Antimicrobial Metabolites Against Methicillin-Resistant Staphylococcus Aureus from the Endophytic Fungus Neofusicoccum Australe
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 Webster Centre-QRW Programme National Symposium on Infectious Diseases: Key Opportunities and Emerging Therapies 7-8Th Septemb
Webster Centre-QRW Programme National Symposium on Infectious Diseases: key opportunities and emerging therapies 7-8th September, 2017 Rydges Hotel, Queenstown, New Zealand Thursday 7th September Time Details LoCation 8:45 – 8:55 am S1: IntroduCtion and opening remarks Andy MerCer – Webster Centre and One Health Aotearoa, University of Otago Session sponsored by One Health Aotearoa and Webster Centre, University of Otago 8:55 – 9.30 am Plenary talk: Professor Elizabeth Hartland Department of Microbiology and Immunology, University of Melbourne “Legionella intracellular replication” 9:30 – 10.00 am Nigel French, Massey University “Genomic anatomy of slow-burn epidemics” 10.00 – 10.30 am Morning Tea S2: Genomic approaches to Combat infeCtious disease Chair: James Ussher 10.30 – 11.00 am Deborah Williamson, Peter Doherty Institute for InfeCtion and Immunity “Applying genomics to outbreak investigations” 11.00 – 11.30am Professor David MurdoCh University of Otago, ChristchurCh Sponsored by New Zealand Food Safety Science & Research Centre “Infectious Diseases within an Increasingly Connected Ecosystem” 11.30 – 12.00pm Htin Aung University of Otago, Dunedin “Whole-genome sequencing for the management of drug-resistant tuberculosis in Myanmar” 12.00 – 12.30pm Mike Taylor, University of AuCkland “Bacterial community collapse: the microbiome in chronic sinus disease” 12.30 – 1.30pm Lunch 1 S3: Fighting BaCk: drug disCovery, AMR and vaccines Chair: Tim Stinear Plenary Talk: Professor John BlanChard 1.30 – 2.15pm Department of Biochemistry, Albert -

Pharmac Session: Antimicrobial Resistance - Global Threat Or Myth? (120Mins, Not Repeated) Antibiotic Resistance Mutations Or Creations? How We Squander a Miracle
Associate Professor Associate Professor David Holland Siouxsie Wiles Director Microbiologist Infection Services Head of the Bioluminescent Superbugs Lab Middlemore Hospital University of Auckland Professor Jack Mr Ben Harris Dr Peter Moodie Heinemann Honorary Lecturer General Practitioner University of Otago Wellington Genetics and Molecular Biology School of Biological Sciences University of Canterbury 14:00 - 16:00 WS #155: Pharmac Session: Antimicrobial Resistance - Global Threat or Myth? (120mins, not repeated) Antibiotic Resistance Mutations or Creations? How We Squander a Miracle Ben Harris, Medical Microbiology Scientist NZ Infection Prevention Control Consultancy [email protected] M: 0276273201 “We are not there to be phased by a brilliant international conference speaker we are there because we are gullible, ignorant & desperate” REFERENCE: Written comment from veteran GP regarding the didactic style that he finds most useful at GP CME “We are not there to be phased by a brilliant international conference speaker we are there because we are gullible, ignorant & desperate” Antibiotic Key Point On NZ average Prescribe well under 50% antibiotics you currently prescribe Because ➢ Reduce increasing MDRO endemicity ➢ Keep rapidly dwindling AB resource reserved for future serious infections ➢ Each AB use increases that patients medium to long term adverse chronic health outcomes Tips to Achieve This • Respiratory - follow BPAC guidelines • UTI – adults, clinical diagnosis, ban dipsticks • Cutaneous – lance abscess, no prophylactic -

