Healthcare Bulletin |
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Direct Effects of the Angiotensin-Converting Enzyme
European Journal of Endocrinology (2006) 154 355–361 ISSN 0804-4643 EXPERIMENTAL STUDY The direct effects of the angiotensin-converting enzyme inhibitors, zofenoprilat and enalaprilat, on isolated human pancreatic islets Roberto Lupi, Silvia Del Guerra, Marco Bugliani, Ugo Boggi1, Franco Mosca1, Scilla Torri, Stefano Del Prato and Piero Marchetti Metabolic Unit, Department of Endocrinology and Metabolism, University of Pisa, Ospedale Cisanello, via Paradisa 2, 56100 Pisa, Italy and 1Transplant Unit, Department of Oncology, University of Pisa, Pisa, Italy, Menarini Ricerche SpA, Florence, Italy (Correspondence should be addressed to P Marchetti; Email: [email protected]) Abstract Objective: Data from prospective studies suggest a significant reduction in the risk of new diabetes from drug therapies containing angiotensin-converting enzyme (ACE) inhibitors. Since the renin–angio- tensin system (RAS) has been found locally in several tissues and cells, including pancreatic islets, we hypothesized that the positive metabolic effects of ACE inhibitors may be due to a beneficial action of these compounds on insulin-secreting b-cells. Design and methods: Isolated human pancreatic islets were studied after 24 h of incubation with 22.2 mmol/l glucose, with or without the presence in the incubation medium of 0.5–6.0 mmol/l zofe- noprilat or enalaprilat, ACE inhibitor drugs which differ by the presence of a sulphydryl or a carboxyl group in their structural formula. Functional and molecular studies were then performed to assess insulin secretion, redox balance, mRNA and protein expression. Results: Angiotensinogen, ACE and angiotensin type 1 receptor mRNA expression increased in islets cultured in high glucose; this was similarly prevented by the presence of either ACE inhibitor. -

A Global Review on Short Peptides: Frontiers and Perspectives †
molecules Review A Global Review on Short Peptides: Frontiers and Perspectives † Vasso Apostolopoulos 1 , Joanna Bojarska 2,* , Tsun-Thai Chai 3 , Sherif Elnagdy 4 , Krzysztof Kaczmarek 5 , John Matsoukas 1,6,7, Roger New 8,9, Keykavous Parang 10 , Octavio Paredes Lopez 11 , Hamideh Parhiz 12, Conrad O. Perera 13, Monica Pickholz 14,15, Milan Remko 16, Michele Saviano 17, Mariusz Skwarczynski 18, Yefeng Tang 19, Wojciech M. Wolf 2,*, Taku Yoshiya 20 , Janusz Zabrocki 5, Piotr Zielenkiewicz 21,22 , Maha AlKhazindar 4 , Vanessa Barriga 1, Konstantinos Kelaidonis 6, Elham Mousavinezhad Sarasia 9 and Istvan Toth 18,23,24 1 Institute for Health and Sport, Victoria University, Melbourne, VIC 3030, Australia; [email protected] (V.A.); [email protected] (J.M.); [email protected] (V.B.) 2 Institute of General and Ecological Chemistry, Faculty of Chemistry, Lodz University of Technology, Zeromskiego˙ 116, 90-924 Lodz, Poland 3 Department of Chemical Science, Faculty of Science, Universiti Tunku Abdul Rahman, Kampar 31900, Malaysia; [email protected] 4 Botany and Microbiology Department, Faculty of Science, Cairo University, Gamaa St., Giza 12613, Egypt; [email protected] (S.E.); [email protected] (M.A.) 5 Institute of Organic Chemistry, Faculty of Chemistry, Lodz University of Technology, Zeromskiego˙ 116, 90-924 Lodz, Poland; [email protected] (K.K.); [email protected] (J.Z.) 6 NewDrug, Patras Science Park, 26500 Patras, Greece; [email protected] 7 Department of Physiology and Pharmacology, -

