South Sudan IDSR Annex
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

South Sudan IDSR Bulletin
South Sudan Integrated Disease Surveillance and Response (IDSR) Epidemiological Update W11 2018 (Mar 12 - Mar 18) Major Epidemiological Developments W11 2018 • Completeness for IDSR reporting at county level was 70% . Completeness for EWARS reporting from IDP sites was 81% ________________________________________________________________________ • A total of 13 alerts were reported, of which 62% have been verified. 0 alerts were risK assessed and 0 required a response. ________________________________________________________________________ • Rift Valley Fever outbreaK - Yirol East with 40 suspect human cases including 6 confirmed; 3 probable; 19 non-cases; and 12 pending classification. Nine confirmed animal cases (cattle). _________________________________________________________________________ • Following the confirmation of a measles outbreaK in Aweil East [after four measles IgM positive cases were confirmed on 24 Feb 2018], a reactive measles campaign planned targeting children 6 months to 59 months. The campaign is slated for March 26-31, 2018. _________________________________________________________________________ • In Torit, suspect meningitis continued to decline with the weeKly attacK rate remaining below the alert threshold during weeKs 11 & 12. At least 173 suspect cases including 31 deaths have been reported. During the weeK, CSF samples arrived in Paris for testing. _____________________________________________________________________________2 Surveillance| IDSR surveillance indicators • Completeness for IDSR reporting -

Aweil East County Executive Summary June 08 VF
South Sudan Preliminary Results Nutritional anthropometric and retrospective mortality surveys Children aged 6 – 59 months Aweil East County Northern Bahr El Ghazal State SOUTH SUDAN 13 th – 28 th of June 2008 Funded by: Common Humanitarian Fund (CHF) Transport Support: World Food Program (WFP) 2 INTRODUCTION Aweil East County is situated in Northern Bahr El Ghazal (NBeG) state, in Southern Sudan. It is under the Government of Southern Sudan, following the peace agreement signed in January 2005 between the government of Khartoum and the SPLM (Sudanese People Liberation Movement). NBeG is one of the smaller states of Southern Sudan but the most densely populated. It is a returnee/IDP entry point from Khartoum and Darfur. More than 40,000 returnees and 8,000 IDPs - including 27,000 returnees and 4,000 IDPs in Aweil East County 1- are reported to have arrived during the first half of 2008 alone. In 2007, 70,000 returnees were registered to have arrived in Northern Bahr el Ghazal State 2 . Aweil East County is inhabited by the Dinka ethnic group. It is composed of seven administrative payams, and each run from the north to the south, resulting in long and narrow areas. They are: Malualbai, Baac, Madhol, Mangartong, Mangok and Wunlang payams. In the rainy season, between April and September, roads are practically or completely impassable, especially in the lowlands. In January 2008, ACF-F3 took over Tearfund nutrition program in Aweil East County by keeping the Tearfund OTP 4 sites, opening a TFC 5 in Malualkon and conducting nutritional surveys. Nutritional and retrospective mortality surveys are undertaken every six months in order to estimate the malnutrition and the mortality rates. -

Enhancing People's Resilience in Northern Bahr El Ghazal, South
BRIEF / FEBRUARY 2021 Enhancing people’s resilience in Northern Bahr el Ghazal, South Sudan Northern Bahr el Ghazal, situated in the northern part The major sources of livelihoods in Northern Bahr el of South Sudan, is one of the country’s states that Ghazal are cattle rearing, small-scale agriculture and experiences fewer incidences of sub-national conflict, trade, especially in Aweil town – the capital of the state cattle raiding and revenge killings, and has experienced – and in the payams1 near to the border with Sudan. Due relatively less political violence than other states since to a long dry spell between May and July 2020, followed the eruption of civil war in South Sudan in December by heavy rains between July and September – which led 2013. to flooding in many of the state’s counties – low harvests and food insecurity are anticipated in 2021. The government of South Sudan increased the number of states in the country from ten to 32 between October Like their fellow citizens in other parts of the country, 2015 and February 2020. Northern Bahr el Ghazal was people in Northern Bahr el Ghazal are facing a dire split into two states (Aweil and Aweil East) and two of economic plight. Several factors have accentuated this its counties (Aweil North and Aweil South) were given to situation, including poor road network connections, Raja county in Western Bahr el Ghazal to form Lol state. the closure of the South Sudan-Sudan borders due to When the government reversed this decision in February disagreements over the border line, multiple taxation on 2020 and returned to the original ten states, Northern roads connecting the state to the country’s capital Juba, Bahr el Ghazal reverted to its former status. -

