Journal of Cardiovascular Computed Tomography 9 (2015) 475E492
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Congenital Heart Disease
GUEST EDITORIAL Congenital heart disease Pediatric Anesthesia is the only anesthesia journal ded- who developed hypoglycemia were infants. (9). Steven icated exclusively to perioperative issues in children and Nicolson take the opposite approach of ‘first do undergoing procedures under anesthesia and sedation. no harm’ (10). If we do not want ‘tight glycemic con- It is a privilege to be the guest editor of this special trol’ because of concern about hypoglycemic brain issue dedicated to the care of children with heart dis- injury, when should we start treating blood sugars? ease. The target audience is anesthetists who care for There are no clear answers based on neurological out- children with heart disease both during cardiac and comes in children. non-cardiac procedures. The latter takes on increasing Williams and Cohen (11) discuss the care of low importance as children with heart disease undergoing birth weight (LBW) infants and their outcomes. Pre- non-cardiac procedures appear to be at a higher risk maturity and LBW are independent risk factors for for cardiac arrest under anesthesia than those without adverse outcomes after cardiac surgery. Do the anes- heart disease (1). We hope the articles in this special thetics we use add to this insult? If prolonged exposure issue will provide guidelines for management and to volatile anesthetics is bad for the developing neona- spark discussions leading to the production of new tal brain, would avoiding them make for improved guidelines. outcomes? Wise-Faberowski and Loepke (12) review Over a decade ago Austin et al. (2) demonstrated the current research in search of a clear answer and the benefits of neurological monitoring during heart conclude that there isn’t one. -

Pediatric Radiology
2013 RSNA (Filtered Schedule) Sunday, December 01, 2013 10:30-12:00 PM • VSPD11 • Room: S100AB • Pediatric Radiology Series: Pediatric Neuroimaging I 10:45-12:15 PM • SPOI11 • Room: E353C • Oncodiagnosis Panel: Pediatric Sarcoma (An Interactive Session) 12:30-01:00 PM • CL-PDS-SUA • Room: S101AB • Pediatric Radiology - Sunday Posters and Exhibits (12:30pm - 1:00pm) 01:00-01:30 PM • CL-PDS-SUB • Room: S101AB • Pediatric Radiology - Sunday Posters and Exhibits (1:00pm - 1:30pm) 02:00-03:30 PM • VSPD12 • Room: S102AB • Pediatric Radiology Series: Pediatric Musculoskeletal Monday, December 02, 2013 08:30-10:00 AM • RC224 • Room: E353B • Mentored Case Approach to Pediatric Cardiovascular Disease 1: Vascular Disease (An Interactive Session) 08:30-12:00 PM • VSPD21 • Room: S102AB • Pediatric Radiology Series: Fetal - Neonatal Imaging 12:15-12:45 PM • CL-PDS-MOA • Room: S101AB • Pediatric Radiology - Monday Posters and Exhibits (12:15pm - 12:45pm) 12:45-01:15 PM • CL-PDS-MOB • Room: S101AB • Pediatric Radiology - Monday Posters and Exhibits (12:45pm - 1:15pm) 03:00-04:00 PM • SSE21 • Room: S102AB • Pediatric (Neuroimaging) Tuesday, December 03, 2013 08:30-10:00 AM • RC324 • Room: S402AB • Mentored Case Approach to Pediatric Cardiovascular Disease 2: Cardiac Disease (An Interactive Session) 08:30-12:00 PM • VSPD31 • Room: S102AB • Pediatric Radiology Series: Chest/Cardiovascular Imaging I 12:15-12:45 PM • CL-PDS-TUA • Room: S101AB • Pediatric Radiology - Tuesday Scientific Posters and Exhibits (12:15pm - 12:45pm) 12:45-01:15 PM • CL-PDS-TUB • -
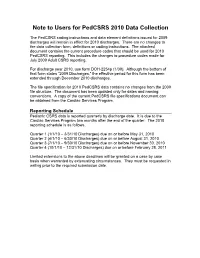
Note to Users for Pedcsrs 2010 Data Collection
Note to Users for PedCSRS 2010 Data Collection The PedCSRS coding instructions and data element definitions issued for 2009 discharges will remain in effect for 2010 discharges. There are no changes to the data collection form, definitions or coding instructions. The attached document contains the current procedure codes that should be used for 2010 PedCSRS reporting. This includes the changes to procedure codes made for July 2009 Adult CSRS reporting. For discharge year 2010, use form DOH-2254p (1/09). Although the bottom of that form states “2009 Discharges,” the effective period for this form has been extended through December 2010 discharges. The file specification for 2010 PedCSRS data contains no changes from the 2009 file structure. The document has been updated only for dates and naming conventions. A copy of the current PedCSRS file specifications document can be obtained from the Cardiac Services Program. Reporting Schedule Pediatric CSRS data is reported quarterly by discharge date. It is due to the Cardiac Services Program two months after the end of the quarter. The 2010 reporting schedule is as follows. Quarter 1 (1/1/10 – 3/31/10 Discharges) due on or before May 31, 2010 Quarter 2 (4/1/10 – 6/30/10 Discharges) due on or before August 31, 2010 Quarter 3 (7/1/10 – 9/30/10 Discharges) due on or before November 30, 2010 Quarter 4 (10/1/10 – 12/31/10 Discharges) due on or before February 28, 2011 Limited extensions to the above deadlines will be granted on a case by case basis when warranted by extenuating circumstances. -