Ovid MEDLINE(R)
Supplementary material BMJ Open Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily <1946 to September 16, 2019> # Searches Results 1 exp Hypertension/ 247434 2 hypertens*.tw,kf. 420857 3 ((high* or elevat* or greater* or control*) adj4 (blood or systolic or diastolic) adj4 68657 pressure*).tw,kf. 4 1 or 2 or 3 501365 5 Sex Characteristics/ 52287 6 Sex/ 7632 7 Sex ratio/ 9049 8 Sex Factors/ 254781 9 ((sex* or gender* or man or men or male* or woman or women or female*) adj3 336361 (difference* or different or characteristic* or ratio* or factor* or imbalanc* or issue* or specific* or disparit* or dependen* or dimorphism* or gap or gaps or influenc* or discrepan* or distribut* or composition*)).tw,kf. 10 or/5-9 559186 11 4 and 10 24653 12 exp Antihypertensive Agents/ 254343 13 (antihypertensiv* or anti-hypertensiv* or ((anti?hyperten* or anti-hyperten*) adj5 52111 (therap* or treat* or effective*))).tw,kf. 14 Calcium Channel Blockers/ 36287 15 (calcium adj2 (channel* or exogenous*) adj2 (block* or inhibitor* or 20534 antagonist*)).tw,kf. 16 (agatoxin or amlodipine or anipamil or aranidipine or atagabalin or azelnidipine or 86627 azidodiltiazem or azidopamil or azidopine or belfosdil or benidipine or bepridil or brinazarone or calciseptine or caroverine or cilnidipine or clentiazem or clevidipine or columbianadin or conotoxin or cronidipine or darodipine or deacetyl n nordiltiazem or deacetyl n o dinordiltiazem or deacetyl o nordiltiazem or deacetyldiltiazem or dealkylnorverapamil or dealkylverapamil -

The Direct Effects of the Angiotensin-Converting Enzyme
European Journal of Endocrinology (2006) 154 355–361 ISSN 0804-4643 EXPERIMENTAL STUDY The direct effects of the angiotensin-converting enzyme inhibitors, zofenoprilat and enalaprilat, on isolated human pancreatic islets Roberto Lupi, Silvia Del Guerra, Marco Bugliani, Ugo Boggi1, Franco Mosca1, Scilla Torri, Stefano Del Prato and Piero Marchetti Metabolic Unit, Department of Endocrinology and Metabolism, University of Pisa, Ospedale Cisanello, via Paradisa 2, 56100 Pisa, Italy and 1Transplant Unit, Department of Oncology, University of Pisa, Pisa, Italy, Menarini Ricerche SpA, Florence, Italy (Correspondence should be addressed to P Marchetti; Email: [email protected]) Abstract Objective: Data from prospective studies suggest a significant reduction in the risk of new diabetes from drug therapies containing angiotensin-converting enzyme (ACE) inhibitors. Since the renin–angio- tensin system (RAS) has been found locally in several tissues and cells, including pancreatic islets, we hypothesized that the positive metabolic effects of ACE inhibitors may be due to a beneficial action of these compounds on insulin-secreting b-cells. Design and methods: Isolated human pancreatic islets were studied after 24 h of incubation with 22.2 mmol/l glucose, with or without the presence in the incubation medium of 0.5–6.0 mmol/l zofe- noprilat or enalaprilat, ACE inhibitor drugs which differ by the presence of a sulphydryl or a carboxyl group in their structural formula. Functional and molecular studies were then performed to assess insulin secretion, redox balance, mRNA and protein expression. Results: Angiotensinogen, ACE and angiotensin type 1 receptor mRNA expression increased in islets cultured in high glucose; this was similarly prevented by the presence of either ACE inhibitor. -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

Hydrogen Sulfide Accounts for the Peripheral Vascular Effects of Zofenopril Independently of ACE Inhibition
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Archivio della ricerca - Università degli studi di Napoli Federico II Cardiovascular Research (2014) 102, 138–147 doi:10.1093/cvr/cvu026 Hydrogen sulfide accounts for the peripheral vascular effects of zofenopril independently of ACE inhibition Mariarosaria Bucci1†, Valentina Vellecco1†, Anna Cantalupo1†, Vincenzo Brancaleone2, Zongmin Zhou3, Stefano Evangelista4, Vincenzo Calderone5, Andreas Papapetropoulos3, and Giuseppe Cirino1* 1Department of Pharmacy, University of Naples ‘Federico II’, Via D. Montesano 49, Naples 80131, Italy; 2Department of Science, University of Basilicata, Potenza, Italy; 3Department of Pharmacy, Laboratory for Molecular Pharmacology, University of Patras, Patra, Greece; 4Menarini Ricerche spa, Firenze, Italy; and 5Department of Pharmacy, University of Pisa, Pisa, Italy Received 21 May 2013; revised 15 January 2014; accepted 25 January 2014; online publish-ahead-of-print 5 February 2014 Time for primary review: 53 days Aims Therapeutic use of sulfhydrylated inhibitor S-zofenopril has raised different hypotheses regarding the role played by its thiol group in the beneficial clinical effects exerted compared with other angiotensin-converting enzyme (ACE) inhibi- tors. Here, we investigated hydrogen sulfide (H2S) pathwayas accountable forextra-beneficialeffectsin vascular function. ..................................................................................................................................................................................... Methods Spontaneously hypertensive rat (SHRs) and control Wistar Kyoto (WKY) rats were treated with either S-zofenopril or and results enalapril in vivo. Aorta and carotid were harvested and ex vivo vascular reactivity to acetylcholine (Ach) and L-cysteine (L-cys) assessed. Cystathionine-b-synthase (CBS), cystathionine-g-lyase (CSE), and 3-mercaptosulfur-transferase (3MST) expression, as well as H2S levels, were evaluated in both vascular tissues. -