Aweil Centre County - Water, Sanitation and Hygiene Factsheet Northern Bahr El Ghazal State, South Sudan November/December2018
Aweil Centre County - Water, Sanitation and Hygiene Factsheet Northern Bahr el Ghazal State, South Sudan November/December2018 Overview and Methodology WASH Needs Severity Map The dynamic and multi-faceted nature of the South countrywide WASH baseline in July and August of Sudanese displacement crisis has created significant 2018 during Round 22 of the Food Security and challenges for the delivery of humanitarian aid. Nutrition Monitoring System (FSNMS). FSNMS evel 2 - Stressed Accessibility and security issues within South Sudan partners agreed to once again incorporate WASH evel 3 - Warning have impeded a systematic understanding of WASH cluster indicators for FSNMS Round 23 (November needs in many areas of the country, and have created and December of 2018). FSNMS is a seasonal evel 4 - Alert difficulties in establishing a clear and unambiguous countrywide assessment conducted, funded and run evel 5 - Emergency system for prioritizing the delivery of aid, thereby limiting by the World Food Programme, UNICEF, and the Upper Nile the effectiveness of humanitarian planning and limiting the Food and Agriculture Organization, and supported by Upp er Nile Jongle i potential impact of donor funding. As this crisis continues REACH in Round 22. FSNMS, established in 2010, is Northern Unity to expand, evolve and spill into neighbouring countries, it a representative survey that employs two-stage cluster Western Bahr el has become increasingly important to fill information gaps sampling, using a state based sample size and cluster Bahr el Ghazal Ghazal to inform a more effective humanitarian response and determination. In each county, access permitting, 9 Warrap planning for immediate life-saving WASH activities and clusters were selected and 12 households interviewed contingency planning for durable solutions. -

South Sudan IDSR Bulletin
South Sudan Integrated Disease Surveillance and Response (IDSR) Epidemiological Update W12 2018 (Mar 19- Mar 25) Major Epidemiological Developments W12 2018 • Completeness for IDSR reporting at county level was 74% . Completeness for EWARS reporting from IDP sites was 86% . ________________________________________________________________________ • A total of 16 alerts were reported, of which 75% have been verified. 0 alerts were risk assessed and 0 required a response. ________________________________________________________________________ • Rift Valley Fever outbreak - Yirol East with 43 suspect human cases including 6 confirmed; 3 probable; 19 non-cases; and 15 pending classification. Nine confirmed animal cases (cattle). _________________________________________________________________________ • A new outbreak of Rubella confirmed in Juba county after 16 Rubella IgM positive cases were confirmed in March 2018. ________________________________________________________________________ • In Torit, suspect meningitis continued to decline with no new cases in week 13 and the weekly attack rate remaining below the alert threshold in weeks 11 , 12, & 13. At least 173 suspect cases (31 deaths) reported. PCR sample testing revealed no definitive etiological pathogen. _____________________________________________________________________________ 2 Surveillance| IDSR surveillance indicators • Completeness for IDSR reporting at county level was 74% in week 12 and cumulatively at 76% for 2018 • Timeliness for IDSR reporting at county level was 74% -

