Cardiac Examination Learnpediatrics.Com Narration Written by Dr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

International Journal of Medical and Health Sciences
International Journal of Medical and Health Sciences Journal Home Page: http://www.ijmhs.net ISSN:2277-4505 Review article Examining the liver – Revisiting an old friend Cyriac Abby Philips1*, Apurva Pande2 1Department of Hepatology and Transplant Medicine, PVS Institute of Digestive Diseases, PVS Memorial Hospital, Kaloor, Kochi, Kerala, India, 2Department of Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi, India. ABSTRACT In the current era of medical practice, super saturated with investigations of choice and development of diagnostic tools, clinical examination is a lost art. In this review we briefly discuss important aspects of examination of the liver, which is much needed in decision making on investigational approach. We urge the new medical student or the newly practicing physician to develop skills in clinical examination for resourceful management of the patient. KEYWORDS: Liver, examination, clinical skills, hepatomegaly, chronic liver disease, portal hypertension, liver span INTRODUCTION respiration, the excursion of liver movement is around 2 to 3 The liver attains its adult size by the age of 15 years. The cm. Castell and Frank has elegantly described normal liver liver weighs 1.2 to 1.4 kg in women and 1.4 to 1.5 kg in span in men and women utilizing the percussion method men. The liver seldom extends more than 5 cm beyond the (Table 1). Accordingly, the mean liver span is 10.5 cm for midline towards the left costal margin. During inspiration, men and 7 cm in women. During examination, a span 2 to 3 the diaphragmatic exertion moves the liver downward with cm larger or smaller than these values is considered anterior surface rotating to the right. -
General Physical Examination Skills for Ahps
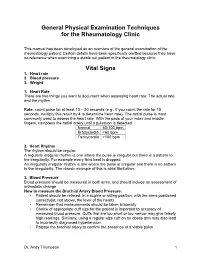
General Physical Examination Techniques for the Rheumatology Clinic This manual has been developed as an overview of the general examination of the rheumatology patient. Certain details have been specifically omitted because they have no relevance when examining a stable out patient in the rheumatology clinic. Vital Signs 1. Heart rate 2. Blood pressure 3. Weight 1. Heart Rate There are two things you want to document when assessing heart rate: The actual rate and the rhythm. Rate: count pulse for at least 15 – 30 seconds (e.g., if you count the rate for 15 seconds, multiply this result by 4 to determine heart rate). The radial pulse is most commonly used to assess the heart rate. With the pads of your index and middle fingers, compress the radial artery until a pulsation is detected. Normal 60-100 bpm Bradycardia <60 bpm Tachycardia >100 bpm 2. Heart Rhythm The rhythm should be regular. A regularly irregular rhythm is one where the pulse is irregular but there is a pattern to the irregularity. For example every third beat is dropped. An irregularly irregular rhythm is one where the pulse is irregular and there is no pattern to the irregularity. The classic example of this is atrial fibrillation. 3. Blood Pressure Blood pressure should be measured in both arms, and should include an assessment of orthostatic change How to measure the Brachial Artery Blood Pressure: • Patient should be relaxed, in a supine or sitting position, with the arms positioned correctly(at, not above, the level of the heart) • Remember that measurements should be taken bilaterally • Choice of appropriate cuff size for the patient is important to accuracy of measured blood pressure. -

The Older Adult 20
CHAPTER The Older Adult 20 Older adults now number more than 25 million people in the United States and are expected to reach 80 million by 2050.1 These seniors will live longer than previous generations: life span at birth is currently 79 years for women and 74 years for men. Those older than 85 years are projected to increase to 5% of the U.S. population within 40 years. Hence, the “demographic im- perative” is to maximize not only the life span but also the “health span” of our older population, so that seniors maintain full function for as long as possible, enjoying rich and active lives in their homes and communities. Clinicians now recognize frailty as one of society’s common myths about aging—more than 95% of Americans older than 65 years live in the commu- nity, and only 5% reside in long-term care facilities.1,2 Over the past 20 years, seniors actually have become more active and less disabled. These changes call for new goals for clinical care—“an informed activated patient inter- acting with a prepared proactive team, resulting in high quality satisfying en- counters and improved outcomes”3—and a distinct set of clinical attitudes and skills. CHAPTER 20 I THE OLDER ADULT 839 ANATOMY AND PHYSIOLOGY Assessing the older adult presents special opportunities and special challenges. Many of these are quite different from the disease-oriented approach of his- tory taking and physical examination for younger patients: the focus on healthy or “successful” aging; the need to understand and mobilize family, social, and community supports; the importance of skills directed to func- tional assessment, “the sixth vital sign”; and the opportunities for promoting the older adult’s long-term health and safety. -