Mustard Procedure Br Heart J: First Published As 10.1136/Hrt.72.1.85 on 1 July 1994
Br Heart J 1994;72:85-88 85 Transcatheter stent implantation for recurrent pulmonary venous pathway obstruction after the Mustard procedure Br Heart J: first published as 10.1136/hrt.72.1.85 on 1 July 1994. Downloaded from Martin C K Hosking, Kenneth A Murdison, Walter J Duncan Abstract pathway obstruction reaching a maximum A 5 year old boy presented with obstruc- flow velocity of 2'0 m/s associated with a tion of the pulmonary venous pathway stenosis measuring 2-3 mm in diameter. four years after the Mustard procedure. Right ventricular dysfunction was a persistent A successful balloon dilatation ofthe pul- echocardiographic finding associated with an monary venous pathway was performed increase in left ventricle dimension in but the benefit was transient. Placement response to the rise of pulmonary arterial of a 10 mm balloon expandable intravas- pressure secondary to the pulmonary venous cular stent across the recurrent stenosis inflow obstruction. A significant systemic to resulted in complete relief ofthe obstruc- pulmonary venous chamber baffle leak mea- tion with prompt resolution ofthe clinical suring 5 mm x 4 mm with right to left shunting signs. The delivery system was modified was seen by Doppler colour flow mapping and to facilitate stent delivery. contributed to central cyanosis. Serial chest x ray films showed persistence of cardiomegaly (Br Heart 1994;72:85-88) with increasing evidence of pulmonary venous congestion. To avoid the risks of surgical repair in a Paediatric experience with transcatheter patient with impaired -

Mustard Operation
Mustard Operation William G. Williams The natural history of infants with complete transposi- desaturation. Mustard reasoned that both vena cavae tion (TGA) is rapid deterioration and death within the could be deliberately diverted to the left atrium while first few months of life. The few babies who do survive allowing the pulmonary return to enter the right atrium, beyond the first year of life usually have an associated thereby correcting the circulation in patients with TGA. ventricular septal defect (VSD) and subsequently dete- The Mustard baffle operation was a simple, reproduc- riorate with progressive pulmonary vascular disease. ible, and elegant technique of transposing venous re- Intervention to improve the outlook for newborns turn. It was easier to learn than the Senning operation, with TGA began with surgical resection of the atrial and became the standard repair in most of the world. septum.' The enlarged atrial defect improves mixing of the pulmonary and systemic circulations, thereby in- creasing the systemic oxygen saturation. Balloon atrial Indications for the Mustard Operation in 1998 septostomy, as described by Rashkind and Miller in The atrial repair of TGA has been almost entirely 1966,2 replaced surgical septectomy. The balloon cath- replaced by the arterial switch operation. However, eter technique continues to provide effective emergency there are three situations were the Mustard operation palliation for the newborn with TGA. may be indicated: In the early 1950s, a number of surgeons, including 1. For infants with isolated TGA who first present M~stard,~attempted arterial repair of TGA in infants, after the neonatal period, the Mustard operation is an all without success until Jatene's report in 1978.4 In alternative to the two-stage arterial switch operation, 1954, Albert5 proposed a surgical technique to trans- ie, a preliminary pulmonary artery banding to prepare pose the venous inflow within the atria to correct TGA. -