[email protected], Area Mapped Logcluster Office, UNOCHA Compound and Jebel Kajur, Juba South Sudan
Sani Mingyeir Sullu Oubbe Wada`ah Djiri Bajouggi Karaw Balla Nyama Ludung Margibba Arga Gertobak Dalia Zulumingtong Gostoweir El Rahad Gyaga Manawashi En Nahud Duraysah Kurbi Karbab Godoba Silo Arid Limo Menawashei Tebeldina Kurto Kulme Gabir Futajiggi Shurab Zulata Tanako Burbur Seingo Kalamboa Uraydimah Kass Attib Deleig Kalu Dilu Shearia Shaqq Bunzuga al Gawa Galgani Duma Garoula Tangya Korgusa Garsila Kagko Khamis Abu zor Amar Seilo Ballah Umm Marabba Gedid Mogara Dauro Shalkha Harun Tumbo Qawz Beringil Lerwa Baya Saq an Na`am Buhera Sineit Goldober Singeiwa Agra Nyala Labado Sereiwa Baddal Sigeir Dilling Kirarow Tumko Umm Sa Disa Um Kurdus Shaqq Girbanat Kasoleri Buronga Gerger Saheib Mabrouka al Huja El Lait Bendisi Diri Tono Abu Mukjar Ambara Deimbo Buddu El doma Gartaga Abou Sufyan Dalami Artala Shuwayy Rashad El Roseires Um Sarir @Adid Al Muturwed Dashi Wad Abu Kubum Dago Ed Damazin Tetene Keikei Hassib Gheid Renk Nurlei Um Boim Î Damba El kharaba West Lasirei Luma Solwong Murr Njumbeil Agi Abu Ghazal Qubba Girru Ajala Um La`ota Abu Marlenga Ma'aliah 1 Jawazat Karinka Hajar Wajage Markundi Al Marwahah Abu Ma'aliah 2 Banda Dimbala 25°0'0"E 26°0'0"E 27°0'0"E 28°0'0"E 29°0'0"E 30°0'0"EUmm 31°0'0"E 32°0'0"E 33°0'0"E 34°0'0"E 35°0'0"E 36°0'0"E Timassi Ajura heitan Abu Edd el Faki Jibaiha Lujugo Milmeidi Gettin Ibrahim 42Bakau Fursan Kukur Kosua Dambar p Lagawa Sali Kulaykili Abu @ Tabanu Agabullah Adilla Wisko War e ho u se Aradeiba Gereida Manasis Anja C ap a ci t i e s 20 11 Katayla Muhajiriye Abu `Ud Heiban Um- 68Akoc Dukhun Gueighrin -

Aweil North County Squeac Assessment Report
AWEIL NORTH COUNTY SQUEAC ASSESSMENT REPORT BY MARCH 22, 2018 Report By: Jacqueline Macharia Acknowledgement This is an expression of gratitude towards the individuals and organizations that effortlessly supported the processes of this noble exercise. The 2017 SQUEAC in Aweil North County would not have been successful without their inputs. • The donor for funding the assessment • The Ministry of Health (MoH), State MoH and the County Health Department for their support and authorizing the assessment process within the community to proceed as planned • The entire Aweil North community for their patience, willingness to give information to the best of their knowledge when called upon and in allowing screening of their children. • Premiere Urgence Internationale (PUI) for providing some inputs used in triangulation being the nutrition partner in Aweil North • Concern worldwide for their inputs in planning for the assessment and mobilizing the community concerning the exercise. Thank you to the staff that went out of their way to assist during some processes for smooth running. i Table of Content Acknowledgement -------------------------------------------------------------------------------------------- i Abbreviations ------------------------------------------------------------------------------------------------ iv Executive Summary ----------------------------------------------------------------------------------------- v Introduction --------------------------------------------------------------------------------------------------- 1 -

