Added Value of Physos Gmine?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Physical Study by Surface Characteriza4ons of Sarin Sensor on the Basis of Chem
Physical Study by Surface Characterizaons of Sarin Sensor on the Basis of Chemically Func4onalized Silicon Nanoribbon Field Effect Transistor K. Smaali1,§, D. Guérin1, V. Passi1, L. Ordronneau2, A. Carella2, T. Mélin1, E. Dubois1, D. Vuillaume1, J.P. Simonato2 and S. Lenfant1,* 1 IEMN, CNRS, Avenue Poincaré, Villeneuve d'Ascq, F-59652 cedex, France. 2. CEA, LITEN/DTNM/SEN/LSIN, Univ. Grenoble Alpes, MINATEC Campus, F-38054 Grenoble, France. ABSTRACT : Surface characteriZa[ons of an organophosphorus (OP) gas detector based on chemically func[onaliZed silicon nanoribbon field-effect transistor (SiNR-FET) were performed by Kelvin Probe Force Microscopy (KPFM) and ToF-SIMS, and correlated with changes in the current-voltage characteris[cs of the devices. KPFM measurements on FETs allow (i) to inves[gate the contact poten[al difference (CPD) distribu[on of the polariZed device as func[on of the gate voltage and the exposure to OP traces and; (ii) to analyZe the CPD hysteresis associated to the presence of mobile ions on the surface. The CPD measured by KPFM on the silicon nanoribbon was corrected due to side capacitance effects in order to determine the real quan[ta[ve surface poten[al. Comparison with macroscopic Kelvin probe (KP) experiments on larger surfaces was carried out. These two approaches were quan[ta[vely consistent. An important increase of the CPD values (between + 399 mV and + 302 mV) was observed aeer the OP sensor graeing, corresponding to a decrease of the work func[on, and a weaker varia[on aeer exposure to OP (between - 14 mV and - 61 mV) was measured. -

Nerve Agent - Lntellipedia Page 1 Of9 Doc ID : 6637155 (U) Nerve Agent
This document is made available through the declassification efforts and research of John Greenewald, Jr., creator of: The Black Vault The Black Vault is the largest online Freedom of Information Act (FOIA) document clearinghouse in the world. The research efforts here are responsible for the declassification of MILLIONS of pages released by the U.S. Government & Military. Discover the Truth at: http://www.theblackvault.com Nerve Agent - lntellipedia Page 1 of9 Doc ID : 6637155 (U) Nerve Agent UNCLASSIFIED From lntellipedia Nerve Agents (also known as nerve gases, though these chemicals are liquid at room temperature) are a class of phosphorus-containing organic chemicals (organophosphates) that disrupt the mechanism by which nerves transfer messages to organs. The disruption is caused by blocking acetylcholinesterase, an enzyme that normally relaxes the activity of acetylcholine, a neurotransmitter. ...--------- --- -·---- - --- -·-- --- --- Contents • 1 Overview • 2 Biological Effects • 2.1 Mechanism of Action • 2.2 Antidotes • 3 Classes • 3.1 G-Series • 3.2 V-Series • 3.3 Novichok Agents • 3.4 Insecticides • 4 History • 4.1 The Discovery ofNerve Agents • 4.2 The Nazi Mass Production ofTabun • 4.3 Nerve Agents in Nazi Germany • 4.4 The Secret Gets Out • 4.5 Since World War II • 4.6 Ocean Disposal of Chemical Weapons • 5 Popular Culture • 6 References and External Links --------------- ----·-- - Overview As chemical weapons, they are classified as weapons of mass destruction by the United Nations according to UN Resolution 687, and their production and stockpiling was outlawed by the Chemical Weapons Convention of 1993; the Chemical Weapons Convention officially took effect on April 291997. Poisoning by a nerve agent leads to contraction of pupils, profuse salivation, convulsions, involuntary urination and defecation, and eventual death by asphyxiation as control is lost over respiratory muscles. -
