00 Antonio Carlos Jobim - Wave (LP + CD) £ 21.00 Arcade Fire - Everything Now (Danish) £ 18.00 Arcade Fire - Funeral £ 20.00 ARCADE FIRE - Neon Bible £ 23.00 Arctic Monkeys - AM £ 24.00 Arctic Monkeys - Tranquility Base Hotel + Casino £ 23.00 Aretha Franklin - The Electrifying £ 10.00 Aretha Franklin - The Tender £ 15.00 Asher Roth- Asleep In The Bread Aisle - Translucent Gold Vinyl £ 17.00 B.B. -

Personal Music Collection
Christopher Lee :: Personal Music Collection electricshockmusic.com :: Saturday, 25 September 2021 < Back Forward > Christopher Lee's Personal Music Collection | # | A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | | DVD Audio | DVD Video | COMPACT DISCS Artist Title Year Label Notes # Digitally 10CC 10cc 1973, 2007 ZT's/Cherry Red Remastered UK import 4-CD Boxed Set 10CC Before During After: The Story Of 10cc 2017 UMC Netherlands import 10CC I'm Not In Love: The Essential 10cc 2016 Spectrum UK import Digitally 10CC The Original Soundtrack 1975, 1997 Mercury Remastered UK import Digitally Remastered 10CC The Very Best Of 10cc 1997 Mercury Australian import 80's Symphonic 2018 Rhino THE 1975 A Brief Inquiry Into Online Relationships 2018 Dirty Hit/Polydor UK import I Like It When You Sleep, For You Are So Beautiful THE 1975 2016 Dirty Hit/Interscope Yet So Unaware Of It THE 1975 Notes On A Conditional Form 2020 Dirty Hit/Interscope THE 1975 The 1975 2013 Dirty Hit/Polydor UK import {Return to Top} A A-HA 25 2010 Warner Bros./Rhino UK import A-HA Analogue 2005 Polydor Thailand import Deluxe Fanbox Edition A-HA Cast In Steel 2015 We Love Music/Polydor Boxed Set German import A-HA East Of The Sun West Of The Moon 1990 Warner Bros. German import Digitally Remastered A-HA East Of The Sun West Of The Moon 1990, 2015 Warner Bros./Rhino 2-CD/1-DVD Edition UK import 2-CD/1-DVD Ending On A High Note: The Final Concert Live At A-HA 2011 Universal Music Deluxe Edition Oslo Spektrum German import A-HA Foot Of The Mountain 2009 Universal Music German import A-HA Hunting High And Low 1985 Reprise Digitally Remastered A-HA Hunting High And Low 1985, 2010 Warner Bros./Rhino 2-CD Edition UK import Digitally Remastered Hunting High And Low: 30th Anniversary Deluxe A-HA 1985, 2015 Warner Bros./Rhino 4-CD/1-DVD Edition Boxed Set German import A-HA Lifelines 2002 WEA German import Digitally Remastered A-HA Lifelines 2002, 2019 Warner Bros./Rhino 2-CD Edition UK import A-HA Memorial Beach 1993 Warner Bros. -

Lita Ford and Doro Interviewed Inside Explores the Brightest Void and the Shadow Self
COMES WITH 78 FREE SONGS AND BONUS INTERVIEWS! Issue 75 £5.99 SUMMER Jul-Sep 2016 9 771754 958015 75> EXPLORES THE BRIGHTEST VOID AND THE SHADOW SELF LITA FORD AND DORO INTERVIEWED INSIDE Plus: Blues Pills, Scorpion Child, Witness PAUL GILBERT F DARE F FROST* F JOE LYNN TURNER THE MUSIC IS OUT THERE... FIREWORKS MAGAZINE PRESENTS 78 FREE SONGS WITH ISSUE #75! GROUP ONE: MELODIC HARD 22. Maessorr Structorr - Lonely Mariner 42. Axon-Neuron - Erasure 61. Zark - Lord Rat ROCK/AOR From the album: Rise At Fall From the album: Metamorphosis From the album: Tales of the Expected www.maessorrstructorr.com www.axonneuron.com www.facebook.com/zarkbanduk 1. Lotta Lené - Souls From the single: Souls 23. 21st Century Fugitives - Losing Time 43. Dimh Project - Wolves In The 62. Dejanira - Birth of the www.lottalene.com From the album: Losing Time Streets Unconquerable Sun www.facebook. From the album: Victim & Maker From the album: Behind The Scenes 2. Tarja - No Bitter End com/21stCenturyFugitives www.facebook.com/dimhproject www.dejanira.org From the album: The Brightest Void www.tarjaturunen.com 24. Darkness Light - Long Ago 44. Mercutio - Shed Your Skin 63. Sfyrokalymnon - Son of Sin From the album: Living With The Danger From the album: Back To Nowhere From the album: The Sign Of Concrete 3. Grandhour - All In Or Nothing http://darknesslight.de Mercutio.me Creation From the album: Bombs & Bullets www.sfyrokalymnon.com www.grandhourband.com GROUP TWO: 70s RETRO ROCK/ 45. Medusa - Queima PSYCHEDELIC/BLUES/SOUTHERN From the album: Monstrologia (Lado A) 64. Chaosmic - Forever Feast 4. -