Preclinical Profile of Zofenopril: an Angiotensin Converting Enzyme Inhibitor with Peculiar Cardioprotective Properties
Cardiovascular Drug Reviews Vol. 17, No. 2, pp. 115–133 © 1999 Neva Press, Branford, Connecticut Preclinical Profile of Zofenopril: An Angiotensin Converting Enzyme Inhibitor with Peculiar Cardioprotective Properties A. Subissi, S. Evangelista and A. Giachetti Preclinical Development, Menarini Ricerche S.p.A., Firenze, Italy. Key Words: Angiotensin-converting enzyme inhibitor—Cardioprotection—Hypertension— Sulfhydryl—Zofenopril. INTRODUCTION The discovery of captopril, the prototype of orally active angiotensin-converting en- zyme inhibitors (ACEIs), represented a major breakthrough in the treatment of cardio- vascular diseases. Currently, captopril has four important indications: hypertension, con- gestive heart failure, acute myocardial infarction, and diabetic nephropathy. After the discovery of captopril, several new ACEIs were developed and introduced into medical practice. These new ACEIs are neither chemically nor pharmacologically identical; they differ in their chemical structure, functional groups (sulfhydryl in captopril, carboxyl in enalapril, or phosphinyl in fosinopril), active moiety (some are prodrugs), potency, an- cillary pharmacology, and pharmacokinetics. These and other important characteristics differentiate ACEIs and influence their ability to inhibit the enzyme in various organs. Since ACEIs appear to work by inhibiting angiotensin-converting enzyme (ACE) in critical tissues, tissue selectivity is one of the most important properties that varies with the individual ACEIs. An important question is whether different tissue-selectivity profiles of ACEIs in ani- mal experiments are clinically relevant. Although the clinical relevance is not yet firmly established, the emerging evidence indicates that some differences among ACEIs are clinically significant (4,6,28,43). The latest ACE inhibitor to reach the European market is zofenopril calcium. By February 1999, it was registered in all 15 European Community countries. -
Angiotensin-Converting Enzyme (ACE)
Angiotensin-converting Enzyme (ACE) Angiotensin-converting enzyme (ACE) indirectly increases blood pressure by causing blood vessels to constrict. ACE does that by converting angiotensin I to angiotensin II, which constricts the vessels. ACE, angiotensin I and angiotensin II are part of the renin-angiotensin system (RAS), which controls blood pressure by regulating the volume of fluids in the body. ACE is secreted in the lungs and kidneys by cells in the endothelium (inner layer) of blood vessels. It has two primary functions: ACE catalyses the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor in a substrate concentration-dependent manner. ACE degrades bradykinin, a potent vasodilator, and other vasoactive peptides. These two actions make ACE inhibition a goal in the treatment of conditions such as high blood pressure, heart failure, diabetic nephropathy, and type 2 diabetes mellitus. Inhibition of ACE (by ACE inhibitors) results in the decreased formation of angiotensin II and decreased metabolism of bradykinin, leading to systematic dilation of the arteries and veins and a decrease in arterial blood pressure. www.MedChemExpress.com 1 Angiotensin-converting Enzyme (ACE) Inhibitors & Modulators Angiotensin 1-7 Benazepril (Angiotensin-(1-7); Ang-(1-7)) Cat. No.: HY-12403 Cat. No.: HY-B0093 Bioactivity: Angiotensin (1-7) inhibits purified canine angiotensin Bioactivity: Benazepril, an angiotensin converting enzyme inhibitor, which converting enzyme ( ACE) activity with an IC50 of 0.65 μM. is a medication used to treat high blood pressure. Purity: 99.61% Purity: >98% Clinical Data: No Development Reported Clinical Data: Launched Size: 10mM x 1mL in Water, Size: 1 g, 5 g 5 mg, 10 mg, 25 mg, 50 mg Benazepril hydrochloride Captopril (CGS14824A) Cat. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -
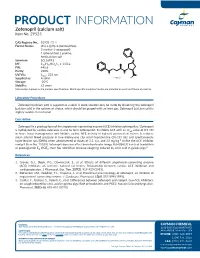
Download Product Insert (PDF)
PRODUCT INFORMATION Zofenopril (calcium salt) Item No. 29525 CAS Registry No.: 81938-43-4 Formal Name: (4S)-1-[(2S)-3-(benzoylthio)- 2-methyl-1-oxopropyl]- 4-(phenylthio)-L-proline, hemicalcium salt Synonym: SQ 26991 S MF: C22H22NO4S2 • 1/2Ca FW: 448.6 S N Purity: ≥98% O O UV/Vis.: λmax: 238 nm O Supplied as: A solid • 1/2Ca2+ -O Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Zofenopril (calcium salt) is supplied as a solid. A stock solution may be made by dissolving the zofenopril (calcium salt) in the solvent of choice, which should be purged with an inert gas. Zofenopril (calcium salt) is slightly soluble in methanol. Description Zofenopril is a prodrug form of the angiotensin-converting enzyme (ACE) inhibitor zofenoprilat.1 Zofenopril is hydrolyzed by cardiac esterases in vivo to form zofenoprilat. It inhibits ACE with an IC50 value of 0.9 nM in heart tissue homogenates and inhibits cardiac ACE activity in isolated perfused rat hearts. It reduces mean arterial blood pressure in two kidney-one clip renal hypertensive (2K-1C) rats and spontaneously hypertensive rats (SHRs) when administered at doses of 2.2, 6.6, and 22 mg/kg.2 Unlike the ACE inhibitor ramipril (Item No. 15558), zofenopril does not affect bronchoalveolar lavage fluid (BALF) levels of bradykinin 3 or prostaglandin E2 (PGE2; Item No. 14010) or increase coughing induced by citric acid in guinea pigs. References 1. Grover, G.J., Sleph, P.G., Dzwonczyk, S., et al. -