Warning: the Following Lecture Contains Graphic Images
What the новичок (Novichok)? Why Chemical Warfare Agents Are More Relevant Than Ever Matt Sztajnkrycer, MD PHD Professor of Emergency Medicine, Mayo Clinic Medical Toxicologist, Minnesota Poison Control System Medical Director, RFD Chemical Assessment Team @NoobieMatt #ITLS2018 Disclosures In accordance with the Accreditation Council for Continuing Medical Education (ACCME) Standards, the American Nurses Credentialing Center’s Commission (ANCC) and the Commission on Accreditation for Pre-Hospital Continuing Education (CAPCE), states presenters must disclose the existence of significant financial interests in or relationships with manufacturers or commercial products that may have a direct interest in the subject matter of the presentation, and relationships with the commercial supporter of this CME activity. The presenter does not consider that it will influence their presentation. Dr. Sztajnkrycer does not have a significant financial relationship to report. Dr. Sztajnkrycer is on the Editorial Board of International Trauma Life Support. Specific CW Agents Classes of Chemical Agents: The Big 5 The “A” List Pulmonary Agents Phosgene Oxime, Chlorine Vesicants Mustard, Phosgene Blood Agents CN Nerve Agents G, V, Novel, T Incapacitating Agents Thinking Outside the Box - An Abbreviated List Ammonia Fluorine Chlorine Acrylonitrile Hydrogen Sulfide Phosphine Methyl Isocyanate Dibotane Hydrogen Selenide Allyl Alcohol Sulfur Dioxide TDI Acrolein Nitric Acid Arsine Hydrazine Compound 1080/1081 Nitrogen Dioxide Tetramine (TETS) Ethylene Oxide Chlorine Leaks Phosphine Chlorine Common Toxic Industrial Chemical (“TIC”). Why use it in war/terror? Chlorine Density of 3.21 g/L. Heavier than air (1.28 g/L) sinks. Concentrates in low-lying areas. Like basements and underground bunkers. Reacts with water: Hypochlorous acid (HClO) Hydrochloric acid (HCl). -

Chemical Warfare Nerve Agents the V Series Nerve Agents Are Highly Toxic Chemical Warfare Agents
CHEMICAL WARFARE NERVE AGENTS THE V SERIES NERVE AGENTS ARE HIGHLY TOXIC CHEMICAL WARFARE AGENTS. THE ‘V’ STANDS FOR ‘VENOMOUS’. THEY WERE DISCOVERED IN THE PART TWO: THE V SERIES UK IN THE 1950s, AND LATER VX WAS DEVELOPED FOR MILITARY USE BY THE UNITED STATES, THOUGH IT HAS NEVER BEEN USED IN WARFARE. O O O O N P N P O S N P O S N P O S O S O VX VE VG VM (O-Ethyl-S-[2(diisopropylamino)ethyl] methylphosphonothioate) O-Ethyl-S-[2-(diethylamino)ethyl] ethylphosphonothioate O,O-Diethyl-S-[2-(diethylamino)ethyl] phosphorothioate O-Ethyl-S-[2-(diethylamino)ethyl] methylphosphonothioate (the compound known as ‘Russian VX’ is an isomer of this compound) SMELL & APPEARANCE DISCOVERY USAGE & FATALITIES LETHALITY FIGURES FOR VX Pure VX is a colourless liquid, but more As the V series agents exist primarily as low commonly it is an amber-coloured, – volatility liquids, they are designed for use median lethal concentration median lethal dose VX oily, odourless liquid. 1952 1955 as area-denial agents. UNITED KINGDOM The only recorded human fatality as a result 15 10 The other V series nerve agents are milligram-minutes per milligrams per person The V series nerve agents were discovered during of VX is in Japan in 1994, when a sect used it cubic metre (skin exposure) thought to be odourless, colourless work to synthesise pesticides and insecticides. to assassinate a former member. It may have VE liquids at room temperature (when also been used in Iraq by Saddam Hussein, Due to the scarcity of research on the V series VG was originally sold as a insecticide, under pure). -

