Complex Characterization of Germline Large Genomic Rearrangements
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Association Weight Matrix for the Genetic Dissection of Puberty in Beef Cattle
Association weight matrix for the genetic dissection of puberty in beef cattle Marina R. S. Fortesa,b,c, Antonio Revertera,b, Yuandan Zhanga,d, Eliza Collisa,b, Shivashankar H. Nagarajb,NickN.Jonssona,c,e, Kishore C. Prayagaa,b,1, Wes Barrisa,b, and Rachel J. Hawkena,b,2 aCooperative Research Centre for Beef Genetic Technologies; bCommonwealth Scientific and Industrial Research Organization, division of Livestock Industries, Queensland Bioscience Precinct, Brisbane QLD 4067, Australia; cThe University of Queensland, School of Veterinary Science, Gatton QLD 4343, Australia; dAnimal Genetics and Breeding Unit, University of New England, Armidale NSW 2351, Australia; and eFaculty of Veterinary Medicine, University of Glasgow, Glasgow G61 1QH, United Kingdom Edited by George Seidel, Colorado State University, Fort Collins, CO, and approved June 21, 2010 (received for review February 23, 2010) We describe a systems biology approach for the genetic dissection tional data on traits related to puberty are available. For example, of complex traits based on applying gene network theory to the re- weight and condition score are often measured on occasions sults from genome-wide associations. The associations of single- throughout an animal’s development. Hence, understanding ge- nucleotide polymorphisms (SNP) that were individually associated netics of cattle puberty and its biology serves two purposes: as with a primary phenotype of interest, age at puberty in our study, a strategy to develop efficient livestock resources and as a model were explored across 22 related traits. Genomic regions were sur- for human biology. veyed for genes harboring the selected SNP. As a result, an asso- The focus of this work is to demonstrate a unique systems ap- ciation weight matrix (AWM) was constructed with as many rows proach, which we call an association weight matrix (AWM), ap- as genes and as many columns as traits. -
NBR1 (D2E6) Rabbit Mab A
Revision 1 C 0 2 - t NBR1 (D2E6) Rabbit mAb a e r o t S Orders: 877-616-CELL (2355) [email protected] Support: 877-678-TECH (8324) 1 9 Web: [email protected] 8 www.cellsignal.com 9 # 3 Trask Lane Danvers Massachusetts 01923 USA For Research Use Only. Not For Use In Diagnostic Procedures. Applications: Reactivity: Sensitivity: MW (kDa): Source/Isotype: UniProt ID: Entrez-Gene Id: WB, IP, IF-IC, F H M Endogenous 120 Rabbit IgG Q14596 4077 Product Usage Information Application Dilution Western Blotting 1:1000 Immunoprecipitation 1:50 Immunofluorescence (Immunocytochemistry) 1:1600 Flow Cytometry 1:50 Storage Supplied in 10 mM sodium HEPES (pH 7.5), 150 mM NaCl, 100 µg/ml BSA, 50% glycerol and less than 0.02% sodium azide. Store at –20°C. Do not aliquot the antibody. Specificity / Sensitivity NBR1 (D2E6) Rabbit mAb recognizes endogenous levels of total NBR1 protein. Species Reactivity: Human, Mouse Source / Purification Monoclonal antibody is produced by immunizing animals with a synthetic peptide corresponding to residues surrounding Lys601 of human NBR1 protein. Background Next to BRCA1 gene 1 (NBR1) protein is known for its encoding gene proximity to the BRCA1 tumor suppressor gene (1,2). N-terminal Phox and Bem1p (PB1) domains of NBR1 mediate its interaction with muscle specific titin kinase (3,4) and scaffolding protein p62 (4). NBR1 plays a role in autophagy by facilitating the autophagosomal degradation of ubiquitinated proteins independently and also in concert with p62 (5,6). 1. Campbell, I.G. et al. (1994) Hum Mol Genet 3, 589-94. 2. -

Datasheet: MCA3240Z Product Details
