Antimicrobial Resistance – Implications for New Zealanders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Contents More Information
Cambridge University Press 978-0-521-86297-4 - Horizontal Gene Transfer in the Evolution of Pathogenesis Edited by Michael Hensel and Herbert Schmidt Table of Contents More information Contents ix Preface page xi Contributors xv PART I Theoretical Considerations on the Evolution of Bacterial Pathogens 1 Genomes in Motion: Gene Transfer as a Catalyst for Genome Change 3 Jeffrey G. Lawrence and Heather Hendrickson 2 Bacterial Recombination in vivo 23 Xavier Didelot and Daniel Falush PART II Mobile Genetic Elements in Bacterial Evolution 3 Phage-bacterium Co-evolution and Its Implication for Bacterial Pathogenesis 49 Harald Brussow¨ 4 The Role of Bacteriophages in the Generation and Spread of Bacterial Pathogens 79 Roger W. Hendrix and Sherwood R. Casjens 5 Genomic Islands in the Bacterial Chromosome – Paradigms of Evolution in Quantum Leaps 113 Tobias Olschl¨ ager¨ and Jorg¨ Hacker PART III Paradigms of Bacterial Evolution 6 Genomic Islands in Plant-pathogenic Bacteria 137 Dawn L. Arnold and Robert W. Jackson © Cambridge University Press www.cambridge.org Cambridge University Press 978-0-521-86297-4 - Horizontal Gene Transfer in the Evolution of Pathogenesis Edited by Michael Hensel and Herbert Schmidt Table of Contents More information 7 Prophage Contribution to Salmonella Virulence and Diversity 159 Sebastien´ Lemire, Nara Figueroa-Bossi, and Lionello Bossi 8 Pathogenic Yersinia: Stepwise Gain of Virulence due to Sequential Acquisition of Mobile Genetic Elements 193 Elisabeth Carniel 9 Genomic or Pathogenicity Islands in Streptococcus pneumoniae 217 Barbara Albiger, Christel Blomberg, Jessica Dagerhamn, Staffan Normark, and Birgitta Henriques-Normark 10 The Mobile Genetic Elements of Staphylococcus aureus 237 Richard P. -

1 Webster Centre-QRW Programme National Symposium on Infectious Diseases: Key Opportunities and Emerging Therapies 7-8Th Septemb
Webster Centre-QRW Programme National Symposium on Infectious Diseases: key opportunities and emerging therapies 7-8th September, 2017 Rydges Hotel, Queenstown, New Zealand Thursday 7th September Time Details LoCation 8:45 – 8:55 am S1: IntroduCtion and opening remarks Andy MerCer – Webster Centre and One Health Aotearoa, University of Otago Session sponsored by One Health Aotearoa and Webster Centre, University of Otago 8:55 – 9.30 am Plenary talk: Professor Elizabeth Hartland Department of Microbiology and Immunology, University of Melbourne “Legionella intracellular replication” 9:30 – 10.00 am Nigel French, Massey University “Genomic anatomy of slow-burn epidemics” 10.00 – 10.30 am Morning Tea S2: Genomic approaches to Combat infeCtious disease Chair: James Ussher 10.30 – 11.00 am Deborah Williamson, Peter Doherty Institute for InfeCtion and Immunity “Applying genomics to outbreak investigations” 11.00 – 11.30am Professor David MurdoCh University of Otago, ChristchurCh Sponsored by New Zealand Food Safety Science & Research Centre “Infectious Diseases within an Increasingly Connected Ecosystem” 11.30 – 12.00pm Htin Aung University of Otago, Dunedin “Whole-genome sequencing for the management of drug-resistant tuberculosis in Myanmar” 12.00 – 12.30pm Mike Taylor, University of AuCkland “Bacterial community collapse: the microbiome in chronic sinus disease” 12.30 – 1.30pm Lunch 1 S3: Fighting BaCk: drug disCovery, AMR and vaccines Chair: Tim Stinear Plenary Talk: Professor John BlanChard 1.30 – 2.15pm Department of Biochemistry, Albert -