Practical Cardiac Auscultation
LWW/CCNQ LWWJ306-08 March 7, 2007 23:32 Char Count= Crit Care Nurs Q Vol. 30, No. 2, pp. 166–180 Copyright c 2007 Wolters Kluwer Health | Lippincott Williams & Wilkins Practical Cardiac Auscultation Daniel M. Shindler, MD, FACC This article focuses on the practical use of the stethoscope. The art of the cardiac physical exam- ination includes skillful auscultation. The article provides the author’s personal approach to the patient for the purpose of best hearing, recognizing, and interpreting heart sounds and murmurs. It should be used as a brief introduction to the art of auscultation. This article also attempts to illustrate heart sounds and murmurs by using words and letters to phonate the sounds, and by presenting practical clinical examples where auscultation clearly influences cardiac diagnosis and treatment. The clinical sections attempt to go beyond what is available in standard textbooks by providing information and stethoscope techniques that are valuable and useful at the bedside. Key words: auscultation, murmur, stethoscope HIS article focuses on the practical use mastered at the bedside. This article also at- T of the stethoscope. The art of the cardiac tempts to illustrate heart sounds and mur- physical examination includes skillful auscul- murs by using words and letters to phonate tation. Even in an era of advanced easily avail- the sounds, and by presenting practical clin- able technological bedside diagnostic tech- ical examples where auscultation clearly in- niques such as echocardiography, there is still fluences cardiac diagnosis and treatment. We an important role for the hands-on approach begin by discussing proper stethoscope selec- to the patient for the purpose of evaluat- tion and use. -

Bates' Pocket Guide to Physical Examination and History Taking
Lynn S. Bickley, MD, FACP Clinical Professor of Internal Medicine School of Medicine University of New Mexico Albuquerque, New Mexico Peter G. Szilagyi, MD, MPH Professor of Pediatrics Chief, Division of General Pediatrics University of Rochester School of Medicine and Dentistry Rochester, New York Acquisitions Editor: Elizabeth Nieginski/Susan Rhyner Product Manager: Annette Ferran Editorial Assistant: Ashley Fischer Design Coordinator: Joan Wendt Art Director, Illustration: Brett MacNaughton Manufacturing Coordinator: Karin Duffield Indexer: Angie Allen Prepress Vendor: Aptara, Inc. 7th Edition Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2009 by Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2007, 2004, 2000 by Lippincott Williams & Wilkins. Copyright © 1995, 1991 by J. B. Lippincott Company. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appear- ing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at Two Commerce Square, 2001 Market Street, Philadelphia PA 19103, via email at [email protected] or via website at lww.com (products and services). 9 8 7 6 5 4 3 2 1 Printed in China Library of Congress Cataloging-in-Publication Data Bickley, Lynn S. Bates’ pocket guide to physical examination and history taking / Lynn S. -