Datasheet: MCA3240Z Description: MOUSE ANTI HUMAN NBR1:Preservative Free Specificity: NBR1 Format: Preservative Free Product Type: Monoclonal Antibody Clone: 6B11 Isotype: IgG1 Quantity: 0.1 mg Product Details Applications This product has been reported to work in the following applications. This information is derived from testing within our laboratories, peer-reviewed publications or personal communications from the originators. Please refer to references indicated for further information. For general protocol recommendations, please visit www.bio-rad-antibodies.com/protocols. Yes No Not Determined Suggested Dilution Western Blotting 0.1 - 10 ug/ml Where this product has not been tested for use in a particular technique this does not necessarily exclude its use in such procedures. Suggested working dilutions are given as a guide only. It is recommended that the user titrates the product for use in their own system using appropriate negative/positive controls. Target Species Human Product Form Purified IgG - liquid Preparation Purified IgG prepared by affinity chromatography on Protein A Buffer Solution Phosphate buffered saline Preservative None present Stabilisers Approx. Protein Ig concentration 0.5 mg/ml Concentrations Immunogen Recombinant protein corresponding to aa 2-97 of human NBR1 External Database Links UniProt: Q14596 Related reagents Entrez Gene: 4077 NBR1 Related reagents Synonyms 1A13B, KIAA0049, M17S2 Page 1 of 3 Fusion Partners Spleen cells from BALB/c mice were fused with cells from the Sp2/0 myeloma cell line. Specificity Mouse anti Human NBR1 antibody, clone 6B11 recognizes human Next to BRCA1 gene 1 protein, also known as NBR1, Cell migration-inducing gene 19 protein, Membrane component chromosome 17 surface marker 2, Neighbor of BRCA1 gene 1 protein or Protein 1A1-3B. -

NBR1 Sirna (H): Sc-94187
SANTA CRUZ BIOTECHNOLOGY, INC. NBR1 siRNA (h): sc-94187 BACKGROUND SUPPORT REAGENTS NBR1 (neighbor of BRCA1 gene 1), also known as M17S2, MIG19 or 1A13B, is For optimal siRNA transfection efficiency, Santa Cruz Biotechnology’s a 966 amino acid protein that is encoded by a gene neighboring the well-char- siRNA Transfection Reagent: sc-29528 (0.3 ml), siRNA Transfection Medium: acterized tumor suppressor BRCA1. Originally thought to be the ovarian cancer sc-36868 (20 ml) and siRNA Dilution Buffer: sc-29527 (1.5 ml) are recom- antigen CA125, NBR1 contains structural motifs, including a B-box/coiled coil mended. Control siRNAs or Fluorescein Conjugated Control siRNAs are domain, an OPR domain and a ZZ-type zinc finger, that are characteristic of available as 10 µM in 66 µl. Each contain a scrambled sequence that will several proteins involved in cell transformation. NBR1 interacts with SQSTM1 not lead to the specific degradation of any known cellular mRNA. Fluorescein (sequestosome 1 protein), Titin and MuRF2 (muscle-specific RING finger pro- Conjugated Control siRNAs include: sc-36869, sc-44239, sc-44240 and tein 2), suggesting a possible role in developmental pathways. Two isoforms, sc-44241. Control siRNAs include: sc-37007, sc-44230, sc-44231, sc-44232, designated NBR1A and NBR1B, are expressed due to alternative splicing sc-44233, sc-44234, sc-44235, sc-44236, sc-44237 and sc-44238. events. Expression of both isoforms is downregulated in malignant mammary tissues, indicating that NBR1 may be involved in tumor suppression. GENE EXPRESSION MONITORING NBR1 (4BR): sc-130380 is recommended as a control antibody for monitoring REFERENCES of NBR1 gene expression knockdown by Western Blotting (starting dilution 1. -

Identification and Comprehensive Characterization of Large Genomic