Pharmac Session: Antimicrobial Resistance - Global Threat Or Myth? (120Mins, Not Repeated) Antibiotic Resistance Mutations Or Creations? How We Squander a Miracle
Associate Professor Associate Professor David Holland Siouxsie Wiles Director Microbiologist Infection Services Head of the Bioluminescent Superbugs Lab Middlemore Hospital University of Auckland Professor Jack Mr Ben Harris Dr Peter Moodie Heinemann Honorary Lecturer General Practitioner University of Otago Wellington Genetics and Molecular Biology School of Biological Sciences University of Canterbury 14:00 - 16:00 WS #155: Pharmac Session: Antimicrobial Resistance - Global Threat or Myth? (120mins, not repeated) Antibiotic Resistance Mutations or Creations? How We Squander a Miracle Ben Harris, Medical Microbiology Scientist NZ Infection Prevention Control Consultancy [email protected] M: 0276273201 “We are not there to be phased by a brilliant international conference speaker we are there because we are gullible, ignorant & desperate” REFERENCE: Written comment from veteran GP regarding the didactic style that he finds most useful at GP CME “We are not there to be phased by a brilliant international conference speaker we are there because we are gullible, ignorant & desperate” Antibiotic Key Point On NZ average Prescribe well under 50% antibiotics you currently prescribe Because ➢ Reduce increasing MDRO endemicity ➢ Keep rapidly dwindling AB resource reserved for future serious infections ➢ Each AB use increases that patients medium to long term adverse chronic health outcomes Tips to Achieve This • Respiratory - follow BPAC guidelines • UTI – adults, clinical diagnosis, ban dipsticks • Cutaneous – lance abscess, no prophylactic -

Dynamics and Genetic Diversification of Escherichia Coli During Experimental Adaptation to an Anaerobic Environment
Dynamics and genetic diversification of Escherichia coli during experimental adaptation to an anaerobic environment Thomas J. Finn1,2,3, Sonal Shewaramani1,2,4, Sinead C. Leahy1, Peter H. Janssen1 and Christina D. Moon1 1 Grasslands Research Centre, AgResearch Ltd, Palmerston North, New Zealand 2 New Zealand Institute for Advanced Study, Massey University, Auckland, New Zealand 3 Department of Biochemistry, University of Otago, Dunedin, New Zealand 4 Department of Molecular and Cell Biology, University of Connecticut, Storrs, CT, United States of America ABSTRACT Background. Many bacteria are facultative anaerobes, and can proliferate in both anoxic and oxic environments. Under anaerobic conditions, fermentation is the primary means of energy generation in contrast to respiration. Furthermore, the rates and spectra of spontaneous mutations that arise during anaerobic growth differ to those under aerobic growth. A long-term selection experiment was undertaken to investigate the genetic changes that underpin how the facultative anaerobe, Escherichia coli, adapts to anaerobic environments. Methods. Twenty-one populations of E. coli REL4536, an aerobically evolved 10,000th generation descendent of the E. coli B strain, REL606, were established from a clonal ancestral culture. These were serially sub-cultured for 2,000 generations in a defined minimal glucose medium in strict aerobic and strict anaerobic environments, as well as in a treatment that fluctuated between the two environments. The competitive fitness of the evolving lineages was assessed at approximately 0, 1,000 and 2,000 generations, in both the environment of selection and the alternative environment. Whole genome re-sequencing was performed on random colonies from all lineages after 2,000-generations. -

Amplification–Mutagenesis: Evidence That ‘‘Directed’’ Adaptive Mutation and General Hypermutability Result from Growth with a Selected Gene Amplification
Amplification–mutagenesis: Evidence that ‘‘directed’’ adaptive mutation and general hypermutability result from growth with a selected gene amplification Heather Hendrickson*†, E. Susan Slechta*, Ulfar Bergthorsson*, Dan I. Andersson‡, and John R. Roth*§ *Department of Biology, University of Utah, Salt Lake City, UT 84112; and ‡Swedish Institute for Infectious Disease Control, S 17182 Solna, Sweden Communicated by Nancy Kleckner, Harvard University, Cambridge, MA, December 18, 2001 (received for review September 9, 2001) When a particular lac mutant of Escherichia coli starves in the presence We have suggested (9) that apparently directed mutation of lactose, nongrowing cells appear to direct mutations preferentially could be explained if the leaky lac allele used in this experiment to sites that allow growth (adaptive mutation). This observation were amplified so as to allow slow growth of a clone on lactose. suggested that growth limitation stimulates mutability. Evidence is Reversion would then occur when the growing clone has accu- provided here that this behavior is actually caused by a standard mulated enough mutant lac copies. What appears to be a Darwinian process in which natural selection acts in three sequential directed single step mutation in a nongrowing cell can result steps. First, growth limitation favors growth of a subpopulation with from selection acting on growing cells within a colony. The ؉ an amplification of the mutant lac gene; next, it favors cells with a lac required growth will not be evident in the lawn between colonies, revertant allele within the amplified array. Finally, it favors loss but can be revealed by appropriate analysis of developing ؉ of mutant copies until a stable haploid lac revertant arises and colonies (9). -