Efficacy of Trimedoxime in Mice Poisoned with Dichlorvos, Heptenophos Or Monocrotophos
CORE Metadata, citation and similar papers at core.ac.uk Provided by FarFar - Repository of the Faculty of Pharmacy, University of Belgrade C Basic & Clinical Pharmacology & Toxicology 2005, 96, 111–117. Printed in Denmark . All rights reserved Copyright C ISSN 1742-7835 Efficacy of Trimedoxime in Mice Poisoned with Dichlorvos, Heptenophos or Monocrotophos Biljana Antonijevic´1, Dubravko Bokonjic´2, Milosˇ P. Stojiljkovic´2, Vesna Kilibarda2, Zoran A. Milovanovic´2, Mirjana Nedeljkovic´1 and Matej Maksimovic´1 1Institute of Toxicological Chemistry, School of Pharmacy, University of Belgrade, Vojvode Stepe 450, and 2National Poison Control Centre, Military Medical Academy, Crnotravska 17; 11000 Belgrade, Serbia and Montenegro (Received June 18, 2004; Accepted September 3, 2004) Abstract: The aim of the study was to examine antidotal potency of trimedoxime in mice poisoned with three direct dimethoxy-substituted organophosphorus inhibitors. In order to assess the protective efficacy of trimedoxime against dichlorvos, heptenophos or monocrotophos, median effective doses and efficacy half-times were calculated. Trimedoxime (24 mg/kg intravenously) was injected 5 min. before 1.3 LD50 intravenously of poisons. Activities of brain, diaphragmal and erythrocyte acetylcholinesterase, as well as of plasma carboxylesterases were determined at different time intervals (10, 40 and 60 min.) after administration of the antidotes. Protective effect of trimedoxime decreased according to the following order: monocrotophos Ͼ heptenophos Ͼ dichlorvos. Administration of the oxime produced a significant reacti- vation of central and peripheral acetylcholinesterase inhibited with dichlorvos and heptenophos, with the exception of erythrocyte acetylcholinesterase inhibited by heptenophos. Surprisingly, trimedoxime did not induce reactivation of mon- ocrotophos-inhibited acetylcholinesterase in any of the tissues tested. -

Acetylcholinesterase: the “Hub” for Neurodegenerative Diseases And
Review biomolecules Acetylcholinesterase: The “Hub” for NeurodegenerativeReview Diseases and Chemical Weapons Acetylcholinesterase: The “Hub” for Convention Neurodegenerative Diseases and Chemical WeaponsSamir F. de A. Cavalcante Convention 1,2,3,*, Alessandro B. C. Simas 2,*, Marcos C. Barcellos 1, Victor G. M. de Oliveira 1, Roberto B. Sousa 1, Paulo A. de M. Cabral 1 and Kamil Kuča 3,*and Tanos C. C. França 3,4,* Samir F. de A. Cavalcante 1,2,3,* , Alessandro B. C. Simas 2,*, Marcos C. Barcellos 1, Victor1 Institute G. M. ofde Chemical, Oliveira Biological,1, Roberto Radiological B. Sousa and1, Paulo Nuclear A. Defense de M. Cabral (IDQBRN),1, Kamil Brazilian Kuˇca Army3,* and TanosTechnological C. C. França Center3,4,* (CTEx), Avenida das Américas 28705, Rio de Janeiro 23020-470, Brazil; [email protected] (M.C.B.); [email protected] (V.G.M.d.O.); [email protected] 1 Institute of Chemical, Biological, Radiological and Nuclear Defense (IDQBRN), Brazilian Army (R.B.S.); [email protected] (P.A.d.M.C.) Technological Center (CTEx), Avenida das Américas 28705, Rio de Janeiro 23020-470, Brazil; 2 [email protected] Mors Institute of Research (M.C.B.); on Natural [email protected] Products (IPPN), Federal (V.G.M.d.O.); University of Rio de Janeiro (UFRJ), CCS,[email protected] Bloco H, Rio de Janeiro (R.B.S.); 21941-902, [email protected] Brazil (P.A.d.M.C.) 32 DepartmentWalter Mors of Institute Chemistry, of Research Faculty of on Science, Natural Un Productsiversity (IPPN), -
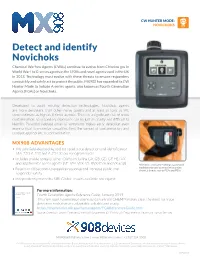
Detect and Identify Novichoks
