Stroke Due to Other Mechanisms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
CADASIL Testing
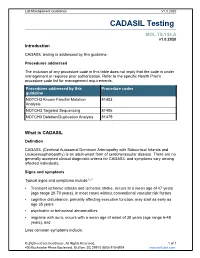
Lab Management Guidelines V1.0.2020 CADASIL Testing MOL.TS.144.A v1.0.2020 Introduction CADASIL testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline NOTCH3 Known Familial Mutation 81403 Analysis NOTCH3 Targeted Sequencing 81406 NOTCH3 Deletion/Duplication Analysis 81479 What is CADASIL Definition CADASIL (Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy) is an adult-onset form of cerebrovascular disease. There are no generally accepted clinical diagnostic criteria for CADASIL and symptoms vary among affected individuals. Signs and symptoms Typical signs and symptoms include1,2,3 Transient ischemic attacks and ischemic stroke, occurs at a mean age of 47 years (age range 20-70 years), in most cases without conventional vascular risk factors cognitive disturbance, primarily affecting executive function, may start as early as age 35 years psychiatric or behavioral abnormalities migraine with aura, occurs with a mean age of onset of 30 years (age range 6-48 years), and Less common symptoms include: © 2020 eviCore healthcare. All Rights Reserved. 1 of 7 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2020 recurrent seizures with onset in middle age, usually secondary to stroke acute encephalopathy, with a mean age of onset of 42 years Life expectancy for men with CADASIL is reduced by approximately five years and for women by 1 to 2 years.4 Diagnosis Brain Magnetic Resonance Imaging (MRI) findings include T2-signal-abnormalities in the white matter of the temporal pole and T2-signal-abnormalities in the external capsule and corpus callosum.1,2 CADASIL is suspected in an individual with the clinical signs and MRI findings. -

The National Economic Burden of Rare Disease Study February 2021
Acknowledgements This study was sponsored by the EveryLife Foundation for Rare Diseases and made possible through the collaborative efforts of the national rare disease community and key stakeholders. The EveryLife Foundation thanks all those who shared their expertise and insights to provide invaluable input to the study including: the Lewin Group, the EveryLife Community Congress membership, the Technical Advisory Group for this study, leadership from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH), the Undiagnosed Diseases Network (UDN), the Little Hercules Foundation, the Rare Disease Legislative Advocates (RDLA) Advisory Committee, SmithSolve, and our study funders. Most especially, we thank the members of our rare disease patient and caregiver community who participated in this effort and have helped to transform their lived experience into quantifiable data. LEWIN GROUP PROJECT STAFF Grace Yang, MPA, MA, Vice President Inna Cintina, PhD, Senior Consultant Matt Zhou, BS, Research Consultant Daniel Emont, MPH, Research Consultant Janice Lin, BS, Consultant Samuel Kallman, BA, BS, Research Consultant EVERYLIFE FOUNDATION PROJECT STAFF Annie Kennedy, BS, Chief of Policy and Advocacy Julia Jenkins, BA, Executive Director Jamie Sullivan, MPH, Director of Policy TECHNICAL ADVISORY GROUP Annie Kennedy, BS, Chief of Policy & Advocacy, EveryLife Foundation for Rare Diseases Anne Pariser, MD, Director, Office of Rare Diseases Research, National Center for Advancing Translational Sciences (NCATS), National Institutes of Health Elisabeth M. Oehrlein, PhD, MS, Senior Director, Research and Programs, National Health Council Christina Hartman, Senior Director of Advocacy, The Assistance Fund Kathleen Stratton, National Academies of Science, Engineering and Medicine (NASEM) Steve Silvestri, Director, Government Affairs, Neurocrine Biosciences Inc. -