Friday, July 10, 2020 Home-Delivered $1.90, Retail $2.20
TE NUPEPA O TE TAIRAWHITI FRIDAY, JULY 10, 2020 HOME-DELIVERED $1.90, RETAIL $2.20 LANDFILL BREACH STAR PAGES 3, 6-8, 10 ANOTHER WAKE-UP CALL OF GLEE COVID-19NEW 12-13, 20 PAGE 5 MISSING, • PBL Helen Clark heading Covid-19 response panel PRESUMED • Police to be posted at all managed isolation facilities DROWNED •PAGE Poor 3 response in US blamed on ‘anti-science bias’ • Covid-19 worldwide cases passes 12 million PAGE 12 SNOWDUST: Daytime maximum temperatures across Tairawhiti struggled to reach 11 degrees yesterday as the cold southerly brought a sprinkling of snow to the top of Mount Hikurangi — captured on camera by Sam Spencer. “We’re well and truly into the midst of winter now and yesterday sure would have felt like it,” said a MetService forecaster. “The dewpoint temperature (measure of moisture in air) was around zero degrees when the maximum air temperature was recorded. “The average daily maximum for Gisborne in July is around 15 degrees. “So it’s colder than average but it will need to drop a few more degrees to get into record books.” The district avoided the forecast frost overnight due to cloud cover, but MetService predicts 1 degree at Gisborne Airport tomorrow morning. by Matai O’Connor British High Commissioner to recovery,” she said. “Individuals New Zealand Laura Clarke, and organisations across TOITU Tairawhiti, a and Te Whanau o Waipareira Tairawhiti, including iwi, all collective of local iwi, have chief executive John Tamihere did a great job. organised a two-day summit to and Director-General of Health “We want to benchmark and reflect on the region’s response Dr Ashley Bloomfield. -

Title 1 Ribosome Provisioning Activates a Bistable Switch
bioRxiv preprint doi: https://doi.org/10.1101/244129; this version posted April 24, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Title 2 Ribosome provisioning activates a bistable switch coupled to fast exit from stationary 3 phase 4 5 Authors: 6 P. Remigi1*, G.C. Ferguson2, S. De Monte3,4 and P.B. Rainey1,5,6* 7 1 New Zealand Institute For Advanced Study, Massey University, AucKland 0745, New 8 Zealand 9 2 Institute oF Natural and Mathematical Sciences, Massey University, AucKland 0745, New 10 Zealand 3 11 Institut de biologie de l’Ecole normale supérieure (IBENS), Ecole normale supérieure, CNRS, 12 INSERM, PSL Université Paris 75005 Paris, France 13 4 Department oF Evolutionary Theory, Max PlancK Institute For Evolutionary Biology, Plön 14 24306, Germany 15 5 Department oF Microbial Population Biology, Max PlancK Institute For Evolutionary Biology, 16 Plön 24306, Germany 6 17 Ecole Superieure de Physique et de Chimie Industrielles de la Ville de Paris (ESPCI Paris 18 Tech), CNRS UMR 8231, PSL Research University, 75231 Paris, France 19 20 * Corresponding authors: 21 Philippe Remigi ([email protected]) and Paul B. Rainey ([email protected]) 22 bioRxiv preprint doi: https://doi.org/10.1101/244129; this version posted April 24, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 23 Abstract: 24 Observations oF bacteria at the single-cell level have revealed many instances oF phenotypic 25 heterogeneity within otherwise clonal populations, but the selective causes, molecular bases 26 and broader ecological relevance remain poorly understood. -
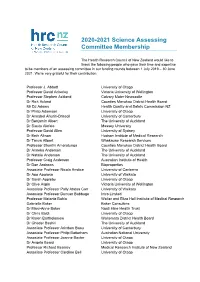
2020-2021 Science Assessing Committee Membership
2020-2021 Science Assessing Committee Membership The Health Research Council of New Zealand would like to thank the following people who gave their time and expertise to be members of an assessing committee in our funding rounds between 1 July 2019 – 30 June 2021. We’re very grateful for their contribution. Professor J. Abbott University of Otago Professor David Ackerley Victoria University of Wellington Professor Stephen Ackland Calvary Mater Newcastle Dr Rick Acland Counties Manukau District Health Board Mr DJ Adams Health Quality and Safety Commission NZ Dr Philip Adamson University of Otago Dr Annabel Ahuriri-Driscoll University of Canterbury Dr Benjamin Albert The University of Auckland Dr Siautu Alefaio Massey University Professor David Allen University of Sydney Dr Beth Allison Hudson Institute of Medical Research Dr Tanya Allport Whakauae Research Services Professor Shanthi Ameratunga Counties Manukau District Health Board Dr Anneka Anderson The University of Auckland Dr Natalie Anderson The University of Auckland Professor Craig Anderson Australian Institute of Health Dr Dan Andrews Bioproperties Associate Professor Nicola Anstice University of Canberra Dr Apo Aporosa University of Waikato Dr Sarah Appleby University of Otago Dr Clive Aspin Victoria University of Wellington Associate Professor Polly Atatoa Carr University of Waikato Associate Professor Duncan Babbage Intro Limited Professor Melanie Bahlo Walter and Eliza Hall Institute of Medical Research Gabrielle Baker Baker Consulting Dr Mary-Anne Baker Ngati Hine Health Trust -