Relation of Biventricular Function Quantified by Stress
Relation of Biventricular Function Quantified by Stress Echocardiography to Cardiopulmonary Exercise Capacity in Adults With Mustard (Atrial Switch) Procedure for Transposition of the Great Arteries Wei Li, Tim S. Hornung, Darrel P. Francis, Christine O’Sullivan, Alison Duncan, Michael Gatzoulis and Michael Henein Circulation 2004;110;1380-1386; originally published online Aug 23, 2004; DOI: 10.1161/01.CIR.0000141370.18560.D1 Circulation is published by the American Heart Association. 7272 Greenville Avenue, Dallas, TX 72514 Copyright © 2005 American Heart Association. All rights reserved. Print ISSN: 0009-7322. Online ISSN: 1524-4539 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circ.ahajournals.org/cgi/content/full/110/11/1380 Subscriptions: Information about subscribing to Circulation is online at http://circ.ahajournals.org/subsriptions/ Permissions: Permissions & Rights Desk, Lippincott Williams & Wilkins, 351 West Camden Street, Baltimore, MD 21202-2436. Phone 410-5280-4050. Fax: 410-528-8550. Email: [email protected] Reprints: Information about reprints can be found online at http://www.lww.com/static/html/reprints.html Downloaded from circ.ahajournals.org at NHLI - Royal Brompton on January 29, 2006 Relation of Biventricular Function Quantified by Stress Echocardiography to Cardiopulmonary Exercise Capacity in Adults With Mustard (Atrial Switch) Procedure for Transposition of the Great Arteries Wei Li, MD, PhD; Tim S. Hornung, MD; Darrel P. Francis, MRCP; Christine O’Sullivan, BSc; Alison Duncan, MRCP; Michael Gatzoulis, MD, PhD; Michael Henein, MD, PhD Background—Mustard repair for transposition of the great arteries (TGA) is frequently associated with impaired systemic (right) ventricular function and sometimes exercise intolerance. -

An Overview of Mechanical Circulatory Support in Single-Ventricle Patients
161 Review Article An overview of mechanical circulatory support in single-ventricle patients Jacob R. Miller1, Timothy S. Lancaster1, Connor Callahan2, Aaron M. Abarbanell3, Pirooz Eghtesady3 1Division of Cardiothoracic Surgery, 2Department of Surgery, Barnes-Jewish Hospital/Washington University School of Medicine, St. Louis, MO, USA; 3Section of Pediatric Cardiothoracic Surgery, St. Louis Children’s Hospital/Washington University School of Medicine, St. Louis, MO, USA Contributions: (I) Conception and design: JR Miller, AM Abarbanell, P Eghtesady; (II) Administrative support: AM Abarbanell, P Eghtesady; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: JR Miller, TS Lancaster, C Callahan; (V) Data analysis and interpretation: JR Miller, AM Abarbanell, P Eghtesady; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Pirooz Eghtesady, MD, PhD. Chief of Pediatric Cardiothoracic Surgery, St. Louis Children’s Hospital, One Children’s Place, Suite 5 South, St. Louis, MO 63110, USA. Email: [email protected]. Abstract: The population of people with a single-ventricle is continually increasing due to improvements across the spectrum of medical care. Unfortunately, a proportion of these patients will develop heart failure. Often, for these patients, mechanical circulatory support (MCS) represents the only available treatment option. While single-ventricle patients currently represent a small proportion of the total number of patients who receive MCS, as the single-ventricle patient population increases, this number will increase as well. Outcomes for these complex single-ventricle patients who require MCS has begun to be evaluated. When considering the entire population, survival to hospital discharge is 30–50%, though this must be considered with the significant heterogeneity of the single-ventricle patient population. -