Cadasil Pathogenesis, Clinical and Radiological Findings and Treatment
View and review Arq Neuropsiquiatr 2010;68(2):287-299 Cadasil Pathogenesis, clinical and radiological findings and treatment Charles André ABSTRACT Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is the most common genetic cause of ischemic strokes and a most important model for the study of subcortical vascular dementia. This unrelentlessly progressive disease affects many hundreds of families all over the world but is not well studied in Brazil. This manuscript reviews pathogenetic, clinical, radiological and therapeutic features of CADASIL. The causal mutations are now very well known, but the same can not be said about its intimate pathogenetic mechanisms. The variable clinical presentation should lead physicians to actively pursue the diagnosis in many settings and to more thouroughly investigate family history in first degree relatives. A rational approach to genetic testing is however needed. Treatment of CADASIL is still largely empiric. High- quality therapeutic studies involving medications and cognitive interventions are strongly needed in CADASIL. Key words: CADASIL, etiology, genetics, diagnosis, therapeutics. CADASIL: patogênese, achados clínicos e radiológicos e tratamento RESUMO CADASIL é a causa genética mais freqüente de infartos cerebrais e constitui modelo importante de estudo de demências vasculares subcorticais. De natureza inexoravelmente progressiva, afeta milhares de pessoas em todo o mundo. Sua importância é pouco reconhecida entre nós, o que nos levou à presente revisão dos principais aspectos patogenéticos, clínicos, neuroradiológicos e terapêuticos da doença. As mutações causais são hoje bem conhecidas, mas os mecanismos patogenéticos íntimos ainda permanecem misteriosos. A apresentação clínica variável deve fazer com que os médicos considerem o diagnóstico em vários contextos clínicos e investiguem de forma mais extensa que o usual a história familial deparentes de primeiro grau. -

Read PDF Edition
REVIEW OF OPTOMETRY EARN 2 CE CREDITS: Positive Visual Phenomena—Etiologies Beyond the Eye, PAGE 58 ■ VOL. 155 NO. 1 January 15, 2018 www.reviewofoptometry.comwww.reviewofoptometry.com ■ ANNUAL CORNEA REPORT JANUARY 15, 2018 ■ CXL ■ EPITHELIAL DEFECTS How to Heal Persistent Epithelial Defects PAGE 38 ■ TRANSPLANTS Corneal Transplants: The OD’s Role PAGE 44 ■ INFILTRATES Diagnosing Corneal Infiltrative Disease PAGE 50 ■ POSITIVE VISUAL PHENOMENA CXL: Your Top 12 Questions —Answered! PAGE 30 001_ro0118_fc.indd 1 1/5/18 4:34 PM ĊčĞĉėĆęĊĉĆĒēĎĔęĎĈĒĊĒćėĆēĊċĔėĎēǦĔċċĎĈĊĕėĔĈĊĉĚėĊĘ ĊđĎĊċĎēĘĎČčę ċċĊĈęĎěĊ Ȉ 1 Ȉ 1 ĊđđǦęĔđĊėĆęĊĉ Ȉ Ȉ ĎĒĕđĊĎēǦĔċċĎĈĊĕėĔĈĊĉĚėĊ Ȉ Ȉ ĔēěĊēĎĊēę Ȉ͝ Ȉ Ȉ Ƭ 1 ǡ ǡǡǤ͚͙͘͜Ǥ Ȁ Ǥ ͚͙͘͜ǣ͘͘ǣ͘͘͘Ǧ͘͘͘ ĕĕđĎĈĆęĎĔēĘ Ȉ Ȉ Ȉ Ȉ Ȉ čĊĚėĎĔē̾ėĔĈĊĘĘ Ȉ Ȉ Katena — Your completecomplete resource forfor amniotic membrane pprocedurerocedure pproducts:roducts: Single use speculums Single use spears ͙͘͘ǡ͘͘͘ήĊĞĊĘęėĊĆęĊĉ Forceps ® ,#"EWB3FW XXXLBUFOBDPNr RO0118_Katena.indd 1 1/2/18 10:34 AM News Review VOL. 155 NO. 1 ■ JANUARY 15, 2018 IN THE NEWS Accelerated CXL Shows The FDA recently approved Luxturna (voretigene neparvovec-rzyl, Spark Promise—and Caution Therapeutics), a directly administered gene therapy that targets biallelic This new technology is already advancing, but not without RPE65 mutation-associated retinal dystrophy. The therapy is designed to some bumps in the road. deliver a normal copy of the gene to By Rebecca Hepp, Managing Editor retinal cells to restore vision loss. While the approval provides hope for patients, wo new studies highlight the resulted in infection—while tradi- the $425,000 per eye price tag stands as pros and cons of accelerated tional C-CXL has a reported inci- a signifi cant hurdle. -