Identification and comprehensive characterization of large genomic rearrangements in the and genes Jesús Valle, Lídia Feliubadaló, Marga Nadal, Alex Teulé, Rosa Miró, Raquel Cuesta, Eva Tornero, Mireia Menéndez, Esther Darder, Joan Brunet, et al. To cite this version: Jesús Valle, Lídia Feliubadaló, Marga Nadal, Alex Teulé, Rosa Miró, et al.. Identification and com- prehensive characterization of large genomic rearrangements in the and genes. Breast Cancer Re- search and Treatment, Springer Verlag, 2009, 122 (3), pp.733-743. 10.1007/s10549-009-0613-9. hal- 00535410 HAL Id: hal-00535410 https://hal.archives-ouvertes.fr/hal-00535410 Submitted on 11 Nov 2010 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Breast Cancer Res Treat (2010) 122:733–743 DOI 10.1007/s10549-009-0613-9 PRECLINICAL STUDY Identification and comprehensive characterization of large genomic rearrangements in the BRCA1 and BRCA2 genes Jesu´s del Valle • Lı´dia Feliubadalo´ • Marga Nadal • Alex Teule´ • Rosa Miro´ • Raquel Cuesta • Eva Tornero • Mireia Mene´ndez • Esther Darder • Joan Brunet • Gabriel Capella` • Ignacio Blanco • Conxi La´zaro Received: 26 August 2009 / Accepted: 20 October 2009 / Published online: 6 November 2009 Ó Springer Science+Business Media, LLC. -

Genomic Characterization of Two Large Alu-Mediated Rearrangements of the BRCA1 Gene
Journal of Human Genetics (2013) 58, 78–83 & 2013 The Japan Society of Human Genetics All rights reserved 1434-5161/13 www.nature.com/jhg ORIGINAL ARTICLE Genomic characterization of two large Alu-mediated rearrangements of the BRCA1 gene Ana Peixoto1,3, Manuela Pinheiro1,3,Lı´gia Massena2, Catarina Santos1, Pedro Pinto1, Patrı´cia Rocha1, Carla Pinto1 and Manuel R Teixeira1,2 To determine whether a large genomic rearrangement is actually novel and to gain insight about the mutational mechanism responsible for its occurrence, molecular characterization with breakpoint identification is mandatory. We here report the characterization of two large deletions involving the BRCA1 gene. The first rearrangement harbored a 89 664-bp deletion comprising exon 7 of the BRCA1 gene to exon 11 of the NBR1 gene (c.441 þ 1724_oNBR1:c.1073 þ 480del). Two highly homologous Alu elements were found in the genomic sequences flanking the deletion breakpoints. Furthermore, a 20-bp overlapping sequence at the breakpoint junction was observed, suggesting that the most likely mechanism for the occurrence of this rearrangement was nonallelic homologous recombination. The second rearrangement fully characterized at the nucleotide level was a BRCA1 exons 11–15 deletion (c.671-319_4677-578delinsAlu). The case harbored a 23 363-bp deletion with an Alu element inserted at the breakpoints of the deleted region. As the Alu element inserted belongs to a still active AluY family, the observed rearrangement could be due to an insertion-mediated deletion mechanism caused by Alu retrotransposition. To conclude, we describe the breakpoints of two novel large deletions involving the BRCA1 gene and analysis of their genomic context allowed us to gain insight about the respective mutational mechanism. -

Structure-Function Study on FIP200 Reveals Mechanistic Insights Into Selective Autophagy
Structure-function study on FIP200 reveals mechanistic insights into selective autophagy Inaugural-Dissertation to obtain the academic degree Doctor rerum naturalium (Dr. rer. nat.) submitted to the Department of Biology, Chemistry and Pharmacy of Freie Universität Berlin by Marie Witt 2019 II Examiners: Prof. Dr. Oliver Daumke Prof. Dr. Udo Heinemann Date of defense: August 8th, 2019 This thesis has been completed from October 2014 through March 2019 under the supervision of Oliver Daumke in the department of structural biology at the Max Delbrück Center in Berlin, Germany. III IV Publication Parts of this thesis have been published online in Molecular Cell on March 7, 2019: “FIP200 Claw domain binding to p62 promotes autophagosome formation at ubiquitin condensates.” Eleonora Turco*, Marie Witt*, Christine Abert*, Tobias Bock-Bierbaum*, Ming-Yuan Su*, Riccardo Trapannone, Martin Sztacho, Alberto Danieli, Xiaoshan Shi, Gabriele Zaffagnini, Annamaria Gamper, Martina Schuschnig, Dorotea Fracchiolla, Daniel Bernklau, Julia Romanov, Markus Hartl, James H. Hurley#, Oliver Daumke#, Sascha Martens# * equal contribution # senior authors Coordinates and diffraction data have been deposited in the Protein Data Bank (PDB) with accession code 6GMA. V VI Table of Contents I. List of Figures .................................................................................................................................. XI II. List of Tables ................................................................................................................................ -