CW HUNTER MODE: NOVICHOKS Detect and identify Novichoks Chemical Warfare Agents (CWAs) continue to evolve from Chlorine gas in World War I to G-series agents in the 1930s and novel agents used in the UK in 2018. Technology must evolve with these threats to ensure responders can quickly and safely act to protect the public. MX908 has expanded its CW Hunter Mode to include A-series agents, also known as Fourth Generation Agents (FGAs) or Novichoks. Developed to avoid existing detection technologies, Novichok agents are more persistent than other nerve agents and at least as toxic as VX; some estimate as high as 8 times as toxic. There is a significant risk of cross contamination, so secondary exposures can be just as deadly and difficult to identify. Potential delayed onset of symptoms makes early detection even more critical to minimize casualties, limit the spread of contamination, and conduct appropriate decontamination. MX908 ADVANTAGES • The only field-deployable tool for rapid trace detection and identification of A-230, A-232 and A-234 at low nanogram levels • Includes a wide range of other CWAs including GA, GB, GD, GF, HD, VX and additional V-series agents (VE, VM, VLX, VS, RVX/CVX and VX acid) MX908 is continually evolving to go beyond traditional threats by adressing emerging • Results in 60 seconds to expedite response and increase public and chemical threats such as FGAs and PBAs. responder safety • Independently tested by MRI Global; results available on request For more information: FOURTH GENERATION AGENTS: REFERENCE GUIDE Fourth Generation Agents: Reference Guide, January 2019 January 2019 This new fourth generation agent guidance from CHEMM makes clear the need for trace detection tools that are adaptable, reliable and ready. -

Nerve Agents (Ga, Gb, Gd, Vx) Tabun (Ga) Cas # 77-81-6 Sarin (Gb) Cas # 107-44-8 Soman (Gd) Cas # 96-64-0 Vx Cas # 50782-69-9
NERVE AGENTS (GA, GB, GD, VX) TABUN (GA) CAS # 77-81-6 SARIN (GB) CAS # 107-44-8 SOMAN (GD) CAS # 96-64-0 VX CAS # 50782-69-9 Division of Toxicology ToxFAQsTM April 2002 This fact sheet answers the most frequently asked health questions (FAQs) about nerve agents. For more information, call the ATSDR Information Center at 1-888-422-8737. This fact sheet is one in a series of summaries about hazardous substances and their health effects. It is important you understand this information because this substance may harm you. The effects of exposure to any hazardous substance depend on the dose, the duration, how you are exposed, personal traits and habits, and whether other chemicals are present. HIGHLIGHTS: Exposure to nerve agents can occur due to accidental release from a military storage facility. Nerve agents are highly toxic regardless of the route of exposure. Exposure to nerve agents can cause tightness of the chest, excessive salivation, abdominal cramps, diarrhea, blurred vision, tremors, and death. Nerve agents (GA, GB, GD, VX) have been identified at 5 of the 1,585 National Priorities List sites identified by the Environmental Protection Agency (EPA). What are nerve agents GA, GB, GD, and VX? ‘ GA, GB, GD, and VX will be broken down in water quickly, but small amounts may evaporate. Nerve agents GA(tabun), GB (sarin), GD(soman), and VX are ‘ GA, GB, GD, and VX will be broken down in moist soil manufactured compounds. The G-type agents are clear, quickly. Small amounts may evaporate into air or travel colorless, tasteless liquids miscible in water and most below the soil surface and contaminate groundwater. -

Medical Aspects of Chemical and Biological Warfare, Index