1. Intermittent Chest Pain: Angina: • Stable: (Caused By
CVS: 1. Intermittent chest pain: Angina: • Stable: (caused by chronic narrowing in one or more coronary arteries), episodes of pain are precipitated by exertion and may occur more readily when walking in cold or windy weather, after a large meal or while carrying a heavy load; the pain is promptly relieved by rest and/or sublingual glyceryl nitrate (GTN) spray, and typically lasts for less than 10 minutes. • unstable angina (caused by a sudden severe narrowing in a coronary artery), there is usually an abrupt onset or worsening of chest pain episodes that may occur on minimal exertion or at rest. • Retrosternal/ Progressive onset/ increase in intensity over 1–2 minutes/ Constricting, heavy/ Sometimes arm(s), neck, epigastrium/ Associated with breathlessness/ Intermittent, with episodes lasting 2–10 minutes/ Triggered by emotion, exertion, especially if cold, windy/ Relieved by rest, nitrates Mild to moderate. • Aggravated by thyroxine or drug-induced anemia, e.g. aspirin or NSAIDs Esophageal: • Retrosternal or epigastric/ Over 1–2 minutes; can be sudden (spasm)/ C: Gripping, tight or burning/ R: Often to back, sometimes to arms/ A: Heartburn, acid reflux/ T: Intermittent, often at night-time; variable duration/ Lying flat/some foods may trigger/ Not relieved by rest; nitrates sometimes relieve/ Usually mild but esophageal spasm can mimic myocardial infarction. 2. Acute chest pain: MI: • SOCRATES: Retrosternal/ Rapid over a few minutes/ Constricting, heavy/ Often to arm(s), neck, jaw, sometimes epigastrium/ Sweating, nausea, vomiting, breathlessness, feeling of impending death (angor animi)/ Acute presentation; prolonged duration/ ’Stress’ and exercise rare triggers, usually spontaneous/ Not relieved by rest or nitrates/ Usually severe. -

Scoliosis, Alters the Position of the Beat
Br Heart J: first published as 10.1136/hrt.8.3.162 on 1 July 1946. Downloaded from THE HEART IN STERNAL DEPRESSION BY WILLIAM EVANS From the Cardiac Department ofthe London Hospital Received June 25, 1946 The place where the apex beat appears on the chest wall depends as much on the symmetry of the thorax as on the size of the heart. A change in the alignment of the spine, the posterior fulcrum of the thoracic cage, in the form of scoliosis, alters the position of the beat. Local deformity of the ribs which form the walls of the cage will do the same thing. Deformity of the sternum, the anterior fulcrum of the thorax, as a cause of displacement of the apex beat has received less attention. The effects of depression of the sternum (pectus excavatum) on the shape and position of the heart have been studied in sixteen adults examined during the past year. DESCRIPTION OF CASES All sixteen patients had been referred for an explanation of certain signs connected with the heart, with the knowledge that deformity of the chest was present, but without appreciating that the two conditions might be related. In many of them suspicion of heart disease had led to restriction of their physical activities and to a change of design for their future livelihood. The symptoms that had caused the patients to seek medical advice in the first place were http://heart.bmj.com/ TABLE I SUMMARY OF FINDNGS IN 16 HEALTHY SUBJECTS WITH DEPRESSED STERNUM Antero-posterior Radiological findings in anterior view chest measurement _ _ Case Age Sternal in inches No. -

GUIDELINES for WRITING SOAP NOTES and HISTORY and PHYSICALS
GUIDELINES FOR WRITING SOAP NOTES and HISTORY AND PHYSICALS by Lois E. Brenneman, M.S.N, C.S., A.N.P, F.N.P. © 2001 NPCEU Inc. all rights reserved NPCEU INC. PO Box 246 Glen Gardner, NJ 08826 908-537-9767 - FAX 908-537-6409 www.npceu.com Copyright © 2001 NPCEU Inc. All rights reserved No part of this book may be reproduced in any manner whatever, including information storage, or retrieval, in whole or in part (except for brief quotations in critical articles or reviews), without written permission of the publisher: NPCEU, Inc. PO Box 246, Glen Gardner, NJ 08826 908-527-9767, Fax 908-527-6409. Bulk Purchase Discounts. For discounts on orders of 20 copies or more, please fax the number above or write the address above. Please state if you are a non-profit organization and the number of copies you are interested in purchasing. 2 GUIDELINES FOR WRITING SOAP NOTES and HISTORY AND PHYSICALS Lois E. Brenneman, M.S.N., C.S., A.N.P., F.N.P. Written documentation for clinical management of patients within health care settings usually include one or more of the following components. - Problem Statement (Chief Complaint) - Subjective (History) - Objective (Physical Exam/Diagnostics) - Assessment (Diagnoses) - Plan (Orders) - Rationale (Clinical Decision Making) Expertise and quality in clinical write-ups is somewhat of an art-form which develops over time as the student/practitioner gains practice and professional experience. In general, students are encouraged to review patient charts, reading as many H/Ps, progress notes and consult reports, as possible. In so doing, one gains insight into a variety of writing styles and methods of conveying clinical information. -