Integrative Functional Analyses of the Neurodegenerative Disease-Associated TECPR2 Gene Reveal Its Diverse Roles
Integrative functional analyses of the neurodegenerative disease-associated TECPR2 gene reveal its diverse roles Ido Shalev Ben-Gurion University of the Negev Judith Somekh University of Haifa Alal Eran ( [email protected] ) Ben-Gurion University of the Negev https://orcid.org/0000-0001-6784-7597 Research article Keywords: Integrative functional analysis, neurodegenerative disorders, autophagy, ribosome, TECPR2 Posted Date: January 30th, 2020 DOI: https://doi.org/10.21203/rs.2.22274/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/23 Abstract Background Loss of tectonin β-propeller repeat-containing 2 (TECPR2) function has been implicated in an array of neurodegenerative disorders, yet its physiological function remains largely unknown. Understanding TECPR2 function is essential for developing much needed precision therapeutics for TECPR2-related diseases. Methods We leveraged the considerable amounts of functional data to obtain a comprehensive perspective of the role of TECPR2 in health and disease. We integrated expression patterns, population variation, phylogenetic proling, protein-protein interactions, and regulatory network data for a minimally biased multimodal functional analysis. Genes and proteins linked to TECPR2 via multiple lines of evidence were subject to functional enrichment analyses to identify molecular mechanisms involving TECPR2. Results TECPR2 was found to be part of a tight neurodevelopmental gene expression program that includes KIF1A, ATXN1, TOM1L2, and FA2H, all implicated in neurological diseases. Functional enrichment analyses of TECPR2-related genes converged on a role in late autophagy and ribosomal processes. Large-scale population variation data demonstrated that this role is nonredundant. Conclusions TECPR2 might serve as an indicator for the energy balance between protein synthesis and autophagy, and a marker for diseases associated with their imbalance, such as Alzheimer’s disease, Huntington’s disease, and various cancers. -

NBR1 Sirna (M): Sc-149849
SAN TA C RUZ BI OTEC HNOL OG Y, INC . NBR1 siRNA (m): sc-149849 BACKGROUND APPLICATIONS NBR1 (neighbor of BRCA1 gene 1), also known as M17S2, MIG19 or 1A13B, NBR1 siRNA (m) is recommended for the inhibition of NBR1 expression in is a 966 amino acid protein that is encoded by a gene neighboring the well- mouse cells. characterized tumor suppressor BRCA1. Originally thought to be the ovarian cancer antigen CA125, NBR1 contains structural motifs, including a B-box/ SUPPORT REAGENTS coiled-coil domain, an OPR domain and a ZZ-type zinc finger, that are charac - For optimal siRNA transfection efficiency, Santa Cruz Biotechnology’s teristic of several proteins involved in cell transformation. NBR1 interacts siRNA Transfection Reagent: sc-29528 (0.3 ml), siRNA Transfection Medium: with SQSTM1 (sequestosome 1 protein), Titin and MuRF2 (muscle-specific sc-36868 (20 ml) and siRNA Dilution Buffer: sc-29527 (1.5 ml) are recom - RING finger protein 2), suggesting a possible role in developmental path - mended. Control siRNAs or Fluorescein Conjugated Control siRNAs are ways. Two isoforms, designated NBR1A and NBR1B, are expressed due to available as 10 µM in 66 µl. Each contain a scrambled sequence that will alternative splicing events. Expression of both isoforms is downregulated in not lead to the specific degradation of any known cellular mRNA. Fluorescein malignant mammary tissues, indicating that NBR1 may be involved in tumor Conjugated Control siRNAs include: sc-36869, sc-44239, sc-44240 and suppression. sc-44241. Control siRNAs include: sc-37007, sc-44230, sc-44231, sc-44232, sc-44233, sc-44234, sc-44235, sc-44236, sc-44237 and sc-44238. -
