Histamine Intolerance: Why Freshness Matters
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Headache Is One of the Most Common Complaints Voiced in a Doctor's
Headache is one of the most common complaints voiced in a doctor’s examination room. Many of these headaches are "benign" in the sense that they are brought on by stress or anxiety, the amount of discomfort is mild to moderate, and relief is achieved withi n a few hours. A second type of headache occurs secondary to a medical illnesses, usually a minor condition such as the flu. Only in rare cases are these headaches a sign of serious conditions such as cerebral aneurysms or strokes. A third type of headache , affecting 10 - 20% of the population, is a migraine (1). Migraines consist of periodic attacks of hemicranial pain, vomiting, photophobia, phonophobia, tiredness, irritability, and impaired concentration. In the case of a classical migraine, the headache itself is preceded by an "aura" consisting of visual problems, generally blind spots or hallucinations. A common migraine contains no premonitory aura (2). Several hypothesis have been proposed to account for the various features of a migraine, yet no cle ar mechanism exists to explain why or how a migraine headache occurs. Certain foods, such as chocolate, wine, and cheese, have been suspected of initiating migraines. It is the purpose of this paper to evaluate the evidence for dietary triggers of migraine s, suggest a mechanism by which specific molecules in food could induce a migraine, and make recommendations regarding dietary treatment for migraine sufferers. Research on the Role of Food in Migraine Headaches Studies implicating food in the pathogene sis of migraines date back to the 1920’s when researchers began to examine and manipulate the diets of individuals suffering from migraines. -
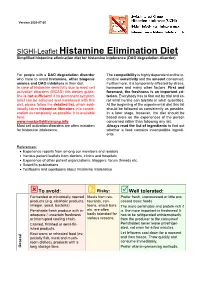
SIGHI-Leaflet Histamine Elimination Diet Simplified Histamine Elimination Diet for Histamine Intolerance (DAO Degradation Disorder)
Version 2020-07-20 SIGHI-Leaflet Histamine Elimination Diet Simplified histamine elimination diet for histamine intolerance (DAO degradation disorder) For people with a DAO degradation disorder The compatibility is highly dependent on the in- who have to avoid histamine, other biogenic dividual sensitivity and the amount consumed. amines and DAO inhibitors in their diet. Furthermore, it is temporarily affected by stress, In case of histamine sensitivity due to mast cell hormones and many other factors. First and activation disorders (MCAD) this dietary guide- foremost, the freshness is an important cri- line is not sufficient! If no permanent symptom terion. Everybody has to find out by trial and er- relief can be achieved and maintained with this ror what he/she can tolerate in what quantities. diet, please follow the detailed list, which addi- At the beginning of the experimental diet this list tionally takes histamine liberators into consid- should be followed as consistently as possible. eration as completely as possible. It is available In a later stage, however, the diet should be here: based more on the experiences of the person www.mastzellaktivierung.info concerned rather than following any list. Mast cell activation disorders are often mistaken Always read the list of ingredients to find out for histamine intolerance. whether a food contains incompatible ingredi- ents. References: • Experience reports from among our members and readers • Various patient leaflets from doctors, clinics and hospitals • Experience of other patient organizations, bloggers, forum threads etc. • Scientific publications • Textbooks and cookbooks about histamine intolerance To avoid: ? Risky: Well tolerated: Fermented or microbially ripened Meals from res- Prefer fresh, unprocessed or little pro- products (e.g. -

THE USE of MIRTAZAPINE AS a HYPNOTIC O Uso Da Mirtazapina Como Hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa
ARTIGO ESPECIAL THE USE OF MIRTAZAPINE AS A HYPNOTIC O uso da mirtazapina como hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa Prescription of approved hypnotics for insomnia decreased by more than 50%, whereas of antidepressive agents outstripped that of hypnotics. However, there is little data on their efficacy to treat insomnia, and many of these medications may be associated with known side effects. Antidepressants are associated with various effects on sleep patterns, depending on the intrinsic pharmacological properties of the active agent, such as degree of inhibition of serotonin or noradrenaline reuptake, effects on 5-HT1A and 5-HT2 receptors, action(s) at alpha-adrenoceptors, and/or histamine H1 sites. Mirtazapine is a noradrenergic and specific serotonergic antidepressive agent that acts by antagonizing alpha-2 adrenergic receptors and blocking 5-HT2 and 5-HT3 receptors. It has high affinity for histamine H1 receptors, low affinity for dopaminergic receptors, and lacks anticholinergic activity. In spite of these potential beneficial effects of mirtazapine on sleep, no placebo-controlled randomized clinical trials of ABSTRACT mirtazapine in primary insomniacs have been conducted. Mirtazapine was associated with improvements in sleep on normal sleepers and depressed patients. The most common side effects of mirtazapine, i.e. dry mouth, drowsiness, increased appetite and increased body weight, were mostly mild and transient. Considering its use in elderly people, this paper provides a revision about studies regarding mirtazapine for sleep disorders. KEYWORDS: sleep; antidepressive agents; sleep disorders; treatment� A prescrição de hipnóticos aprovados para insônia diminuiu em mais de 50%, enquanto de antidepressivos ultrapassou a dos primeiros. -