The BG News October 20, 2000
Bowling Green State University ScholarWorks@BGSU BG News (Student Newspaper) University Publications 10-20-2000 The BG News October 20, 2000 Bowling Green State University Follow this and additional works at: https://scholarworks.bgsu.edu/bg-news Recommended Citation Bowling Green State University, "The BG News October 20, 2000" (2000). BG News (Student Newspaper). 6704. https://scholarworks.bgsu.edu/bg-news/6704 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This Article is brought to you for free and open access by the University Publications at ScholarWorks@BGSU. It has been accepted for inclusion in BG News (Student Newspaper) by an authorized administrator of ScholarWorks@BGSU. m M 1 Bowling Green State University FRIDAY October 20, 2000 Brian Engelman talks ^^ « ■/ 1/ i 1 SUNNY one on one with gui- ■■ 1 A W ■ k HIGH: 74 | LOW: 48 tarist Dan Donegan; I \ -^ ■ J—^ -K_y www.bgnews.com VOLUME 90 ISSUE 37 Union renovation on schedule By Craig Grtfofd "They (the constniction crew) pletion. We are hopeful that it will tion," Crooks said. "We are eager CAMPUS toiioa are very eager to hustle on the I*' completed around Dec. 12." to be back in business and look- The building of Che new project," Crooks said. "Things Gale Swanka, associate direc- ing forward to the pleasure of m^Li^LW Student Union is on schedule have gone as well as we could tor of the Student Union, agrees operating the new facility." and is expected to be completed have hoped." that the Union is on schedule, but Swanka sees more of a sense of 0 m ■ by December 2001, said Dave With all of the destruction tak- anything could still happen. -

And a Letter to My Customers ===
--- == ROOTS & RHYTHM - SALE 01/12/2014 - AND A LETTER TO MY CUSTOMERS === --- Dear Friends Happy New Year! We hope you all had a wonderful holiday season. NOTE: Regrettably our holiday season was the slowest we've ever seen and it may mean that we will not be able to continue operating our business for very much longer. I am no longer a young man (not by a long shot!) and don't have the energy to pursue ways in which we may be able to promote the business. I would love to be able to settle down and listen to all the music I have gathered over the years in a relaxed setting and with critical reviewing faculties turned off. I would love to see Roots & Rhythm continue and thrive and even if we make it through the current crisis I would still like to get away from the stress of running a business so I am open to having someone else take over and move the company forward. If you are such a person or know such a person please contact me and we can discuss it. This list consists of a sale which we hope will raise enough money to help us get caught up with our suppliers and our taxes as well as some other pressing expenses. This list features 600 titles in all covering all the genres of music we specialize in and featuring books, DVDs and compact discs. This list includes manufacturer?s overstocks and deletions, our own excess inventory and a lot of titles that have been sitting on our shelves that have never been listed before. -

