Assessment Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neurotransmitter Resource Guide
NEUROTRANSMITTER RESOURCE GUIDE Science + Insight doctorsdata.com Doctor’s Data, Inc. Neurotransmitter RESOURCE GUIDE Table of Contents Sample Report Sample Report ........................................................................................................................................................................... 1 Analyte Considerations Phenylethylamine (B-phenylethylamine or PEA) ................................................................................................. 1 Tyrosine .......................................................................................................................................................................................... 3 Tyramine ........................................................................................................................................................................................4 Dopamine .....................................................................................................................................................................................6 3, 4-Dihydroxyphenylacetic Acid (DOPAC) ............................................................................................................... 7 3-Methoxytyramine (3-MT) ............................................................................................................................................... 9 Norepinephrine ........................................................................................................................................................................ -

Dopamine D1 Rather Than D2 Receptor Agonists Disrupt Prepulse Inhibition of Startle in Mice
Neuropsychopharmacology (2003) 28, 108–118 & 2003 Nature Publishing Group All rights reserved 0893-133X/03 $25.00 www.neuropsychopharmacology.org Dopamine D1 Rather than D2 Receptor Agonists Disrupt Prepulse Inhibition of Startle in Mice 1 2 ,2 Rebecca J Ralph-Williams , Virginia Lehmann-Masten and Mark A Geyer* 1 2 Alcohol and Drug Abuse Research Center, Harvard Medical School and McLean Hospital, Belmont, MA, USA; Department of Psychiatry, University of California, San Diego, La Jolla, CA, USA Although substantial literature describes the modulation of prepulse inhibition (PPI) by dopamine (DA) in rats, few reports address the effects of dopaminergic manipulations on PPI in mice. We characterized the effects of subtype-specific DA agonists in the PPI paradigm to further delineate the specific influences of each DA receptor subtype on sensorimotor gating in mice. The mixed D1/D2 agonist apomorphine and the preferential D1-family agonists SKF82958 and dihydrexidine significantly disrupted PPI, with differing or no effects on startle. In contrast to findings in rats, the D2/D3 agonist quinpirole reduced startle but had no effect on PPI. Pergolide, which has affinity for D2/D3 and D1-like receptors, reduced both startle and PPI, but only at the higher, nonspecific doses. In addition, the D1-family receptor antagonist SCH23390 blocked the PPI-disruptive effects of apomorphine on PPI, but the D2-family receptor antagonist raclopride failed to alter the disruptive effect of apomorphine. These studies reveal potential species differences in the DA receptor modulation of PPI between rats and mice, where D1-family receptors may play a more prominent and independent role in the modulation of PPI in mice than in rats. -

Dopamine: a Role in the Pathogenesis and Treatment of Hypertension
Journal of Human Hypertension (2000) 14, Suppl 1, S47–S50 2000 Macmillan Publishers Ltd All rights reserved 0950-9240/00 $15.00 www.nature.com/jhh Dopamine: a role in the pathogenesis and treatment of hypertension MB Murphy Department of Pharmacology and Therapeutics, National University of Ireland, Cork, Ireland The catecholamine dopamine (DA), activates two dis- (largely nausea and orthostasis) have precluded wide tinct classes of DA-specific receptors in the cardio- use of D2 agonists. In contrast, the D1 selective agonist vascular system and kidney—each capable of influenc- fenoldopam has been licensed for the parenteral treat- ing systemic blood pressure. D1 receptors on vascular ment of severe hypertension. Apart from inducing sys- smooth muscle cells mediate vasodilation, while on temic vasodilation it induces a diuresis and natriuresis, renal tubular cells they modulate sodium excretion. D2 enhanced renal blood flow, and a small increment in receptors on pre-synaptic nerve terminals influence nor- glomerular filtration rate. Evidence is emerging that adrenaline release and, consequently, heart rate and abnormalities in DA production, or in signal transduc- vascular resistance. Activation of both, by low dose DA tion of the D1 receptor in renal proximal tubules, may lowers blood pressure. While DA also binds to alpha- result in salt retention and high blood pressure in some and beta-adrenoceptors, selective agonists at both DA humans and in several animal models of hypertension. receptor classes have been studied in the treatment of -