Impact Innovation
#ASC14 BRISBANE February 2-5, 2014 INSIGHT IMPACT INNOVATION National Conference 2014 PROGRAM HANDBOOK www.ascconference.info 2 Organising committee Claire Harris Kali Madden Contents Jesse Shore Rod Lamberts Program committee Kali Madden Claire Harris Sponsors 3 Nancy Longnecker Jesse Shore Welcome messages 4 Social events committee Kali Madden Claire Harris 2014 and icons explained Andrew Stephenson 7 Kate Patterson Peter Wheeler Christine Ross Event highlights 8 SEQ ASC Branch Promotions and media committee General information 10 Claire Harris Kali Madden Sarah Lau Michelle Wheeler Social media policy 11 Kylie Sturgess Simon Chester James Hardy Sunday at a glance 13 Victoria Leitch Joan Leach John Harrison Monday at a glance 14 Andrew Wight Kate Hodge Students from The University of Queensland, Science Communication Tuesday at a glance 16 Peer reviewers Lindy Orthia Australian National University Wednesday at a glance 18 Will Grant Australian National University Vicky Martin Southern Cross University John O’Connor University of Newcastle Nancy Longnecker University of Western Australia Thursday at a glance 20 Emma Bartle University of Queensland Muza Gondwe University of Western Australia Will Rifkin University of Queensland Speaker and delegate index 21 Miriam Sullivan University of Western Australia Jennifer Manyweathers University of Western Australia Jenni Metcalfe Econnect Communication Venue and Brisbane maps 54 Jenny Donovan University of Southern Queensland Jean Fletcher University of Western Australia Volunteers Notes 56 Melanie McKenzie: evaluation Alex Jurkiewicz, website management Heidi Jones and others! Conference management Justin Holsinger and Melissa Batterbee from Eventcorp 3 HOSTED BY SPONSORS Silver WiFi Bronze Dinner Science Storytelling Event SUPPORTERS 4 PRESIDENT’S WELCOME As President of the Australian Science Communicators, I want to welcome you to my home city of Brisbane and to ASC2014. -
Lessons from the Pandemic: an Australasian Perspective
Lessons from the pandemic: an Australasian perspective 2nd Open Science Conference July 21-23, 2021 Dr Ginny Barbour Director, Open Access Australasia 28 universities across Australia & New Zealand, Creative Commons Australia & Tohatoha Aotearoa Commons Chair of Executive Committee, Martin Borchert, UNSW We collaborate widely across the Australasian sector Principles ● equity in scholarly communications, to access & publish research ● diverse ecosystem of open access approaches ● inteGrity and quality in research ● maximisation of the impact of research ● appropriate and respectful use of IndiGenous knowledGes ● retention of riGhts by authors or their institutions https://oaaustralasia.org/ A brief view from Australasia Open science initiatives triGGered by COVID-19 Discussions on a Australian national approach to open research 2021 in Australasian open science Lessons from the pandemic for the next crisis Australasian open science initiatives triggered by COVID-19 Some of the best pandemic science communication came from New Zealand! https://thespinoff.co.nz/media/12-05-2021/the-great-toby-morris-siouxsie-wiles-covid-19-omnibus/ Council of Australian University Librarians and Open Access Australasia: discussions on a national approach to open research Roundtable Canberra Cancelled! Discussions with national Webinars with international and national experts stakeholders Discussions with Chief Scientist and National Science and June December Technology Council 2020 2020 March November January 2020 First online 2020 Second 2021 - Roundtable -