Friday, July 10, 2020 Home-Delivered $1.90, Retail $2.20
TE NUPEPA O TE TAIRAWHITI FRIDAY, JULY 10, 2020 HOME-DELIVERED $1.90, RETAIL $2.20 LANDFILL BREACH STAR PAGES 3, 6-8, 10 ANOTHER WAKE-UP CALL OF GLEE COVID-19NEW 12-13, 20 PAGE 5 MISSING, • PBL Helen Clark heading Covid-19 response panel PRESUMED • Police to be posted at all managed isolation facilities DROWNED •PAGE Poor 3 response in US blamed on ‘anti-science bias’ • Covid-19 worldwide cases passes 12 million PAGE 12 SNOWDUST: Daytime maximum temperatures across Tairawhiti struggled to reach 11 degrees yesterday as the cold southerly brought a sprinkling of snow to the top of Mount Hikurangi — captured on camera by Sam Spencer. “We’re well and truly into the midst of winter now and yesterday sure would have felt like it,” said a MetService forecaster. “The dewpoint temperature (measure of moisture in air) was around zero degrees when the maximum air temperature was recorded. “The average daily maximum for Gisborne in July is around 15 degrees. “So it’s colder than average but it will need to drop a few more degrees to get into record books.” The district avoided the forecast frost overnight due to cloud cover, but MetService predicts 1 degree at Gisborne Airport tomorrow morning. by Matai O’Connor British High Commissioner to recovery,” she said. “Individuals New Zealand Laura Clarke, and organisations across TOITU Tairawhiti, a and Te Whanau o Waipareira Tairawhiti, including iwi, all collective of local iwi, have chief executive John Tamihere did a great job. organised a two-day summit to and Director-General of Health “We want to benchmark and reflect on the region’s response Dr Ashley Bloomfield. -
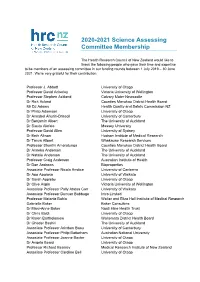
2020-2021 Science Assessing Committee Membership
2020-2021 Science Assessing Committee Membership The Health Research Council of New Zealand would like to thank the following people who gave their time and expertise to be members of an assessing committee in our funding rounds between 1 July 2019 – 30 June 2021. We’re very grateful for their contribution. Professor J. Abbott University of Otago Professor David Ackerley Victoria University of Wellington Professor Stephen Ackland Calvary Mater Newcastle Dr Rick Acland Counties Manukau District Health Board Mr DJ Adams Health Quality and Safety Commission NZ Dr Philip Adamson University of Otago Dr Annabel Ahuriri-Driscoll University of Canterbury Dr Benjamin Albert The University of Auckland Dr Siautu Alefaio Massey University Professor David Allen University of Sydney Dr Beth Allison Hudson Institute of Medical Research Dr Tanya Allport Whakauae Research Services Professor Shanthi Ameratunga Counties Manukau District Health Board Dr Anneka Anderson The University of Auckland Dr Natalie Anderson The University of Auckland Professor Craig Anderson Australian Institute of Health Dr Dan Andrews Bioproperties Associate Professor Nicola Anstice University of Canberra Dr Apo Aporosa University of Waikato Dr Sarah Appleby University of Otago Dr Clive Aspin Victoria University of Wellington Associate Professor Polly Atatoa Carr University of Waikato Associate Professor Duncan Babbage Intro Limited Professor Melanie Bahlo Walter and Eliza Hall Institute of Medical Research Gabrielle Baker Baker Consulting Dr Mary-Anne Baker Ngati Hine Health Trust -