Angiotensin II Type 1 Receptor (AT1R) Changes in Animal Model of Chronic Kidney Disease: Evaluation and Pharmacotherapy
Angiotensin II Type 1 Receptor (AT1R) Changes in Animal Model of Chronic Kidney Disease: Evaluation and Pharmacotherapy By Basma Ismail Thesis submitted to the Faculty of Graduate and Posdoctoral Studies in partial fulfillment of the requirements for a doctoral degree in Cellular and Molecular Medicine. Department of Cellular and Molecular Medicine Faculty of Medicine University of Ottawa © Basma Ismail, Ottawa, Canada, 2016 Basma Ismail Evaluation of AT1 receptor in chronic kidney disease ABSTRACT Cardiovascular complications represent the leading cause of death in chronic kidney disease (CKD) patients. Significant renal mass reduction induced by 5/6 subtotal nephrectomy (Nx) animal model leads to a chain of events that culminates in hypertension and CKD. The renin angiotensin (Ang) system (RAS) is known to be dysregulated, specifically Ang type 1 receptor (AT1R) plays a major role in development and progression of the disease. However, conflicting results have been reported on intrarenal AT1R levels, and the impact of antihypertensive drugs on RAS signaling is divergent. We hypothesize that PET imaging will be able to quantify kidney AT1R expression reliably in healthy and disease states. The broad objectives of this research project were: (i) to develop a positron emission tomography (PET) probe capable of detecting changes in the AT1R binding in the kidney; (ii) to elucidate the nature/temporal role of renal AT1R in Nx rat model of CKD; and (iii) to explore the predictive value of non-invasive PET imaging of AT1R to guide the use of antihypertensive therapy in preventing the progression of the disease. The novel selective AT1R PET radioligand 18 [ F]FPyKYNE-losartan was successfully used with PET in detecting renal AT1Rs at early and late stages of the CKD. -

Zofenopril Mylan Film-Coated Tablet ENG Smpc
SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT <Invented name> 30mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each film-coated tablet contains 30mg of zofenopril calcium, equivalent to 28.7 mg of zofenopril Eccipients with known effect: lactose monohydrate and sodium. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet White, round, film-coated tablets with break line on one side. The tablet can be divided into equal doses. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Hypertension Zofenopril is indicated for the treatment of mild to moderate essential hypertension. Acute Myocardial Infarction Zofenopril is indicated for the treatment initiated within the first 24 hours of patients with acute myocardial infarction with or without signs and symptoms of heart failure, who are haemodynamically stable and have not received thrombolytic therapy. 4.2 Posology and method of administration Posology Hypertension The need for dosage titration should be determined by measurement of blood pressure just before the next dose. The dose should be increased at an interval of four weeks. Patients without volume or salt depletion Treatment should be started with 15mg once daily and titrated upwards to achieve optimal blood pressure control. The usual effective dose is 30mg once daily. The maximum dose is 60mg per day administered in a single or two divided doses. Page 1 In case of inadequate response, other antihypertensive agents such as diuretics may be added (see sections 4.3, 4.4, 4.5 and 5.1). Patients suspected of volume or salt depletion First-dose hypotension may occur in high risk patients (see section 4.4).