Outcome of the Norwood Operation in Patients with Hypoplastic Left Heart Syndrome: a 12-Year Single-Center Survey
Furck et al Congenital Heart Disease Outcome of the Norwood operation in patients with hypoplastic left heart syndrome: A 12-year single-center survey Anke Katharina Furck, MD,a Anselm Uebing, MD,a Jan Hinnerk Hansen,a Jens Scheewe, MD,b Olaf Jung, MD,a Gunther Fischer, MD,a Carsten Rickers, MD,a Tim Holland-Letz, MSc,c and Hans-Heiner Kramer, MDa Objective: Recent advances in perioperative care have led to a decrease in mortality of children with hypoplastic left heart syndrome undergoing the Norwood operation. This study aimed to evaluate the outcome of the Nor- wood operation in a single center over 12 years and to identify clinical and anatomic risk factors for adverse early CHD and longer term outcome. Methods: Full data on all 157 patients treated between 1996 and 2007 were analyzed. Results: Thirty-day mortality of the Norwood operation decreased from 21% in the first 3 years to 2.5% in the last 3 years. The estimated exponentially weighted moving average of early mortality after 157 Norwood oper- ations was 2.3%. Risk factors were an aberrant right subclavian artery, the use and duration of circulatory arrest, and the duration of total support time. The anatomic subgroup mitral stenosis/aortic atresia and female gender tended to show an increased early mortality. In the group of patients who required postoperative cardiopulmonary resuscitation, the ascending aorta was significantly smaller than in the remainder (3.03 Æ 1.05 vs 3.63 Æ 1.41 mm). Interstage mortality was 15% until the initiation of a home surveillance program in 2005, which has zeroed it so far. -

Coders' Desk Reference for ICD-10-PCS Procedures
2 0 2 DESK REFERENCE 1 ICD-10-PCS Procedures ICD-10-PCS for DeskCoders’ Reference Coders’ Desk Reference for ICD-10-PCS Procedures Clinical descriptions with answers to your toughest ICD-10-PCS coding questions Sample 2021 optum360coding.com Contents Illustrations ..................................................................................................................................... xi Introduction .....................................................................................................................................1 ICD-10-PCS Overview ...........................................................................................................................................................1 How to Use Coders’ Desk Reference for ICD-10-PCS Procedures ...................................................................................2 Format ......................................................................................................................................................................................3 ICD-10-PCS Official Guidelines for Coding and Reporting 2020 .........................................................7 Conventions ...........................................................................................................................................................................7 Medical and Surgical Section Guidelines (section 0) ....................................................................................................8 Obstetric Section Guidelines (section -

Echocardiographic Assessment of TGA After Atrial Switch Repair
Echocardiographic assessment of TGA after Atrial switch repair Session 6. Transposition of the great arteries Multimodality Imaging in ACHD and PH Annemien van den Bosch Erasmus MC, Thoraxcenter, Rotterdam, The Netherlands Transposition of the Great Arteries . Mustard and Senning operations establish appropriate connection - between systemic venous pathways and subpulmonic ventricle - between pulmonary venous pathway and the systemic ventricle . At the expense of a morphological RV support systemic circulation Atrial switch operation Mustard Procedure: Uses baffles made from Dacron, GoreTex or pericardial tissue to redirect flow Hans Hamer© Atrial switch operation Senning Procedure: Uses tissue from the right atrium and the atrial septum to redirect flow. Diagrams from Popelova et al Post-operative Sequelae Baffle problems . Baffle obstruction - SVC baffle obstruction more common following Mustard operation 5-10% superior, 1% inferior - PV baffle obstruction is more common following Senning operation . Baffle leaks - Small leaks are common and not haemodynamically 25% important, except in the case of cryptogenic stroke - Large leaks are rarer but important due to associated volume overload 1-2 re-op% Post-operative Sequelae . Systemic RV - Hypertrophy - Dilatation (lack of reference values for systemic RV) - Systolic function invariably deteriorates over time . Tricuspid regurgitation - TR is predominantly due to annular dilatation and is likely functional rather than due to primary organic abnormality. In rare cases, structural tricuspid -