TECHNISCHE UNIVERSITÄT MÜNCHEN Large Scale
TECHNISCHE UNIVERSITÄT MÜNCHEN Lehrstuhl für Genomorientierte Bioinformatik Large Scale Knowledge Extraction from Biomedical Literature Based on Semantic Role Labeling Thorsten Barnickel Vollständiger Abdruck der von der Fakultät Wissenschaftszentrum Weihenstephan für Ernährung, Landnutzung und Umwelt der Technischen Universität München zur Erlangung des akademischen Grades eines Doktors der Naturwissenschaften genehmigten Dissertation. Vorsitzende: Univ.‐Prof. Dr. I. Antes Prüfer der Dissertation: 1. Univ.‐Prof. Dr. H.‐W. Mewes 2. Univ.‐Prof. Dr. R. Zimmer (Ludwig‐Maximilians‐Universität München) Die Dissertation wurde am 30. Juli bei der Technischen Universität München eingereicht und durch die Fakultät Wissenschaftszentrum Weihenstephan für Ernährung, Landnutzung und Umwelt am 25. November 2009 angenommen. ACKNOWLEDGEMENTS First and foremost, I would like to express my deep gratitude to my promoter Dr. Volker Stümpflen. Without his continuing, stimulating encouragement and his excellent background in Enterprise technologies still being predominantly used in the IT-industry rather than in academic research, I would not have been able to finish my doctorate in the presented form. Facing the tremendous amount of data that was generated by gathering the positional information of millions of biomedical terms, I was close to cutting the project down to a notably smaller version compared to the text mining system presented in this thesis. Volkers knowledge on database servers and performance tuning significantly contributed to the development of a database schema finally being able to cope with the immense amount of data. I would also like to cordially thank Prof. Dr. Hans-Werner Mewes, head of the Institute for Bioinformatics and Systems Biology (IBIS), for giving me the opportunity to do my doctorate at his institute and for his friendly support and encouragement all along my time at IBIS. -
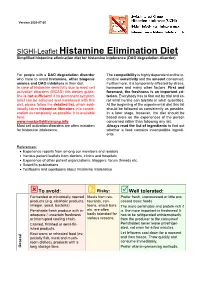
SIGHI-Leaflet Histamine Elimination Diet Simplified Histamine Elimination Diet for Histamine Intolerance (DAO Degradation Disorder)
Version 2020-07-20 SIGHI-Leaflet Histamine Elimination Diet Simplified histamine elimination diet for histamine intolerance (DAO degradation disorder) For people with a DAO degradation disorder The compatibility is highly dependent on the in- who have to avoid histamine, other biogenic dividual sensitivity and the amount consumed. amines and DAO inhibitors in their diet. Furthermore, it is temporarily affected by stress, In case of histamine sensitivity due to mast cell hormones and many other factors. First and activation disorders (MCAD) this dietary guide- foremost, the freshness is an important cri- line is not sufficient! If no permanent symptom terion. Everybody has to find out by trial and er- relief can be achieved and maintained with this ror what he/she can tolerate in what quantities. diet, please follow the detailed list, which addi- At the beginning of the experimental diet this list tionally takes histamine liberators into consid- should be followed as consistently as possible. eration as completely as possible. It is available In a later stage, however, the diet should be here: based more on the experiences of the person www.mastzellaktivierung.info concerned rather than following any list. Mast cell activation disorders are often mistaken Always read the list of ingredients to find out for histamine intolerance. whether a food contains incompatible ingredi- ents. References: • Experience reports from among our members and readers • Various patient leaflets from doctors, clinics and hospitals • Experience of other patient organizations, bloggers, forum threads etc. • Scientific publications • Textbooks and cookbooks about histamine intolerance To avoid: ? Risky: Well tolerated: Fermented or microbially ripened Meals from res- Prefer fresh, unprocessed or little pro- products (e.g. -