SUDAN-SOUTH SUDAN MIGRATION CORRIDORS Relationship Between Security, Migration and Governance
SUDAN-SOUTH SUDAN MIGRATION CORRIDORS Relationship between Security, Migration and Governance SELEIM & SUDAN AWLAD HIMIED HAWAZMA AMBORORO SHANABALA RIZEIGAT & FELLATA MISSERIYA MISSERIYA CAR SOUTH SUDAN 1 Seleim Fellata Update: Rufaa • In Melut, migration is peaceful, Hawazma nomads now at Kaka heading towards Fashoda County. No families following nomads. • Arrival of Arab nomads (wk beg. 12 Nov 2012) in Gerger payam, Arabs: Renk County without prior • Naza coordination from White Nile • Sabah and Sennar of Sudan and settled • Hassania in north-west areas of Renk • Mosalami • No Ambororo presence in Renk, Fellata moved to Maban County. Concerns : • Unauthorized presence of Fellata some nomadic group in Renk. • RMG presence. Migration corridor: MEDIUM RISK LEGEND Disputed areas RETURNEE (UNS) - 66,713 (Feb RMG activity 2007-Dec 2012) REFUGEES (UNS) - 111,908 (as of 13 Migration movement 5/30/2012 2 Jan 2013) 2012 arrival location Update: Migration has not started, nomads Fellata: are proceeding towards Fashoda • Wela County from Manyo. • Futa • Gamba Concerns: RMG presence Shanabala Ambororo Hawazma Fashoda County Migration corridor: MEDIUM RISK RETURNEE (UNS) - 66,713 (Feb 2007-Dec 2012) LEGEND Disputed areas Panyikang County RMG activity Possible migration movement Main location of returnees 3 Maban County Update: • Presence of Ambororo nomads in Maban County coming from Renk. • Some Ambororo are in Longochuk County. • Nomadic refugees from BNS Potential located within short distance Refugee from main refugee camps. AreaFellata Concerns: -

Greater Bahr El Ghazal, South Sudan October - December 2018
Situation Overview: Greater Bahr el Ghazal, South Sudan October - December 2018 Figure 1: Proportion of assessed settlements Introduction. # of key informant interviews53+33+13 conducted: 1,117 an up to date understanding of current WBeG 597 humanitarian conditions and displacement reporting IDPs present in settlements, WBeG, GTA and NBeG, December 2018 Ongoing insecurity in Western Bahr el Ghazal 373 dynamics in settlements across WBeG State, 1 NBeG (WBeG) State and Greater Tonj Area (GTA) NBeG State, GTA and Gogrial East County, GTA+GE2 147 and environmental shocks in Northern Bahr Warrap State, REACH interviewed KIs who # of assessed settlements covered: 864 el Ghazal (NBeG) State and GTA continued 43+40+17+ were new arrivals in either IDP sites or 373 to drive food insecurity and limited access WBeG settlements from the area of knowledge or KIs to resources for settlements in the Greater NBeG 348 who were in contact with an individual from Bahr el Ghazal (GBeG) region from October GTA+GE 143 the assessed settlement within the last month. to December 2018. Despite the arrival of the seasonal harvest, minimal crop yields in State; Aweil North, East, South, Centre and To triangulate the findings, REACH conducted some areas due to conflict and erratic rainfall West counties in NBeG State; and Gogrial 4 Food Security and Livelihoods (FSL) focus resulted in low reported access to food in East and Tonj North, South and East counties group discussions (FGDs) and 2 Participatory assessed settlements in the GBeG region and in Warrap State. This is the first quarter Cattle Migration mapping FGDs. -