New Zealand Media Ownership 2018
NEW ZEALAND MEDIA OWNERSHIP 2020 AUT research centre for Journalism, Media and Democracy (JMAD) Edited by Merja Myllylahti and Wayne Hope December 7, 2020 ABOUT THIS REPORT This report is part of JMAD’s ongoing series of reports on New Zealand media ownership. Since 2011, the AUT research centre for Journalism, Media and Democracy (JMAD) has published reports that document and analyse developments within New Zealand media. These incorporate media ownership, market structures and key events during each year. The reports are freely available and accessible to anyone via the JMAD research centre: https://www.aut.ac.nz/study/study-options/communication- studies/research/journalism,-media-and-democracy-research-centre 2020 report team To celebrate the JMAD research centre’s 10th anniversary, this 10th New Zealand media ownership report is co-written by AUT lecturers who are experts in their fields. The report is co-edited by the JMAD Co-Directors Dr Merja Myllylahti and Professor Wayne Hope. Contributors Dr Sarah Baker Dr Peter Hoar Professor Wayne Hope Dr Rufus McEwan Dr Atakohu Middleton Dr Merja Myllylahti Dr Greg Treadwell This report is covered by the Creative Commons Attribution License 4.0 International. When reproducing any part of this report – including tables and graphs – full attribution must be given to the report author(s). 1 10TH ANNIVERSARY OF JOURNALISM, MEDIA AND DEMOCRACY RESEARCH CENTRE The AUT research centre for Journalism, Media and Democracy (JMAD) was established in 2010 by (then) Associate Professors Wayne Hope and Martin Hirst to promote research into the media and communication industries and to increase knowledge about news and professional practices in journalism. -

Recombineering in Mycobacteria Using Mycobacteriophage Proteins
RECOMBINEERING IN MYCOBACTERIA USING MYCOBACTERIOPHAGE PROTEINS by Julia Catherine van Kessel B.S. Biology, Utica College of Syracuse University, 2003 Submitted to the Graduate Faculty of Arts and Sciences in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2008 UNIVERSITY OF PITTSBURGH SCHOOL OF ARTS AND SCIENCES This dissertation was presented by Julia Catherine van Kessel It was defended on July 24, 2008 and approved by Roger W. Hendrix, Ph.D., Biological Sciences, University of Pittsburgh William R. Jacobs, Jr., Ph.D., Albert Einstein College of Medicine Jeffrey G. Lawrence, Ph.D., Biological Sciences, University of Pittsburgh Valerie Oke, Ph.D., Biological Sciences, University of Pittsburgh Dissertation Advisor: Graham F. Hatfull, Ph.D., Biological Sciences, University of Pittsburgh ii Copyright © by Julia Catherine van Kessel 2008 iii RECOMBINEERING IN MYCOBACTERIA USING MYCOBACTERIOPHAGE PROTEINS Julia Catherine van Kessel, Ph.D. University of Pittsburgh, 2008 Genetic manipulations of Mycobacterium tuberculosis are complicated by its slow growth, inefficient DNA uptake, and relatively high levels of illegitimate recombination. Most methods for construction of gene replacement mutants are lengthy and complicated, and the lack of generalized transducing phages that infect M. tuberculosis prevents simple construction of isogenic mutant strains. Characterization and genomic analysis of mycobacteriophages has provided numerous molecular and genetic tools for the mycobacteria. Recently, genes encoding homologues of the Escherichia coli Rac prophage RecET proteins were revealed in the genome of mycobacteriophage Chec9c. RecE and RecT are functional analogues of the phage λ Red recombination proteins, Exo (exonuclease) and Beta (recombinase), respectively. These recombination enzymes act coordinately to promote high levels of recombination in vivo in E.