Index INDEX A Aircrew uniform, integrated battlefield (AUIB), 373 Air delivery Aberdeen Proving Ground, Maryland, 398, 409–410 history, 28, 31, 34–35, 49–50 See also Edgewood Arsenal, Maryland See also Aerosol; Inhalational injury; specific agent ABG Airplane smoke tanks, 31 See Arterial blood gases (ABG) AIT Abortion See Aeromedical Isolation Team (AIT) septic, in brucellosis, 516 Alarms, 377–383 Abrin, 610, 632 biological agent, 431 Abrus precatorius, 610, 632 history, 23, 53, 60–62, 66–67 AC LOPAIR, E33 Area Scanning, 53 See Hydrogen cyanide (AC) M8A1 Automatic Chemical Agent, 380–381 Acetaminophen, 627 M21 Remote Sensing Chemical Agent (RSCAAL), 381 Acetylcholine (ACh), 132–134, 136, 159, 647 Portable Automatic Chemical Agent, 60–62 Acetylcholinesterase (AChE), 131–132, 134, 182–184 See also Detection Acetylene tetrachloride, 34 Alastrim, 543 Acid hydrolysis, 355 Alexander, Stewart, 103 Action potential, 133 Algal toxins, 457, 609, 617 Activated charcoal, 217, 362–363, 366, 370, 373, 670 Alimentary toxic aleukia (ATA), 659, 667 Adamsite Alkaline hydrolysis, 355 See DM (diphenylaminearsine) Allergic contact sensitivity, 238–239, 249, 314, 316–317 Additives, 122 a -Naphthylthiourea (ANTU), 638 Adenine arabinoside (Ara-A), 553 Alphaviruses, 562 Adenosine triphosphate (ATP), 275, 383, 431 antigenic classification, 564–565 S-Adenosylhomocysteine hydrolase inhibitors, 552 structure and replication, 569–570 Adenoviridae, 575, 683 See also Viral encephalitides; specific virus Adrenaline, 132 Alphavirus virion, 569 Adrenergic nervous system, -

Pretreatment and Prophylaxis Against Nerve Agent Poisoning: Are Undesirable Behavioral Side Effects Unavoidable?
1 Pretreatment and prophylaxis against nerve agent poisoning: Are undesirable behavioral side effects unavoidable? Trond Myhrer, Pål Aas Norwegian Defence Research Establishment (FFI), Protection and Societal Security Division, Kjeller, Norway Running title: Pretreatment and side effects Correspondence: Pål Aas Norwegian Defence Research Establishment (FFI) Protection and Societal Security Division P O Box 25 NO-2027 Kjeller, Norway Phone: +47 63 80 78 43 Fax: +47 63 80 75 09 E-mail: [email protected] 2 Abstract The threat of chemical warfare agents like nerve agents requires life saving measures of medical pretreatment combined with treatment after exposure. Pretreatment (pyridostigmine) may cause some side effects in a small number of individuals. A comprehensive research on animals has been performed to clarify effects on behavior. The results from these studies are far from unambiguous, since pyridostigmine may produce adverse effects on behavior in animals in relatively high doses, but not in a consistent way. Other animal studies have examined the potential of drugs like physostigmine, galantamine, benactyzine, trihexyphenidyl, and procyclidine, but they all produce marked behavioral impairment at doses sufficient to contribute to protection against a convulsant dose of soman. Attempts have also been made to develop a combination of drugs capable of assuring full protection (prophylaxis) against nerve agents. However, common to all combinations is that they at anticonvulsant doses cause behavioral deficits. Therefore, the use of limited pretreatment doses may be performed without marked side effects followed by post-exposure therapy with a combination of drugs. Keywords: Nerve agents; Pharmacological protection; Enzymatic protection; Behavioral side effects 3 1. Introduction Organophosphates called nerve agents are considered to be the most toxic among all chemical weapons. -

On the Universality of Oxime Hlö-7 – Antidote for Case of the Nerve Agent Poisoning