Anthropometric and Retrospective Mortality Survey Aweil East County
June 2010 Anthropometric and Retrospective Mortality Survey Aweil East County, Northern Bahr el Ghazal State Southern Sudan ACF-USA Nutrition Survey, Aweil East County, Southern Sudan, June 2010 1 Acknowledgement Action Against Hunger would like to express its deep gratitude for the support given during the Anthropometric and retrospective Mortality Survey 2010 in Aweil East County. We would like to thank ACF-USA staff, particularly the support team without which the survey wouldn’t have been possible. Furthermore, we would like to thank the survey teams, for their endurance, dedication and team spirit which enabled survey to reach the end successfully. Thanks also to all drivers who ensured timely and safe movement of the survey teams. A special thanks to the SSRRC of Aweil East County for providing vital information on the geographical areas. We finally like to say many thanks to the individual families who pleasantly allowed the survey teams measure their children and provided the survey team with the information required to make it a success. ACF-USA Nutrition Survey, Aweil East County, Southern Sudan, June 2010 2 Table of Contents Executive Summary ....................................................................................................................................................... 5 1. Introduction ......................................................................................................................................................... 7 2. Objectives of the survey ..................................................................................................................................... -

State Report Northern Bahr El Ghazal
STATE REPORT NORTHERN BAHR EL GHAZAL Village Assessments and Returnee Monitoring Analytical Report, Maps and Statistical Tables 2009 Acknowledgements The International Organization for Migration (IOM) wishes to thank its partners, the Government of National Unity (GoNU), the Government of Southern Sudan (GoSS), and particularly the Southern Sudan Relief and Rehabilitation Commission (SSRRC), for the hard work and support for the implementation of this programme. IOM also wishes to thank the United Nations Mission in Sudan (UNMIS) Protection, Return, Reintegration and Recovery (RRR). This project would not have been possible without the generous contributions and support of our donors. In this respect, IOM would like to offer its sincere appreciation to the United Nations Common Humanitarian Fund (CHF), the European Commission for Humanitarian Aid (ECHO), the Office for Disaster Assistance of the United States Agency for Development (OFDA/USAID), AusAID International Refugee Fund, the Government of Japan, and UNDP, particularly the Threat and Risk Mapping Analysis (TRMA) project. 2 Table of contents Acknowledgements ...............................................................................................................................................2 Scope of report......................................................................................................................................................4 Executive summary ...............................................................................................................................................5 -
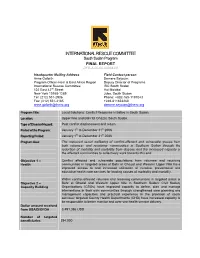
INTERNATIONAL RESCUE COMMITTEE South Sudan Program FINAL REPORT DFD-A-00-06-00068-00
INTERNATIONAL RESCUE COMMITTEE South Sudan Program FINAL REPORT DFD-A-00-06-00068-00 Headquarter Mailing Address Field Contact person Anne Goforth Demere Seyoum Program Officer-Horn & East Africa Region Deputy Director of Programs International Rescue Committee IRC South Sudan 122 East 42nd Street Hai Malakal New York 10168-1289 Juba, South Sudan Tel: (212) 551-2906 Phone: +882-165-1197043 Fax: (212) 551-3185 +249-811823260 [email protected] [email protected] Program Title: Local Solutions: Conflict Response Initiative in South Sudan. Location: Upper Nile and Bahr El Ghazal, South Sudan. Type of Disaster/Hazard: Post conflict displacement and return Period of the Program: January 1st to December 31st 2006 Reporting Period: January 1st to December 31st 2006 Program Goal The improved social wellbeing of conflict-affected and vulnerable groups from both returnee- and receiving- communities in Southern Sudan through the reduction of mortality and morbidity from disease and the increased capacity of the affected communities to collectively work towards this end. Objective 1 – Conflict affected and vulnerable populations from returnee and receiving Health communities in targeted areas of Bahr el Ghazal and Western Upper Nile have improved access to and increased utilization of curative, preventative and educative health care services for leading causes of morbidity and mortality. Within conflict-affected returnee and receiving communities in targeted areas of Objective 2 – Bahr el Ghazal and Western Upper Nile in Southern Sudan: Civil Society Capacity Building Organizations (CSOs) have improved capacity to define, plan and manage interventions in their own communities through strengthened core planning and management capacities and practical experience in the provision of social services; targeted County Health Departments (CHD) have increased capacity to be responsible to better monitor and over-see health service delivery.