Dyssynchrony and Electromechanical Delay.Pdf
TGA, Fibrosis, LAX and TR - 1 - Babu-Narayan SV, Prati D -et - al. 1 - - - - 1 - - Dyssynchrony and Electromechanical delay are associated with focal fibrosis in the Systemic Right Ventricle – Insights from Echocardiography Sonya V. Babu-Narayan*, BSc MRCP PhD 1,2,3, Daniele Prati*, MD 1,3,4, Riikka Rydman MD PhD1,2,3,5 , Konstantinos Dimopoulos, MD PhD 1,3, Gerhard P. Diller, MD PhD 1,3, Anselm Uebing MD PhD, 1 Michael Y. Henein, MD PhD 3, Philip J. Kilner, MD PhD 2,3, Michael A. Gatzoulis, MD PhD1,3, **Wei Li, MD PhD1,3. 1 Adult Congenital Heart Unit, Royal Brompton Hospital, Sydney Street, London SW3 6NP, UK. 2 NIHR cardiovascular Biomedical Research Unit, Royal Brompton Hospital, Sydney Street, London SW3 6NP, UK. 3 National Heart and Lung Institute, Imperial College, Dovehouse Street, London SW3 6LY, UK. 4 Department of Biomedical and Surgical Sciences, Section of Cardiology, Universita’ degli Studi di Verona, Verona, Italy 5 Department of Molecular Medicine and Surgery, Section of Clinical Physiology, at Karolinska Institutet, Stockholm, Sweden 1-5 This author takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation. No conflicts of interest. * The first and second author contributed equally to the work **Corresponding Author: Wei Li MD PhD, Adult Congenital Heart Program Royal Brompton Hospital, Sydney Street, SW3 6NP London, UK Tel. + 44 (0) 207 351 8602, Fax + 44 (0) 207 351 8629 E-mail: [email protected] Word Count (including references, figure legends and tables); 5294 Abstract: 238 words Figures and Tables: 4 figures, 2 tables Keywords Systemic right ventricle, transposition of the great arteries, long axis function, tissue Doppler imaging, fibrosis, late gadolinium enhancement TGA, Fibrosis, LAX and TR - 2 - Babu-Narayan SV, Prati D -et - al. -

Arterial Switch for Pulmonary Venous Obstruction Complicating Mustard
Ann Thorac Surg CASE REPORT DE JONG ET AL 1005 1995;59:1005-7 ARTERIAL SWITCH AFTER MUSTARD PROCEDURE References Table I. Variables Before Arterial Switch Procedure 1. Mork Jp, Gersony WM. Progressive atrioventricular regurgi- Variable Patient 1 Patient 2 tation in single ventricle. Am J Cardiol 1987;59:658. 2. Yutaka O, Miki S, Kusuhara K, et al. Annuloplastic recon- Weight (kg) struction for common atrioventricular valvular regurgitation Electrocardiogram Biventricular Biventricular in right isomerism. Ann Thorac Surg 1989;47:302-4. hypertrophy hypertrophy Echocardiography Diastolic left 8 (95th 6 (75th ventricular percentile) percentile) posterior wall thickness (ram) Arterial Switch for Pulmonary Shortening fraction 0.30 0.29 Cardiac catheterization Venous Obstruction Complicating Ejection fraction 0.70 0.65 Mustard Procedure Left ventricular 80/5-10 71/1-7 Peter L. de Jong, MD, Ad J. J. C. Bogers, MD, PhD, pressure (mm Hg) Pulmonary artery 69/36 68/39 Maarten Witsenburg, MD, PhD, and Egbert Bos, MD, pressure (ram Hg) PhD Mean capillary wedge 29 30 pressure (mm Hg) Departments of Thoracic Surgery and Pediatric Cardiology, Sophia/Dijkzigt University Hospital, Rotterdam, the Right ventricular 91/0-10 95/1-8 Netherlands pressure (rnm Hg) Left ventricular-to- 0.88 0.75 right ventricular Two patients underwent an arterial switch procedure for ratio the relief of severe pulmonary venous obstruction com- plicating a Mustard procedure. Without preparatory pul- monary banding, both patients had adequate left ventric- symptomatic pulmonary venous obstruction, without the ular function due to secondary pulmonary hypertension. need for preparatory pulmonary artery banding. At 8 and 4 years after the procedure, both patients are in New York Heart Association functional class I, with echocardiographic evidence of good left and right ven- Case Reports tricular function.