Migraine Triggered Seizures and Epilepsy Triggered Headache and Migraine Attacks: a Need for Re-Assessment
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central J Headache Pain (2011) 12:287–288 DOI 10.1007/s10194-011-0344-2 COMMENTARY Migraine triggered seizures and epilepsy triggered headache and migraine attacks: a need for re-assessment Paul T. G. Davies • C. P. Panayiotopoulos Received: 5 April 2011 / Accepted: 8 April 2011 / Published online: 24 April 2011 Ó The Author(s) 2011. This article is published with open access at Springerlink.com In this issue of the Journal, Belcastro and associates review Migralepsy terminology and classification issues for migralepsy, hem- icrania epileptica, post-ictal and ictal headache [1]. They According to the ICHD-II 1.5.5, ‘‘migraine-triggered sei- raise key points such as ictal headache and visual seizures zure (sometimes referred to as migralepsy)’’ denotes an are often misdiagnosed as migraine, ‘‘migralepsy’’ is unli- epileptic seizure that occurs ‘‘during or within one hour kely to exist and an ‘‘epilepsy-migraine sequence’’ is much after a migraine aura’’ [3]. However, the evidence of this more common and well documented than the dominant ‘‘migraine-seizure’’ sequence is weak and the proposed view of a ‘‘migraine-epilepsy sequence’’. Their relevant criterion of 1 h gap between the end of the ‘‘aura’’ and the proposals need appropriate attention by the committee of start of an epileptic seizure is entirely arbitrary the international classification of headache disorders Migralepsy is an old term derived from migra(ine) and (ICHD) as well as the physicians in their clinical practice (epi)lepsy, coined by Dr Douglas Davidson, but mainly because of the consequences that misdiagnosis may have on attributed to Lennox and Lennox, which we quote, ‘‘a patients. -

TIA Vs CVA (STROKE)
Phone: 973.334.3443 Email: [email protected] NJPR.com TIA vs CVA (STROKE) What is the difference between a TIA and a stroke? Difference Between TIA and Stroke • Both TIA and stroke are due to poor blood supply to the brain. • Stroke is a medical emergency and it’s a life-threatening condition. • The symptoms of TIA and Stroke may be same but TIA symptoms will recover within 24 hours. TRANSIENT ISCHEMIC ATTACK ● Also known as: TIA, mini stroke 80 E. Ridgewood Avenue, 4th Floor Paramus, NJ 07652 TIA Causes ● A transient ischemic attack has the same origins as that of an ischemic stroke, the most common type of stroke. In an ischemic stroke, a clot blocks the blood supply to part of your brain. In a transient ischemic attack, unlike a stroke, the blockage is brief, and there is no permanent damage. ● The underlying cause of a TIA often is a buildup of cholesterol- containing fatty deposits called plaques (atherosclerosis) in an artery or one of its branches that supplies oxygen and nutrients to your brain. ● Plaques can decrease the blood flow through an artery or lead to the development of a clot. A blood clot moving to an artery that supplies your brain from another part of your body, most commonly from your heart, also may cause a TIA. CEREBROVASCULAR ACCIDENT/STROKE Page 2 When the brain’s blood supply is insufficient, a stroke occurs. Stroke symptoms (for example, slurring of speech or loss of function in an arm or leg) indicate a medical emergency. Without treatment, the brain cells quickly become impaired or die. -

Elementary Visual Hallucinations, Blindness, and Headache in Idiopathic Occipital Epilepsy: Diverentiation from Migraine
536 J Neurol Neurosurg Psychiatry 1999;66:536–540 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.66.4.536 on 1 April 1999. Downloaded from SHORT REPORT Elementary visual hallucinations, blindness, and headache in idiopathic occipital epilepsy: diVerentiation from migraine C P Panayiotopoulos Abstract also fundamental symptoms often with the This is a qualitative and chronological same sequence of events in occipital seizures.1−9 analysis of ictal and postictal symptoms, This is a systematic prospective qualitative frequency of seizures, family history, study of the characteristics of elementary visual response to treatment, and prognosis in hallucinations, blindness, and headache in nine patients with idiopathic occipital epi- idiopathic occipital epilepsy. lepsy and visual seizures. Ictal elementary visual hallucinations are stereotyped for Methods each patient, usually lasting for seconds. These are detailed elsewhere.910 Patients with They consist of mainly multiple, bright occipital seizures were prospectively evaluated coloured, small circular spots, circles, or and followed up from 1973. Nine patients with balls. Mostly, they appear in a temporal idiopathic occipital epilepsy with visual halluci- hemifield often moving contralaterally or nations (IOEVH) had: in the centre where they may be flashing. (a) Incontrovertible clinical evidence of oc- They may multiply and increase in size in cipital seizures with or without secondarily the course of the seizure and may progress generalisation. to other non-visual occipital seizure (b) Normal physical, neurological, and men- symptoms and more rarely to extra- tal states and high resolution MRI. They all had detailed interviews, seven com- occipital manifestations and convulsions. 9 Blindness occurs usually from the begin- pleted a purposely designed questionnaire, ning and postictal headache, often indis- and eight provided drawings of their visual hal- tinguishable from migraine, is common. -