5 Precordial Pulsations
Chapter 5 / Precordial Pulsations 113 5 Precordial Pulsations CONTENTS MECHANICS AND PHYSIOLOGY OF THE NORMAL APICAL IMPULSE PHYSICAL PRINCIPLES GOVERNING THE FORMATION OF THE APICAL IMPULSE NORMAL APICAL IMPULSE AND ITS DETERMINANTS ASSESSMENT OF THE APICAL IMPULSE LEFT PARASTERNAL AND STERNAL MOVEMENTS RIGHT PARASTERNAL MOVEMENT PULSATIONS OVER THE CLAVICULAR HEADS PULSATIONS OVER THE SECOND AND/OR THIRD LEFT INTERCOSTAL SPACES SUBXIPHOID IMPULSE PRACTICAL POINTS IN THE CLINICAL ASSESSMENT OF PRECORDIAL PULSATIONS REFERENCES In this chapter the pulsations of the precordium will be discussed in relation to their identification, the mechanisms of their origin, and their pathophysiological and clinical significance. Precordial pulsations include the “apical impulse,” left parasternal movement, right parasternal movement, pulsations of the clavicular heads, pulsations over the second left intercostal space, and subxiphoid impulses. MECHANICS AND PHYSIOLOGY OF THE NORMAL APICAL IMPULSE Since during systole the heart contracts, becoming smaller and therefore moving away from the chest wall, why should one feel a systolic outward movement (the apical impulse) at all? Logically speaking there should not be an apical impulse. Several different methods of recording the precordial motion have been used to study the apical impulse going back to the late 19th century (1,2). Among the more modern methods, the notable ones are the recordings of the apexcardiogram (3–17), the impulse cardiogram (18), and the kinetocardiogram (19–21). While apexcardiography records the relative displacement of the chest wall under the transducer pickup device, which is often held by the examiner’s hands, the proponents of the impulse cardiography and kinetocardiography point out that these methods allow the recording of the absolute movement of the chest wall because the pickup device is anchored to a fixed point held 113 114 Cardiac Physical Examination in space away from the chest. -

Topic: MITRAL HEART DISEASES: BASIC SYMPTOMS and SYNDROMES on the BASIS of CLINICAL and INSTRUMENTAL METHODS of EXAMINATION
Topic: MITRAL HEART DISEASES: BASIC SYMPTOMS AND SYNDROMES ON THE BASIS OF CLINICAL AND INSTRUMENTAL METHODS OF EXAMINATION 1. What hemodynamic changes cause complaints of patients with mitral stenosis for cough, shortness of breath, hemoptysis? A. reduction of systemic blood pressure; B. increased pressure in the small circulatory system; C. stagnation of blood in the liver; D. enlargement of the left atrium and contraction of the mediastinum; E. Reduction of blood flow from the left ventricle. 2. What complaints are caused by a decrease in minute volume of blood in patients with mitral stenosis? A) cough, shortness of breath, hemoptysis; C) fever, joint pain, general weakness; C) heartache, heart failure, palpitations; D) lower extremity swelling, heaviness in the right hypochondrium; E) headache, dizziness, general weakness, fatigue. 3. Data palpation of the heart area with mitral stenosis: A) no change is observed; B) apex beat displaced to the left, resistant; C) apex beat weakened or undetectable; D) there is an increased pulsation in the second intercostal space to the left; E) there is a systolic "cat murmur" in the second intercostal space to the right. 4. What forced position can occupy a patient with mitral stenosis? A) knee-elbow; B) a Bedouin who prays; C) orthopnoe; D) opistotonus; E) outside the pointing dog 5. What does the face of a patient with mitral stenosis look like? A) swollen, cyanotic; B) swollen, pale, enophthalmos observed; C) the face of a "wax doll"; D) swollen, pale, with swelling under and above the eyes; E) pale, with cyanotic blush, cyanosis of the tip of the nose, ear lobes, chin. -