Histamine and Gut Mucosal Immune Regulation S
Allergy REVIEW ARTICLE Histamine and gut mucosal immune regulation S. Smolinska1,2, M. Jutel1,2, R. Crameri3 & L. O’Mahony3 1Department of Clinical Immunology, Wroclaw Medical University, Wroclaw; 2‘ALL-MED’ Medical Research Institute, Wroclaw, Poland; 3Swiss Institute of Allergy and Asthma Research, University of Zurich, Davos, Switzerland To cite this article: Smolinska S, Jutel M, Crameri R, O’Mahony L. Histamine and gut mucosal immune regulation. Allergy 2013; DOI: 10.1111/all.12330. Keywords Abstract allergy; histamine; inflammation; microbial Histamine is a biogenic amine with extensive effects on many cell types, mediated metabolites; mucosal immunology. by the activation of its four receptors (H1R–H4R). Distinct effects are dependent Correspondence on receptor subtypes and their differential expression. Within the gastrointestinal Dr. Liam O’Mahony, SIAF, Obere Strasse tract, histamine is present at relatively high concentrations, particularly during 22, 7270 Davos Platz, Switzerland. inflammatory responses. In this review, we discuss the immunoregulatory influ- Tel.: +41-81-4100853 ence of histamine on a number of gastrointestinal disorders, including food Fax: +41-81-4100840 allergy, scombroid food poisoning, histamine intolerance, irritable bowel syn- E-mail: [email protected] drome, and inflammatory bowel disease. It is clear that the effects of histamine on mucosal immune homeostasis are dependent on expression and activity of the Accepted for publication 21 October 2013 four currently known histamine receptors; however, the relative protective or pathogenic effects of histamine on inflammatory processes within the gut are still DOI:10.1111/all.12330 poorly defined and require further investigation. Edited by: Hans-Uwe Simon Histamine [2-(4-imidazolyl)-ethylamine] is a short-acting studies demonstrate the influence of histamine on wound endogenous amine, which is widely distributed throughout healing, circulatory disease, immunology, oncology, and the body (1, 2). -

Food Allergy and Intolerance: a Narrative Review on Nutritional Concerns
nutrients Review Food Allergy and Intolerance: A Narrative Review on Nutritional Concerns Domenico Gargano 1,†, Ramapraba Appanna 2,†, Antonella Santonicola 2 , Fabio De Bartolomeis 1, Cristiana Stellato 2, Antonella Cianferoni 3, Vincenzo Casolaro 2 and Paola Iovino 2,* 1 Allergy and Clinical Immunology Unit, San Giuseppe Moscati Hospital, 83100 Avellino, Italy; [email protected] (D.G.); [email protected] (F.D.B.) 2 Department of Medicine, Surgery and Dentistry “Scuola Medica Salernitana”, University of Salerno, 84081 Baronissi, Italy; [email protected] (R.A.); [email protected] (A.S.); [email protected] (C.S.); [email protected] (V.C.) 3 Division of Allergy and Immunology, The Children’s Hospital of Philadelphia, Perelman School of Medicine at University of Pennsylvania, Philadelphia, PA 19104, USA; [email protected] * Correspondence: [email protected]; Tel.: +39-335-7822672 † These authors contributed equally to this work. Abstract: Adverse food reactions include immune-mediated food allergies and non-immune-mediated intolerances. However, this distinction and the involvement of different pathogenetic mechanisms are often confused. Furthermore, there is a discrepancy between the perceived vs. actual prevalence of immune-mediated food allergies and non-immune reactions to food that are extremely common. The risk of an inappropriate approach to their correct identification can lead to inappropriate diets with severe nutritional deficiencies. This narrative review provides an outline of the pathophysiologic and clinical features of immune and non-immune adverse reactions to food—along with general Citation: Gargano, D.; Appanna, R.; diagnostic and therapeutic strategies. Special emphasis is placed on specific nutritional concerns for Santonicola, A.; De Bartolomeis, F.; each of these conditions from the combined point of view of gastroenterology and immunology, in Stellato, C.; Cianferoni, A.; Casolaro, an attempt to offer a useful tool to practicing physicians in discriminating these diverging disease V.; Iovino, P. -