Prevalence and Incidence of Rare Diseases: Bibliographic Data
Number 1 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Prevalence, incidence or number of published cases listed by diseases (in alphabetical order) www.orpha.net www.orphadata.org If a range of national data is available, the average is Methodology calculated to estimate the worldwide or European prevalence or incidence. When a range of data sources is available, the most Orphanet carries out a systematic survey of literature in recent data source that meets a certain number of quality order to estimate the prevalence and incidence of rare criteria is favoured (registries, meta-analyses, diseases. This study aims to collect new data regarding population-based studies, large cohorts studies). point prevalence, birth prevalence and incidence, and to update already published data according to new For congenital diseases, the prevalence is estimated, so scientific studies or other available data. that: Prevalence = birth prevalence x (patient life This data is presented in the following reports published expectancy/general population life expectancy). biannually: When only incidence data is documented, the prevalence is estimated when possible, so that : • Prevalence, incidence or number of published cases listed by diseases (in alphabetical order); Prevalence = incidence x disease mean duration. • Diseases listed by decreasing prevalence, incidence When neither prevalence nor incidence data is available, or number of published cases; which is the case for very rare diseases, the number of cases or families documented in the medical literature is Data collection provided. A number of different sources are used : Limitations of the study • Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report are only estimations and cannot be considered to • National/international health institutes and agencies be absolutely correct. -

Insurance and Advance Pay Test Requisition
Insurance and Advance Pay Test Requisition (2021) For Specimen Collection Service, Please Fax this Test Requisition to 1.610.271.6085 Client Services is available Monday through Friday from 8:30 AM to 9:00 PM EST at 1.800.394.4493, option 2 Patient Information Patient Name Patient ID# (if available) Date of Birth Sex designated at birth: 9 Male 9 Female Street address City, State, Zip Mobile phone #1 Other Phone #2 Patient email Language spoken if other than English Test and Specimen Information Consult test list for test code and name Test Code: Test Name: Test Code: Test Name: 9 Check if more than 2 tests are ordered. Additional tests should be checked off within the test list ICD-10 Codes (required for billing insurance): Clinical diagnosis: Age at Initial Presentation: Ancestral Background (check all that apply): 9 African 9 Asian: East 9 Asian: Southeast 9 Central/South American 9 Hispanic 9 Native American 9 Ashkenazi Jewish 9 Asian: Indian 9 Caribbean 9 European 9 Middle Eastern 9 Pacific Islander Other: Indications for genetic testing (please check one): 9 Diagnostic (symptomatic) 9 Predictive (asymptomatic) 9 Prenatal* 9 Carrier 9 Family testing/single site Relationship to Proband: If performed at Athena, provide relative’s accession # . If performed at another lab, a copy of the relative’s report is required. Please attach detailed medical records and family history information Specimen Type: Date sample obtained: __________ /__________ /__________ 9 Whole Blood 9 Serum 9 CSF 9 Muscle 9 CVS: Cultured 9 Amniotic Fluid: Cultured 9 Saliva (Not available for all tests) 9 DNA** - tissue source: Concentration ug/ml Was DNA extracted at a CLIA-certified laboratory or a laboratory meeting equivalent requirements (as determined by CAP and/or CMS)? 9 Yes 9 No 9 Other*: If not collected same day as shipped, how was sample stored? 9 Room temp 9 Refrigerated 9 Frozen (-20) 9 Frozen (-80) History of blood transfusion? 9 Yes 9 No Most recent transfusion: __________ /__________ /__________ *Please contact us at 1.800.394.4493, option 2 prior to sending specimens. -