Accuracy and Reliability of Palpation and Percussion for Detecting Hepatomegaly: a Rural Hospital-Based Study
Accuracy and reliability of palpation and percussion for detecting hepatomegaly: a rural hospital-based study Rajnish Joshi, Amandeep Singh, Namita Jajoo, Madhukar Pai,* S P Kalantri Department of Medicine, Mahatma Gandhi Institute of Medical Sciences, Sevagram 442 102, Maharashtra; and *Division of Epidemiology, University of California at Berkeley, Berkeley, CA 94720, USA Background: Palpation and percussion are standard Although many physicians believe that physical bedside techniques used to diagnose hepatomegaly. examination can accurately identify hepatomegaly, some Ultrasonography is a noninvasive and accurate method published reports suggest that physical signs lack accu- for measurement of liver size, but many patients in racy and reliability.1,2,3 To our knowledge, no study from developing countries have limited access to it. We India has evaluated the accuracy of physical examina- compared the accuracy of palpation and percussion tion in the assessment of enlarged liver. We conducted in a rural population in central India, using this study to determine how accurately doctors can ultrasonography as a reference standard. Methods: distinguish an enlarged liver from a normal sized one, The study design was a blinded, cross-sectional analysis and how often they agree with one another while as- of a hospital-based case series. Three physicians, sessing liver size. blind to clinical data and to each others results, independently used palpation and percussion to detect Methods hepatomegaly. Diagnostic accuracy was measured by We enrolled consecutive patients admitted to the Medi- computing sensitivity, specificity, and likelihood ratio cine wards between February 1 and 15, 2003. Patients values. Inter-physician agreement was assessed using with pleural diseases (effusion or pneumothorax) or the kappa statistic. -

CARDIOLOGY Section Editors: Dr
2 CARDIOLOGY Section Editors: Dr. Mustafa Toma and Dr. Jason Andrade Aortic Dissection DIFFERENTIAL DIAGNOSIS PATHOPHYSIOLOGY (CONT’D) CARDIAC DEBAKEY—I ¼ ascending and at least aortic arch, MYOCARDIAL—myocardial infarction, angina II ¼ ascending only, III ¼ originates in descending VALVULAR—aortic stenosis, aortic regurgitation and extends proximally or distally PERICARDIAL—pericarditis RISK FACTORS VASCULAR—aortic dissection COMMON—hypertension, age, male RESPIRATORY VASCULITIS—Takayasu arteritis, giant cell arteritis, PARENCHYMAL—pneumonia, cancer rheumatoid arthritis, syphilitic aortitis PLEURAL—pneumothorax, pneumomediasti- COLLAGEN DISORDERS—Marfan syndrome, Ehlers– num, pleural effusion, pleuritis Danlos syndrome, cystic medial necrosis VASCULAR—pulmonary embolism, pulmonary VALVULAR—bicuspid aortic valve, aortic coarcta- hypertension tion, Turner syndrome, aortic valve replacement GI—esophagitis, esophageal cancer, GERD, peptic OTHERS—cocaine, trauma ulcer disease, Boerhaave’s, cholecystitis, pancreatitis CLINICAL FEATURES OTHERS—musculoskeletal, shingles, anxiety RATIONAL CLINICAL EXAMINATION SERIES: DOES THIS PATIENT HAVE AN ACUTE THORACIC PATHOPHYSIOLOGY AORTIC DISSECTION? ANATOMY—layers of aorta include intima, media, LR+ LRÀ and adventitia. Majority of tears found in ascending History aorta right lateral wall where the greatest shear force Hypertension 1.6 0.5 upon the artery wall is produced Sudden chest pain 1.6 0.3 AORTIC TEAR AND EXTENSION—aortic tear may Tearing or ripping pain 1.2–10.8 0.4–0.99 produce