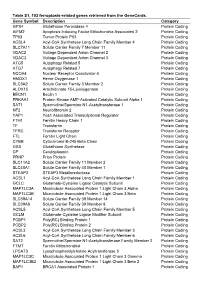
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -
Disruptions of Autophagy in the Rat Retina with Age During the Development of Age-Related-Macular- Degeneration-Like Retinopathy
International Journal of Molecular Sciences Article Disruptions of Autophagy in the Rat Retina with Age During the Development of Age-Related-Macular- Degeneration-like Retinopathy Oyuna S. Kozhevnikova * , Darya V. Telegina, Mikhail A. Tyumentsev and Nataliya G. Kolosova Institute of Cytology and Genetics, Siberian Branch of Russian Academy of Sciences (SB RAS), Pr. Lavrentyeva 10, Novosibirsk 630090, Russia * Correspondence: [email protected]; Tel.: +7-(383)-363-49-63 (ext. 4128) Received: 22 August 2019; Accepted: 23 September 2019; Published: 27 September 2019 Abstract: Age-related macular degeneration (AMD) is one of the main causes of vision impairment in the elderly. Autophagy is the process of delivery of cytoplasmic components into lysosomes for cleavage; its age-related malfunction may contribute to AMD. Here we showed that the development of AMD-like retinopathy in OXYS rats is accompanied by retinal transcriptome changes affecting genes involved in autophagy. These genes are associated with kinase activity, immune processes, and FoxO, mTOR, PI3K-AKT, MAPK, AMPK, and neurotrophin pathways at preclinical and manifestation stages, as well as vesicle transport and processes in lysosomes at the progression stage. We demonstrated a reduced response to autophagy modulation (inhibition or induction) in the OXYS retina at age 16 months: expression of genes Atg5, Atg7, Becn1, Nbr1, Map1lc3b, p62, and Gabarapl1 differed between OXYS and Wistar (control) rats. The impaired reactivity of autophagy was confirmed by a decreased number of autophagosomes under the conditions of blocked autophagosome–lysosomal fusion according to immunohistochemical analysis and transmission electron microscopy. Thus, the development of AMD signs occurs against the background of changes in the expression of autophagy-related genes and a decrease in autophagy reactivity: the ability to enhance autophagic flux in response to stress. -
NBR1 ELISA Kit (Human) (OKEH06788) Instructions for Use
NBR1 ELISA Kit (Human) (OKEH06788) Instructions for Use For the quantitative measurement of NBR1 in serum, plasma, tissue homogenates, cell culture supernatants and other biological fluids. Lot to lot variations can occur. Refer to the manual provided along with the kit. This product is intended for research use only. NBR1 ELISA Kit (Human) (OKEH06788) Contents 1. Background...................................................................................................................2 2. Assay Summary............................................................................................................3 3. Storage and Stability.....................................................................................................3 4. Kit Components ............................................................................................................3 5. Precautions ...................................................................................................................4 6. Required Materials Not Supplied ..................................................................................4 7. Technical Application Tips ............................................................................................4 8. Reagent Preparation.....................................................................................................5 9. Sample Preparation ......................................................................................................7 10. Assay Procedure...........................................................................................................8