Genetics of Hypertension Paul N
November/December 2003 ⅐ Vol. 5 ⅐ No. 6 review Genetics of hypertension Paul N. Hopkins, MD, MSPH and Steven C. Hunt, PhD Hypertension is the most prevalent cardiovascular disorder. progressively to arterial and arteriolar hypertrophy, arterio- In the 1999 to 2000 NHANES survey, the prevalence of hyper- sclerosis and arteriolosclerosis, and with very high pressures to tension progressively increased from 7.2% in those aged 18 to fibrinoid change and fibrinoid necrosis in arterioles. These lat- 39 to 30.1% in 40 to 59 year olds and 65.4% in those 60 and ter changes can result in lumen compromise of arterioles re- older.1 Risk of both coronary atherosclerosis and stroke in- sulting in lacunar stroke, Charcot-Bouchard aneurysms, glo- crease exponentially as blood pressure rises (see Fig. 1).2 Al- merulosclerosis and nephrosclerosis, and ultimately malignant though the relative risk for stroke increases more rapidly than hypertension in the kidney and retinal ischemia and blindness. coronary disease, at any pressure, the absolute risk for coro- Risk of intracerebral hemorrhage is increased 33-fold at stage 3 nary disease is considerably greater than for stroke. An insight or higher pressures compared to normal blood pressure.23 Un- into this finding comes from autopsy studies that show that the treated, malignant hypertension is associated with a 5-year carotid and intracerebral vascular beds are relatively protected mortality rate of 95% with 65% dying from congestive heart from atherosclerosis as compared to the coronary circulation, failure, -

New Insights Into the Diagnosis and Treatment of Single-Gene Disorders Associated with Cryptogenic Ischemic Stroke
New Insights Into the Diagnosis and Treatment of Single-Gene Disorders Associated With Cryptogenic Ischemic Stroke A Continuing Medical Education Monograph Release date: September 30, 2010 Expiration date: September 30, 2013 Editor Contributors Katherine B. Sims, MD Mark J. Alberts, MD, FAHA Louis R. Caplan, MD Massachusetts General Hospital Northwestern University Beth Israel Deaconess Medical Center Harvard Medical School Feinberg School of Medicine Harvard Medical School Boston, Massachusetts Northwestern Memorial Hospital Boston, Massachusetts Chicago, Illinois This activity is jointly sponsored by the University of Kentucky College of Medicine and CE Health Sciences Inc. New Insights Into the Diagnosis and Treatment of Single-Gene Disorders Associated With Cryptogenic Ischemic Stroke A Continuing Medical Education Monograph Editor Katherine B. Sims, MD Director, Developmental Neurogenetics Clinic Director, Neurogenetics DNA Diagnostic Laboratory Massachusetts General Hospital Associate Professor of Neurology Harvard Medical School Boston, Massachusetts Contributors Mark J. Alberts, MD, FAHA Professor of Neurology Section Chief, Stroke and Cerebrovascular Disease Northwestern University, Feinberg School of Medicine Director, Stroke Program Northwestern Memorial Hospital Chicago, Illinois Louis R. Caplan, MD Beth Israel Deaconess Medical Center Professor of Neurology Harvard Medical School Boston, Massachusetts To receive CME credit for this activity, please review the material in full and complete the online posttest and evaluation form at www.CECentral.com/getcredit (activity code MEN09182). A printable statement of credit will be issued upon successful completion of the required forms. 3 Accreditation This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of the University of Kentucky College of Medicine and CE Health Sciences Inc. -

Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives
International Journal of Molecular Sciences Review Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives Diji Kuriakose and Zhicheng Xiao * Development and Stem Cells Program, Monash Biomedicine Discovery Institute and Department of Anatomy and Developmental Biology, Monash University, Melbourne, VIC 3800, Australia; [email protected] * Correspondence: [email protected] Received: 29 September 2020; Accepted: 13 October 2020; Published: 15 October 2020 Abstract: Stroke is the second leading cause of death and a major contributor to disability worldwide. The prevalence of stroke is highest in developing countries, with ischemic stroke being the most common type. Considerable progress has been made in our understanding of the pathophysiology of stroke and the underlying mechanisms leading to ischemic insult. Stroke therapy primarily focuses on restoring blood flow to the brain and treating stroke-induced neurological damage. Lack of success in recent clinical trials has led to significant refinement of animal models, focus-driven study design and use of new technologies in stroke research. Simultaneously, despite progress in stroke management, post-stroke care exerts a substantial impact on families, the healthcare system and the economy. Improvements in pre-clinical and clinical care are likely to underpin successful stroke treatment, recovery, rehabilitation and prevention. In this review, we focus on the pathophysiology of stroke, major advances in the identification of therapeutic targets and recent trends in stroke research. Keywords: stroke; pathophysiology; treatment; neurological deficit; recovery; rehabilitation 1. Introduction Stroke is a neurological disorder characterized by blockage of blood vessels. Clots form in the brain and interrupt blood flow, clogging arteries and causing blood vessels to break, leading to bleeding.