Histamine and Antihistamines Sites of Action Conditions Which Cause Release Aron H
Learning Objectives I Histamine Pharmacological effects Histamine and Antihistamines Sites of action Conditions which cause release Aron H. Lichtman, Ph.D. Diagnostic uses Associate Professor II Antihistamines acting at the H1 and H2 receptor Pharmacology and Toxicology Pharmacological effects Mechanisms of action Therapeutic uses Side effects and drug interactions Be familiar with the existence of the H3 receptor III Be able to describe the main mechanism of action of cromolyn sodium and its clinical uses Histamine Pharmacology First autacoid to be discovered. (Greek: autos=self; Histamine Formation akos=cure) Synthesized in 1907 Synthesized in mammalian tissues by Demonstrated to be a natural constituent of decarboxylation of the amino acid l-histidine mammalian tissues (1927) Involved in inflammatory and anaphylactic reactions. Local application causes swelling redness, and edema, mimicking a mild inflammatory reaction. Large systemic doses leads to profound vascular changes similar to those seen after shock or anaphylactic origin Histamine Stored in complex with: Heparin Chondroitin Sulfate Eosinophilic Chemotactic Factor Neutrophilic Chemotactic Factor Proteases 1 Conditions That Release Histamine 1. Tissue injury: Any physical or chemical agent that injures tissue, skin or mucosa are particularly sensitive to injury and will cause the immediate release of histamine from mast cells. 2. Allergic reactions: exposure of an antigen to a previously sensitized (exposed) subject can immediately trigger allergic reactions. If sensitized by IgE antibodies attached to their surface membranes will degranulate when exposed to the appropriate antigen and release histamine, ATP and other mediators. 3. Drugs and other foreign compounds: morphine, dextran, antimalarial drugs, dyes, antibiotic bases, alkaloids, amides, quaternary ammonium compounds, enzymes (phospholipase C). -

Synergistic Action of 5-HT2A Antagonists and Selective Serotonin Reuptake Inhibitors in Neuropsychiatric Disorders
Neuropsychopharmacology (2003) 28, 402–412 & 2003 Nature Publishing Group All rights reserved 0893-133X/03 $25.00 www.neuropsychopharmacology.org Synergistic Action of 5-HT2A Antagonists and Selective Serotonin Reuptake Inhibitors in Neuropsychiatric Disorders ,1 2 3 2 Gerard J Marek* , Linda L Carpenter , Christopher J McDougle and Lawrence H Price 1Department of Psychiatry, Yale School of Medicine, New Haven, CT, USA; 2Department of Psychiatry and Human, Brown Medical School, Mood 3 Disorders Program, Behavior, Butler Hospital, Providence, RI, USA; Department of Psychiatry, Indiana University School of Medicine, Indianapolis, IN, USA Recently, the addition of drugs with prominent 5-HT2 receptor antagonist properties (risperidone, olanzapine, mirtazapine, and mianserin) to selective serotonin reuptake inhibitors (SSRIs) has been shown to enhance therapeutic responses in patients with major depression and treatment-refractory obsessive–compulsive disorder (OCD). These 5-HT antagonists may also be effective in 2 ameliorating some symptoms associated with autism and other pervasive developmental disorders (PDDs). At the doses used, these drugs would be expected to saturate 5-HT2A receptors. These findings suggest that the simultaneous blockade of 5-HT2A receptors and activation of an unknown constellation of other 5-HT receptors indirectly as a result of 5-HT uptake inhibition might have greater therapeutic efficacy than either action alone. Animal studies have suggested that activation of 5-HT1A and 5-HT2C receptors may counteract the effects of activating 5-HT2A receptors. Additional 5-HT receptors, such as the 5-HT1B/1D/5/7 receptors, may similarly counteract the effects of 5-HT receptor activation. These clinical and preclinical observations suggest that the combination of highly 2A selective 5-HT antagonists and SSRIs, as well as strategies to combine high-potency 5-HT receptor and 5-HT transporter blockade in 2A 2A a single compound, offer the potential for therapeutic advances in a number of neuropsychiatric disorders. -