Canada's Large Intact Forest Landscapes
Global Forest Watch Global Forest Watch is an international network that provides timely, accurate, and balanced information and analysis on forests and forest use to promote public understanding, informed decision-making, support for practical management solutions, and enhanced accountability. The World Resources Institute launched Global Forest Watch in 1997. Global Forest Watch Canada Global Forest Watch Canada is a partner in the Global Forest Watch network, and was formed to provide access to more complete information about development activities in Canada’s forests and their environmental impacts. We are convinced that providing greater information about Canada’s forests will lead to better decision-making on forest management and use, which ultimately will result in forest management regimes that provide a full range of benefits for both present and future generations. Canada’s Large Intact Forest Landscapes A report by Global Forest Watch Canada By: Peter Lee (Global Forest Watch Canada) Dmitry Aksenov (Socio-Ecological Union International) Lars Laestadius (World Resources Institute) Ruth Nogueron (World Resources Institute) Wynet Smith (Global Forest Watch Canada) Edmonton, Alberta Canada 2003 Canada’s Large Intact Forest Landscapes A report by Global Forest Watch Canada By: Peter Lee (Global Forest Watch Canada) Dmitry Aksenov (Socio-Ecological Union International) Lars Laestadius (World Resources Institute) Ruth Nogueron (World Resources Institute) Wynet Smith (Global Forest Watch Canada) GIS analysis and research: Maxim Dubinin -
Kenyon Collegian College Archives
Digital Kenyon: Research, Scholarship, and Creative Exchange The Kenyon Collegian College Archives 11-16-1978 Kenyon Collegian - November 16, 1978 Follow this and additional works at: https://digital.kenyon.edu/collegian Recommended Citation "Kenyon Collegian - November 16, 1978" (1978). The Kenyon Collegian. 1004. https://digital.kenyon.edu/collegian/1004 This News Article is brought to you for free and open access by the College Archives at Digital Kenyon: Research, Scholarship, and Creative Exchange. It has been accepted for inclusion in The Kenyon Collegian by an authorized administrator of Digital Kenyon: Research, Scholarship, and Creative Exchange. For more information, please contact [email protected]. Colleg Established 1856 ;CVI, Number 10 Kenyon College, Gambier, Ohio 43022 Money: the root of new o I Council's first concerns By SUSAN J ACOBY really be the body of investigation for asked about alternative ways Staff Writer such a matter. To to cover temporarily settle the damage, Kurella replied, Vice-Preside- nt "I'm things, Maureen -- not aware of any other source. We .. The "Renaissance Man and Corcoran moved that council should don't budget damage." Woman" has been the object of not decide until the matter has been this Fall. Most of these juny pranks investigated more thoroughly by an Another important issue brought elicited chuckles from mentions appointed committee. up at Sunday's meeting was the Middle-Pathe- rs and were then easily In a short interview Mr. John Student Activities Fee Referendum. amoved. However, such was not the Kurella, manager of Business Ser- "A non vote is a 'no' vote," Gould 'ase with Ine mysterious Halloween vices, pointed out that there is an reminded council, who, with the "T-p'in- This, along with g" paim job. -
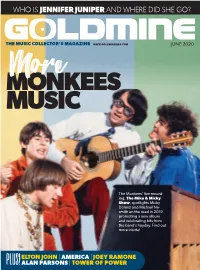
Who Is Jennifer Juniper and Where Did She Go?
WHO IS JENNIFER JUNIPER AND WHERE DID SHE GO? THE MUSIC COLLECTOR’S MAGAZINE WWW.GOLDMINEMAG.COM JUNE 2020 More MONKEES MUSIC The Monkees’ live record- ing, The Mike & Micky Show, spotlights Micky Dolenz and Michael Ne- smith on the road in 2019 promoting a new album and celebrating hits from the band’s heyday. Find out more inside! ELTON JOHN | AMERICA | JOEY RAMONE PLUS! ALAN PARSONS | TOWER OF POWER GM 918 Cover.indd 1 4/8/20 1:54 PM ENTERTAINMENT AND MUSIC July 11 | Dallas | Live & Online ACCEPTING CONSIGNMENTS Michael Jackson Abbey Road Original UK Marilyn Monroe Signed The Beatles Jr. Rolling Stones Nirvana/Screaming Swarovski Triumph Tour Street Sign Black and White Vintage Toy Promo Autographed Program Trees/Tad Pine Street Helmet (1981) Sold for $10,625 Photograph (1950s) Guitar by Mastro from 2nd-Ever American Theatre Concert Sold for $35,000 Sold for $9,687 (NEMS, 1964) Concert Date (June 1964) Poster (1990) Sold for $8,125 Sold for $5,250 Sold for $2,250 Bob Dylan “Blowin’ in Duane Allman’s Circa 1961/1962 Gibson SG, Cherry, Solid Body The Beatles Introducing ... the Wind” Vintage 10” Electric Guitar, Serial #15263 Owned and Played by Graham Nash Mono Sealed LP Metal Acetate Sold for $591,000 Sold for $11,250 Sold for $2,750 Bob Dylan Signed Highway Steppenwolf “Born to Be The Beatles 1966 Wild” White Matte RIAA Grateful Dead 1966 61 Revisited Reissue Genuine, Original Red Hot Chili Peppers/ Jimi Hendrix/Janis Gold Sales Award and “Skeleton & Roses” Stereo Vinyl LP (Legacy/ Shea Stadium NYC Nirvana/Pearl Jam Joplin/The Who -

Smash Hits Volume 19
l^^^^^B _jK_____B_ ^^j^rf/j I i I'J ^ ^^^3 August 23-September 5 1979 mjijtliiiT' ' 'i 25p a* lonT.lCE ' f . YiorcLs xo vnc at ! TOP SINGLES including ^^ O <5 <<* o^ *>° ^ 0>* <\«P>"V &*J BSfc's plus bddibcochka mmm CARS By Gary Numan on Beggars Banquet Records Here in my car I feel safest of all I can lock all my doors It's the only way to live In cars Here in my car I can only receive I can listen to you It keeps me stable for days In cars Here in my car The image breaks down Will you visit me? Please? If I open my door In cars Here in my car I know I've started to think About leaving tonight Although nothing seems right In cars I know I've started to think I know I've started to think Words and music by Gary Numan Reproduced by permission Beggars Banquet/Andrew Heath Music -^&& p»c l toot > / ->/-;..( &$ v ^^i~.L<k\kv ^.^> l >v'-/''/s'C'r SMASH HITSHI 3 - rtf^v v«u Need Wheels Parka5 Merton deals BY The Choruscto,„s wanna make °^ , haftls ,f vou wheels 'iv° You need " get hot need a ,„ his hand You tOPJIJ^SSman wrt man ain«t a h ^ wheels A get a pn T K you wanna dead a low slung *£*£%£ noting , fl0t SaVeed one hundred du8t ^' ' S P th"ta,n trUSt K^heta"^n«* Repeat chorus the unique All ^fVjTthat's so — ek srcsAifa *. - chorus Repeat chrome s&Srsssst-- Only °ne own Repeat chorus wheels You need Repeat to fade ^ mu b Words and f j£ permission Music.