2D6 Substrates 2D6 Inhibitors 2D6 Inducers
Physician Guidelines: Drugs Metabolized by Cytochrome P450’s 1 2D6 Substrates Acetaminophen Captopril Dextroamphetamine Fluphenazine Methoxyphenamine Paroxetine Tacrine Ajmaline Carteolol Dextromethorphan Fluvoxamine Metoclopramide Perhexiline Tamoxifen Alprenolol Carvedilol Diazinon Galantamine Metoprolol Perphenazine Tamsulosin Amiflamine Cevimeline Dihydrocodeine Guanoxan Mexiletine Phenacetin Thioridazine Amitriptyline Chloropromazine Diltiazem Haloperidol Mianserin Phenformin Timolol Amphetamine Chlorpheniramine Diprafenone Hydrocodone Minaprine Procainamide Tolterodine Amprenavir Chlorpyrifos Dolasetron Ibogaine Mirtazapine Promethazine Tradodone Aprindine Cinnarizine Donepezil Iloperidone Nefazodone Propafenone Tramadol Aripiprazole Citalopram Doxepin Imipramine Nifedipine Propranolol Trimipramine Atomoxetine Clomipramine Encainide Indoramin Nisoldipine Quanoxan Tropisetron Benztropine Clozapine Ethylmorphine Lidocaine Norcodeine Quetiapine Venlafaxine Bisoprolol Codeine Ezlopitant Loratidine Nortriptyline Ranitidine Verapamil Brofaramine Debrisoquine Flecainide Maprotline olanzapine Remoxipride Zotepine Bufuralol Delavirdine Flunarizine Mequitazine Ondansetron Risperidone Zuclopenthixol Bunitrolol Desipramine Fluoxetine Methadone Oxycodone Sertraline Butylamphetamine Dexfenfluramine Fluperlapine Methamphetamine Parathion Sparteine 2D6 Inhibitors Ajmaline Chlorpromazine Diphenhydramine Indinavir Mibefradil Pimozide Terfenadine Amiodarone Cimetidine Doxorubicin Lasoprazole Moclobemide Quinidine Thioridazine Amitriptyline Cisapride -

THE BIOSYNTHESIS of SOME PHENOLIC ALKALOIDS a Thesis Submitted by GEOFFREY MELVILLE THOMAS for the Degree of DOCTOR of PHILOSOPH
/1 THE BIOSYNTHESIS OF SOME PHENOLIC ALKALOIDS a thesis submitted by GEOFFREY MELVILLE THOMAS for the degree of DOCTOR OF PHILOSOPHY of THE UNIVERSITY OF LONDON Imperial College, June 1963. London, S. W.7. ABSTRACT A brief review of the biosynthesis of alkaloids, other than those of the Amaryllidaceae and morphine groups, is given. The biosynthesis of these two groups is discussed more fully with particular reference to the evidence for the Barton and Cohen concept of phenol oxidation as a biogenetic mechanism. The incorporation of labelled phenolic precursors, derivatives of norbelladine, has been shown and by means of multiple labelled experiments incorporation as a whole, without degradation, has been proved. Other experiments described have thrown light on the earlier stages of biogenesis. The norlaudanosine derivative, (±) reticuline, has been shown to be incorporated into morphine, and an in vitro synthesis of thebaine from (±) reticuline using a radiochemical dilution method is de-scribed. I am deeply grateful to Professor D. H. R. Barton and Dr. G. W. Kirby for the privilege and pleasure of working under their supervision and for their great help in matters chemical and non-chemical. To the Salters Company I would like to express my sincere thanks for the award of a scholarship and for their interest during the tenure of it. My thanks are also due to Dr. D. W. Turner for advice on counting techniques, Mr. D. Aldrich and his staff for valuable technical assistance, Miss J. Cuckney for microanalyses, Mr. R.H. Young who grew the daffodils and poppies and to my many friends and co-workers at Imperial College. -