Assessment Report
19 September 2013 EMA/737723/2013 Committee for Medicinal Products for Human Use (CHMP) Assessment report ABILIFY MAINTENA International non-proprietary name: ARIPIPRAZOLE Procedure No. EMEA/H/C/002755/0000 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. 7 Westferry Circus ● Canary Wharf ● London E14 4HB ● United Kingdom Telephone +44 (0)20 7418 8400 Facsimile +44 (0)20 7418 8613 E -mail [email protected] Website www.ema.europa.eu An agency of the European Union © European Medicines Agency, 2013. Reproduction is authorised provided the source is acknowledged. Table of contents 1.1. Submission of the dossier .................................................................................... 6 1.2. Manufacturers ................................................................................................... 6 1.3. Steps taken for the assessment of the product ....................................................... 7 2. Scientific discussion ................................................................................ 7 2.1. Introduction ...................................................................................................... 7 2.2. Quality aspects .................................................................................................. 9 2.2.1. Introduction ................................................................................................... 9 2.2.2. Active Substance .......................................................................................... -

Histamine, Metabolic Remodelling and Angiogenesis: a Systems Level Approach †
biomolecules Review Histamine, Metabolic Remodelling and Angiogenesis: A Systems Level Approach † Aurelio A. Moya-García 1,2,‡ , Almudena Pino-Ángeles 3,4,‡, Francisca Sánchez-Jiménez 5,§, José Luis Urdiales 1,2,5,* and Miguel Ángel Medina 1,2,5 1 Departamento de Biología Molecular y Bioquímica, Universidad de Málaga, 29071 Málaga, Spain; [email protected] (A.A.M.-G.); [email protected] (M.Á.M.) 2 Instituto de Investigación Biomédica de Málaga (IBIMA), 29010 Málaga, Spain 3 Unidad de Lípidos y Arteriosclerosis, Servicio de Medicina Interna, Hospital Universitario Reina Sofia, Instituto Maimonides de Investigación Biomédica de Córdoba (IMIBIC), Universidad de Córdoba, 14004 Córdoba, Spain; [email protected] 4 Centro de Investigación Biomédica en Red de Fisiopatología de la Obesidad y la Nutrición (CIBEROBN), Instituto de Salud Carlos III, 14004 Córdoba, Spain 5 Centro de Investigación Biomédica en Red de Enfermedades Raras (CIBERER), Instituto de Salud Carlos III, 29010 Málaga, Spain; [email protected] * Correspondence: [email protected]; Tel.: +34-9521-37285 † To Professor Rafael Peñafiel, in memoriam. ‡ These authors contributed equally to this work. § Retired; formerly as in affiliations 1 and 2. Abstract: Histamine is a highly pleiotropic biogenic amine involved in key physiological processes including neurotransmission, immune response, nutrition, and cell growth and differentiation. Its effects, sometimes contradictory, are mediated by at least four different G-protein coupled receptors, Citation: Moya-García, A.A.; which expression and signalling pathways are tissue-specific. Histamine metabolism conforms a Pino-Ángeles, A.; Sánchez-Jiménez, F.; Urdiales, J.L.; Medina, M.Á. very complex network that connect many metabolic processes important for homeostasis, including Histamine, Metabolic Remodelling nitrogen and energy metabolism. -