Mil. Med. Sci. Lett. (Voj. Zdrav. Listy) 2011, vol. 80, p. 80-84 ISSN 0372-7025 DOI: 10.31482/mmsl.2011.012 ORIGINAL ARTICLE ON THE UNIVERSALITY OF OXIME HLö-7 – ANTIDOTE FOR CASE OF THE NERVE AGENT POISONING Kamil Kuca 1,2 , Kamil Musilek 2,3 , Jana Karasova 2,4 , Daniel Jun 2, Ondrej Soukup 1,2 , Miroslav Pohanka 1,2 , Kallol Kumar Ghosh 5, Martina Hrabinova 1 1 Center of Advanced Studies, Faculty of Military Health Sciences, University of Defence, Hradec Kralove, Czech Republic 2 University Hospital, Hradec Kralove, Czech Republic 3 University of Hradec Kralove, Faculty of Science, Department of Chemistry, Hradec Kralove, Czech Republic 4 Department of Public Health, Faculty of Military Health Sciences, University of Defence, Hradec Kralove, Czech Republic 5 School of Studies in Chemistry, Pt. Ravishankar Shukla University, Raipur (C.G.), India Received 12 th April 2011. Revised 29 th May 2011. Published 10 th June 2011. Summary Searching for the universal oxime, which could be able to reactivate acetylcholinesterase inhibited by various nerve agents is still topic of high interest. In this contribution, oxime HLö-7, that was thoroughly discussed in the last decade, is evaluated . Its universality was tested in vitro using the rat brain homogenate as a source of the cholinesterases. The main members of the nerve agent family (tabun, sarin, soman, cyclosarin and VX) were used for this purpose. As shown, oxime HLö-7 was able to reactivate cholinesterases inhibited by all tested nerve agents with the exception of tabun. Hence, it could not be designated as the broad-spectrum reactivator. -

In Vitro Evaluation of Neutral Aryloximes As Reactivators for Electrophorus Eel Acetylcholinesterase Inhibited by Paraoxon
biomolecules Article In Vitro Evaluation of Neutral Aryloximes as Reactivators for Electrophorus eel Acetylcholinesterase Inhibited by Paraoxon Daniel A. S. Kitagawa 1,2 , Samir F. de A. Cavalcante 2,3,4,5,* , Reuel L. de Paula 2,6 , Rafael B. Rodrigues 2, Leandro B. Bernardo 2, Munique C. J. da Silva 2 , Thiago N. da Silva 4, Wellington V. dos Santos 7,8, José M. Granjeiro 6, Joyce S. F. D. de Almeida 1 , Marcos C. Barcellos 2, Ana Beatriz de A. Correa 2 , Tanos C. C. França 1,5 , Kamil Kuˇca 5,* and Alessandro B. C. Simas 3,* 1 Laboratory of Molecular Modelling Applied to Chemical and Biological Defense (LMACBD), Military Institute of Engineering (IME), Praça General Tibúrcio 80, Rio de Janeiro 22290-270, Brazil 2 Brazilian Army Institute of Chemical, Biological, Radiological and Nuclear Defense (IDQBRN), Brazilian Army Technological Center (CTEx), Avenida das Américas 28705, Rio de Janeiro 23020-470, Brazil 3 Walter Mors Institute of Research on Natural Products (IPPN), Federal University of Rio de Janeiro (UFRJ), CCS, Bloco H, Rio de Janeiro 21941-902, Brazil 4 Castelo Branco University (UCB), School of Pharmacy, Avenida Santa Cruz 1631, Rio de Janeiro 21710-255, Brazil 5 Department of Chemistry, Faculty of Science, University of Hradec Králové, Rokitanskeho 62, 50003 Hradec Králové, Czech Republic 6 National Institute of Metrology, Standardization and Industrial Quality (INMETRO), Avenida Nossa Senhora das Graças 50, Duque de Caxias 25250-020, Brazil 7 Emergency and Rescue Department (DSE), Rio de Janeiro State Fire Department (CBMERJ), Praça São Salvador 4, Rio de Janeiro 22231-170, Brazil 8 School of Biomedicine, University Universus Veritas (UNIVERITAS), Rua Marquês de Abrantes 55, Rio de Janeiro 22230-060, Brazil * Correspondence: [email protected] (S.F.d.A.C.); [email protected] (K.K.); [email protected] (A.B.C.S.) Received: 9 September 2019; Accepted: 4 October 2019; Published: 8 October 2019 Abstract: Casualties caused by organophosphorus pesticides are a burden for health systems in developing and poor countries.