THE USE of MIRTAZAPINE AS a HYPNOTIC O Uso Da Mirtazapina Como Hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa
ARTIGO ESPECIAL THE USE OF MIRTAZAPINE AS A HYPNOTIC O uso da mirtazapina como hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa Prescription of approved hypnotics for insomnia decreased by more than 50%, whereas of antidepressive agents outstripped that of hypnotics. However, there is little data on their efficacy to treat insomnia, and many of these medications may be associated with known side effects. Antidepressants are associated with various effects on sleep patterns, depending on the intrinsic pharmacological properties of the active agent, such as degree of inhibition of serotonin or noradrenaline reuptake, effects on 5-HT1A and 5-HT2 receptors, action(s) at alpha-adrenoceptors, and/or histamine H1 sites. Mirtazapine is a noradrenergic and specific serotonergic antidepressive agent that acts by antagonizing alpha-2 adrenergic receptors and blocking 5-HT2 and 5-HT3 receptors. It has high affinity for histamine H1 receptors, low affinity for dopaminergic receptors, and lacks anticholinergic activity. In spite of these potential beneficial effects of mirtazapine on sleep, no placebo-controlled randomized clinical trials of ABSTRACT mirtazapine in primary insomniacs have been conducted. Mirtazapine was associated with improvements in sleep on normal sleepers and depressed patients. The most common side effects of mirtazapine, i.e. dry mouth, drowsiness, increased appetite and increased body weight, were mostly mild and transient. Considering its use in elderly people, this paper provides a revision about studies regarding mirtazapine for sleep disorders. KEYWORDS: sleep; antidepressive agents; sleep disorders; treatment� A prescrição de hipnóticos aprovados para insônia diminuiu em mais de 50%, enquanto de antidepressivos ultrapassou a dos primeiros. -

Reference 8 Huang Repurposing Psychiatric Drugs for Cancer 18
Cancer Letters 419 (2018) 257e265 Contents lists available at ScienceDirect Cancer Letters journal homepage: www.elsevier.com/locate/canlet Mini-review Repurposing psychiatric drugs as anti-cancer agents * Jing Huang a, b, c, d, Danwei Zhao e, Zhixiong Liu a, Fangkun Liu a, a Department of Neurosurgery, Xiangya Hospital, Central South University (CSU), Changsha, China b Department of Psychiatry, The Second Xiangya Hospital, Central South University, Changsha, Hunan, 410011, China c Mental Health Institute of the Second Xiangya Hospital, Central South University, Chinese National Clinical Research Center for Mental Disorders (Xiangya), Changsha, Hunan, 410011, China d Chinese National Technology Institute on Mental Disorders, Hunan Key Laboratory of Psychiatry and Mental Health, Changsha, Hunan, 410011, China e Xiangya Medical School, Central South University, Changsha, Hunan, China article info abstract Article history: Cancer is a major public health problem and one of the leading contributors to the global disease burden. Received 10 November 2017 The high cost of development of new drugs and the increasingly severe burden of cancer globally have Received in revised form led to increased interest in the search and development of novel, affordable anti-neoplastic medications. 17 January 2018 Antipsychotic drugs have a long history of clinical use and tolerable safety; they have been used as good Accepted 19 January 2018 targets for drug repurposing. Being used for various psychiatric diseases for decades, antipsychotic drugs are now reported to have potent anti-cancer properties against a wide variety of malignancies in addition Keywords: to their antipsychotic effects. In this review, an overview of repurposing various psychiatric drugs for Antipsychotic drugs Drug repurposing cancer treatment is presented, and the putative mechanisms for the anti-neoplastic actions of these Cancer treatment antipsychotic drugs are reviewed. -