REMERON/Remeronsoltab with Caution These Highlights Do Not Include All the Information Needed to Use in Patients with Risk Factors for QT Prolongation
HIGHLIGHTS OF PRESCRIBING INFORMATION QT Prolongation: Use REMERON/REMERONSolTab with caution These highlights do not include all the information needed to use in patients with risk factors for QT prolongation. (5.5, 7) REMERON/REMERONSolTab safely and effectively. See full Increased Appetite/Weight Gain: REMERON/REMERONSolTab prescribing information for REMERON/REMERONSolTab. has been associated with increased appetite and weight gain. (5.6) ® REMERON (mirtazapine) tablets, for oral use Somnolence: May impair judgment, thinking and/or motor skills. ® REMERONSolTab (mirtazapine) orally disintegrating tablets Use with caution when engaging in activities requiring alertness, Initial U.S. Approval: 1996 such as driving or operating machinery. (5.7, 7) Activation of Mania/Hypomania: Screen patients for bipolar WARNING: SUICIDAL THOUGHTS AND BEHAVIORS disorder prior to initiating treatment. (2.3, 5.8) See full prescribing information for complete boxed warning. Seizures: Use with caution in patients with a seizure disorder. (5.9) Increased risk of suicidal thoughts and behavior in pediatric and Elevated Cholesterol/Triglycerides: Has been reported with young adult patients taking antidepressants. Closely monitor all REMERON use. (5.10) antidepressant-treated patients for clinical worsening and Hyponatremia: May occur as a result of treatment with emergence of suicidal thoughts and behaviors. serotonergic antidepressants, including REMERON/REMERONSolTab is not approved for use in pediatric REMERON/REMERONSolTab. (5.11) patients. (5.1, -

ARISTADA INITIO® Prescribing Information
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use ___________________ CONTRAINDICATIONS ___________________ ARISTADA INITIO® safely and effectively. See full prescribing Known hypersensitivity to aripiprazole (4). information for ARISTADA INITIO®. _______________ WARNINGS AND PRECAUTIONS _______________ ARISTADA INITIO® (aripiprazole lauroxil) extended-release injectable • Cerebrovascular Adverse Reactions in Elderly Patients with Dementia- suspension, for intramuscular use Related Psychosis: Increased incidence of cerebrovascular adverse Initial U.S. Approval: 2015 reactions (e.g., stroke, transient ischemia attack, including fatalities) (5.2). • Potential for Dosing and Medication Errors: Substitution and dispensing WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS errors between ARISTADA INITIO and ARISTADA could occur. Do not WITH DEMENTIA-RELATED PSYCHOSIS substitute ARISTADA INITIO for ARISTADA (5.3). See full prescribing information for complete boxed warning. • Neuroleptic Malignant Syndrome: Manage with immediate discontinuation and close monitoring (5.4). • Elderly patients with dementia-related psychosis treated with • Tardive Dyskinesia: Discontinue if clinically appropriate (5.5). antipsychotic drugs are at an increased risk of death. (5.1) • Metabolic Changes: Monitor for hyperglycemia, dyslipidemia, and weight • ARISTADA INITIO is not approved for the treatment of patients with gain (5.6). dementia-related psychosis. (5.1) • Pathological Gambling and Other Compulsive Behaviors: -

Download Product Insert (PDF)
PRODUCT INFORMATION Trimipramine (maleate) Item No. 15921 CAS Registry No.: 521-78-8 Formal Name: 10,11-dihydro-N,N,β-trimethyl-5H-dibenz[b,f] O azepine-5-propanamine, (2Z)-2-butenedioate MF: C20H26N2 • C4H4O4 N OH FW: 410.5 OH Purity: ≥95% O UV/Vis.: λmax: 211, 248 nm Supplied as: A crystalline solid N Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Trimipramine (maleate) is supplied as a crystalline solid. A stock solution may be made by dissolving the trimipramine (maleate) in the solvent of choice, which should be purged with an inert gas. Trimipramine (maleate) is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of trimipramine (maleate) in these solvents is approximately 3 mg/ml in ethanol and 30 mg/ml in DMSO and DMF. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of trimipramine (maleate) can be prepared by directly dissolving the crystalline solid in aqueous buffers. The solubility of trimipramine (maleate) in PBS, pH 7.2, is approximately 2 mg/ml. We do not recommend storing the aqueous solution for more than one day. Description Trimipramine is a tricyclic antidepressant.1-3 It selectively binds the serotonin (5-HT) transporter (SERT) over the norepinephrine transporter (NET) and dopamine transporter (DAT; Kds = 149, 2,450, and 3,780 nM, respectively) and acts as a histamine H1 receptor antagonist (Ki = 0.02 µM) that is selective for 1,2 histamine H1 over H2, H3, and H4 receptors (Kis = 0.04, >100, and 43.6 µM, respectively).