Impact Innovation
#ASC14 BRISBANE February 2-5, 2014 INSIGHT IMPACT INNOVATION National Conference 2014 PROGRAM HANDBOOK www.ascconference.info 2 Organising committee Claire Harris Kali Madden Contents Jesse Shore Rod Lamberts Program committee Kali Madden Claire Harris Sponsors 3 Nancy Longnecker Jesse Shore Welcome messages 4 Social events committee Kali Madden Claire Harris 2014 and icons explained Andrew Stephenson 7 Kate Patterson Peter Wheeler Christine Ross Event highlights 8 SEQ ASC Branch Promotions and media committee General information 10 Claire Harris Kali Madden Sarah Lau Michelle Wheeler Social media policy 11 Kylie Sturgess Simon Chester James Hardy Sunday at a glance 13 Victoria Leitch Joan Leach John Harrison Monday at a glance 14 Andrew Wight Kate Hodge Students from The University of Queensland, Science Communication Tuesday at a glance 16 Peer reviewers Lindy Orthia Australian National University Wednesday at a glance 18 Will Grant Australian National University Vicky Martin Southern Cross University John O’Connor University of Newcastle Nancy Longnecker University of Western Australia Thursday at a glance 20 Emma Bartle University of Queensland Muza Gondwe University of Western Australia Will Rifkin University of Queensland Speaker and delegate index 21 Miriam Sullivan University of Western Australia Jennifer Manyweathers University of Western Australia Jenni Metcalfe Econnect Communication Venue and Brisbane maps 54 Jenny Donovan University of Southern Queensland Jean Fletcher University of Western Australia Volunteers Notes 56 Melanie McKenzie: evaluation Alex Jurkiewicz, website management Heidi Jones and others! Conference management Justin Holsinger and Melissa Batterbee from Eventcorp 3 HOSTED BY SPONSORS Silver WiFi Bronze Dinner Science Storytelling Event SUPPORTERS 4 PRESIDENT’S WELCOME As President of the Australian Science Communicators, I want to welcome you to my home city of Brisbane and to ASC2014. -
Lessons from the Pandemic: an Australasian Perspective
Lessons from the pandemic: an Australasian perspective 2nd Open Science Conference July 21-23, 2021 Dr Ginny Barbour Director, Open Access Australasia 28 universities across Australia & New Zealand, Creative Commons Australia & Tohatoha Aotearoa Commons Chair of Executive Committee, Martin Borchert, UNSW We collaborate widely across the Australasian sector Principles ● equity in scholarly communications, to access & publish research ● diverse ecosystem of open access approaches ● inteGrity and quality in research ● maximisation of the impact of research ● appropriate and respectful use of IndiGenous knowledGes ● retention of riGhts by authors or their institutions https://oaaustralasia.org/ A brief view from Australasia Open science initiatives triGGered by COVID-19 Discussions on a Australian national approach to open research 2021 in Australasian open science Lessons from the pandemic for the next crisis Australasian open science initiatives triggered by COVID-19 Some of the best pandemic science communication came from New Zealand! https://thespinoff.co.nz/media/12-05-2021/the-great-toby-morris-siouxsie-wiles-covid-19-omnibus/ Council of Australian University Librarians and Open Access Australasia: discussions on a national approach to open research Roundtable Canberra Cancelled! Discussions with national Webinars with international and national experts stakeholders Discussions with Chief Scientist and National Science and June December Technology Council 2020 2020 March November January 2020 First online 2020 Second 2021 - Roundtable -

New Zealand Media Ownership 2018
NEW ZEALAND MEDIA OWNERSHIP 2020 AUT research centre for Journalism, Media and Democracy (JMAD) Edited by Merja Myllylahti and Wayne Hope December 7, 2020 ABOUT THIS REPORT This report is part of JMAD’s ongoing series of reports on New Zealand media ownership. Since 2011, the AUT research centre for Journalism, Media and Democracy (JMAD) has published reports that document and analyse developments within New Zealand media. These incorporate media ownership, market structures and key events during each year. The reports are freely available and accessible to anyone via the JMAD research centre: https://www.aut.ac.nz/study/study-options/communication- studies/research/journalism,-media-and-democracy-research-centre 2020 report team To celebrate the JMAD research centre’s 10th anniversary, this 10th New Zealand media ownership report is co-written by AUT lecturers who are experts in their fields. The report is co-edited by the JMAD Co-Directors Dr Merja Myllylahti and Professor Wayne Hope. Contributors Dr Sarah Baker Dr Peter Hoar Professor Wayne Hope Dr Rufus McEwan Dr Atakohu Middleton Dr Merja Myllylahti Dr Greg Treadwell This report is covered by the Creative Commons Attribution License 4.0 International. When reproducing any part of this report – including tables and graphs – full attribution must be given to the report author(s). 1 10TH ANNIVERSARY OF JOURNALISM, MEDIA AND DEMOCRACY RESEARCH CENTRE The AUT research centre for Journalism, Media and Democracy (JMAD) was established in 2010 by (then) Associate Professors Wayne Hope and Martin Hirst to promote research into the media and communication industries and to increase knowledge about news and professional practices in journalism. -