Mrx CLINICAL ALERT
MRx AUGUST 2018 CLINICAL ALERT YOUR MONTHLY SOURCE FOR DRUG INFORMATION HIGHLIGHTS HOT TOPIC: potential to placebo in non-dependent FIRST DRUG COMPRISED adult recreational drug users. EDITORIAL OF ACTIVE MARIJUANA DERIVATIVE APPROVED Cannabidiol oral solution was studied STAFF in 3 randomized, double-blind, placebo- Under Priority review, the United States controlled clinical trials including 516 (US) Food and Drug Administration (FDA) patients with either LGS or Dravet EDITOR IN CHIEF approved cannabidiol oral solution syndrome. Cannabidiol taken with ® Maryam Tabatabai (Epidiolex ) for the treatment of the patient’s current anticonvulsant PharmD seizures associated with Lennox-Gastaut regimen was shown to be effective syndrome (LGS) or Dravet syndrome in in reducing the frequency of seizures patients ≥ 2 years of age. It is the only when compared with placebo. Over EXECUTIVE EDITOR drug approved to treat Dravet syndrome the 12-week treatment period, the Carole Kerzic and the FDA designated it as an Orphan reduction in median number of LGS RPh drug and Rare pediatric disease drug seizures ranged from 37% to 44% with to treat both serious, difficult-to-treat CBD and 17% to 22% with placebo. DEPUTY EDITORS childhood seizure disorders. Dravet For Dravet syndrome, seizure reductions Stephanie Christofferson syndrome is diagnosed in approximately were 39% and 13% with CBD and PharmD 1 in 15,700 individuals in the US and placebo, respectively. Common side is characterized by frequent prolonged effects (≥ 10%) reported with CBD Jessica Czechowski seizures and developmental delays. LGS were increased liver transaminases PharmD involves frequent drop seizures and (particularly with concurrent use of impaired intellectual development. -

Drug Class Review on Atypical Antipsychotic Drugs
Drug Class Review on Atypical Antipsychotic Drugs Final Report April 2006 The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of, or recommendation for, any particular drug, use or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Marian S. McDonagh, PharmD Kim Peterson, MS Susan Carson, MPH Oregon Evidence-based Practice Center Oregon Health & Science University Mark Helfand, MD, MPH, Director Copyright © 2006 by Oregon Health & Science University Portland, Oregon 97201. All rights reserved. Final Report Update 1 Drug Effectiveness Review Project TABLE OF CONTENTS INTRODUCTION............................................................................................................. 5 Scope and Key Questions ......................................................................................................13 METHODS .................................................................................................................... 15 Literature Search ....................................................................................................................15 Study Selection .......................................................................................................................15 Data Abstraction .....................................................................................................................15 -
How CATIE Brought Us Back to Kansas: a Critical Re-Evaluation of the Concept of Atypical Antipsychotics and Their Place In
Advances in Psychiatric Treatment (2008), vol. 14, 17–28 doi: 10.1192/apt.bp.107.003970 How CATIE brought us back to Kansas: a critical re-evaluation of the concept of atypical antipsychotics and their place in the treatment of schizophrenia David Cunningham Owens Abstract The subdivision of the class of antipsychotic drugs into two discrete groups – ‘conventional’ (or first generation) and ‘atypical’ (or second generation) – has been adopted as standard, with the latter generally accepted as ‘better’ and widely recommended as automatic first-line choices. However, this perception has been thrown into confusion with the results of large pragmatic trials that failed to identify advantages with the new, more expensive drugs, while identifying worrying tolerability issues. This article explores the origins of ‘atypicality’, its construction on the back of a confusing and weak clinical validator (diminished liability to promote parkinsonism) and how even in relation to the archetypical atypical, clozapine, the uncertain boundaries of drug-induced extrapyramidal dysfunction may be contributing to confusion about ‘efficacy’ and ‘tolerability’. It argues that abandoning atypicality would open up clinical practice to all drugs of a single class of ‘antipsychotics’ and allow for individualised risk/benefit appraisal as a basis for truly tailored treatment recommendations. Sometimes, the best way forward is back – to take This article raises fundamental questions about stock, appraise anew, admit mistakes. This is never our understanding of the clinical pharmacology easy, especially if shadows haunt the way but, if of antipsychotic drugs – so fundamental that (as necessary, is better undertaken sooner than later – numerous publication rejections attest) they were and with honesty.