AMR Resources What Is Antimicrobial Resistance? Antibiotic Resistance – World Health Organisation (2018). a Fact Sheet Summari
AMR Resources What is Antimicrobial Resistance? Antibiotic resistance – World Health Organisation (2018). A fact sheet summarising many of the key aspects of AMR. Contains links to useful information on other activities the WHO conducts and oversees as part of their wide-reaching work against AMR. Antibiotic resistance – Royal Society Te Apārangi (2017). A series of useful resources compiled by the Royal Society Te Apārangi outlining the state of AMR, with a specific focus on current evidence for the prevalence of resistance in New Zealand. Antibiotic Resistance – The End of Modern Medicine – Siouxsie Wiles (2017). An easily accessible and informative book on antibiotic resistance by a prominent New Zealand author and microbiologist. Antibiotic Resistance Questions and Answers – US Centre for Disease Control and Prevention (2017). A Q and A explaining some basic facts about AMR and help communicate ways to prevent the development and spread of resistance. Antibiotic resistance: a rundown of a global crisis – Aslam et al. Infection and Drug Rresistance (2018). A comprehensive overview of the current global situation regarding AMR covering the threat posed, what is needed and the promise of potential solutions. WHO: Handle Antibiotics with Care – World Health Organisation (2017). A short animated video giving a brief introduction to antibiotic resistance and containing important messages for the appropriate use of antibiotics. Future Impacts No to wait: securing the future from drug-resistant infections – Report to the Secretary General of the United Nations – Interagency Coordination Group on Antimicrobial Resistance (2019). A far-reaching report outlining the prospects of AMR and the global impacts it will have. It includes major recommendations for what actions is required internationally. -

INFORMED Emotional Tone and Checking Facts
tip What’s real? GETTING There are ways to explore whether online sheet information is legitimate including looking the #1 URL and the source, looking at the quality and INFORMED emotional tone and checking facts. Protective 1. TURN ANXIETY INTO ACTION! Actions List Get your facts from reputable sources: • Wash Your Hands • Ministry of Health COVID-19 Information • Centers for Disease Control • Avoid touching your nose, eyes and • Unite against COVID-19 mouth • World Health Organisation Coronavirus Information • Cough or Sneeze in your Elbow Making sense with: • Remember not to share food, • Nanogirl Explaining Coronavirus video (4min) (Source: You Tube) utensils, drinks or make up • Coronavirus Picture Book (Source: Mindheart) • Wipe desks, knobs, door handles • Coronavirus Comic for Kids (Source: NPR) and screens • Q & A with Dr Michelle Dickinson and Dr Juliet Gerrard (Source: PM Jacinda Ardern, Facebook Watch) • Stay at home when you are sick • Sneeze or cough into tissues Watch out for fear and fake news and think about: • Where have you been getting your information about Coronavirus? • Be Healthy – rest, sleep, eat well, • What have you noticed about the different styles of information? exercise • How would you determine reliable sources of information about • Stay away from sick people Coronavirus? • What have you noticed about the different styles of information? How did • Put used tissue in the bin you feel in response to each type of information? immediately • Read and get your Thinking Cap on with Critical thinking in an age of fake • Change your clothes when you get news (Source: newsroom) home from school • Ventilate your rooms or cars 2. -

Dr Michael O'sullivan
Healthcare Modelling for Pandemic Planning and Recovery Michael O’Sullivan Joint work with: Cameron Walker, Ilze Ziedins University of Auckland Summary of work from Te Pūnaha Matatini Dr Michael O’Sullivan Ko Maungakiekie te maunga Ko Waitemata te moana Dept of Engineering Science Ko waka moana te waka University of Auckland (UoA) Ko Te Atatu te marae Ko Airangi me Haina te iwi University of Auckland Ko O’Sullivan te hapu • BSc (Hons), MPhil (Disc) Ko Mike ahau Stanford University alumni • MS, PhD One Tree Hill is my mountain Waitemata is my ocean President, OR Society of NZ My waka (canoe) comes from over the sea Theme Leader, Precision Driven Health My community is Te Atatu Investigator, Te Punaha Matatini I am of Irish and Chinese descent (Complex Systems) My family is O’Sullivan Research/consulting in Operations Research and (Computational) I am Mike Analytics for Health, Social Investment, Cloud Computing, Infrastructure Planning, Finance University of Auckland/Te Pūnaha Matatini Researchers Associate Associate Dr Mike Professor Ilze Professor O’Sullivan Ziedins Cameron Walker Associate Professor Associate Professor Senior Lecturer in of Statistics, of Engineering Engineering Science, University of Auckland Science, University of University of Auckland • Ilze, Cameron and Mike are all AssociateAuckland Investigators with Auckland/Te Pūnaha Matatini • Involved in the response to Covid-19 – translating disease spread into hospital/ICU admissions • Have worked with Waitemata DHB and other DHBs previously • Surgery scheduling, CVICU -

Tuesday, April 6, 2021
TE NUPEPA O TE TAIRAWHITI TUESDAY, APRIL 6, 2021 HOME-DELIVERED $1.90, RETAIL $2.20 CHEERS TO THINKING COUNTDOWN TO BEERS ABOUT THE VACCINE PHASE 2 EASTER FESTIVAL NEXT STEP ROLL-OUT A HIT FEATURE INSIDE TODAY PAGE 4 PAGE 2 Kiri in fight of her life MP’s plea for regular smear testing after cancer diagnosis EAST COAST Member of The last smear test she had Parliament Kiri Allan faces was inspired by Smear Your the fight of her life after being Mea founder Talei Morrison just diagnosed with stage 3 cervical before she died from cervical cancer. cancer. Cabinet Minister Ms Allan “She rallied her whanau, shared the news today on her her friends, the kapa haka social media accounts, going community and ultimately New into depth about what she had Zealand to campaign for women, experienced so far and imploring and particularly Maori women, women to get regular smear to get their smear tests done tests. regularly,” said Ms Allan. Prime Minister Jacinda “I’m one of those gals who Ardern announced today that hates anything to do with ‘down Ms Allan was there’ and have taking medical taken a ‘see leave from work I’m one of those gals no evil, hear and acting ‘ no evil’-type ministers would who hates anything to approach to THERE FOR MUM: East Coast MP Kiri Allan has stage 3 cervical cancer and is taking medical leave for be appointed on do with ‘down there’ and that part of my treatment. The Cabinet Minister, pictured with daughter Hiwa-i-te-rangi Rangitaia Ramarihi Allan-Coates, her behalf. -

Note: This Paper Has Not Yet Undergone Formal Peer Review
Note: This paper has not yet undergone formal peer review Evaluating the infodemic: assessing the prevalence and nature of COVID- 19 unreliable and untrustworthy information in Aotearoa New Zealand’s social media, January-August 2020 6 September 2020 Max Soar1,2, Victoria Louise Smith1,3, M.R.X. Dentith4, Daniel Barnett5,6, Kate Hannah1,2,7, Giulio Valentino Dalla Riva8, Andrew Sporle5,6 1. Te Pūnaha Matatini: Centre of Research Excellence for Complex Systems and Networks, New Zealand 2. Centre for Science in Society, Te Herenga Waka – Victoria University of Wellington 3. Faculty of Science, University of Auckland 4. University of Waikato 5. Department of Statistics, University of Auckland 6. iNZight Analytics 7. Department of Physics, University of Auckland 8. School of Mathematics and Statistics, University of Canterbury Abstract The arrival of the COVID-19 pandemic in Aotearoa New Zealand saw New Zealanders presented with the accompanying infodemic. Aotearoa New Zealand’s experience, which is characterised by mis- and dis-information, as well as the emergence of a number of conspiracy theories, is linked to international patterns within the COVID-19 infodemic overall, but also displays significant situated and differential themes and impacts. We evaluate the prevalence of the COVID-19 infodemic in social and mainstream media February-August 2020, and analyse the narrative intent and social or political discourses of the content collated. In evaluating the nature of COVID-19 narratives over this time period, we find that there are significant changes in the types of discourses these narratives engage with, with an increasing prevalence of conspiracy narratives noted since the re-emergence of community transmission in August.