Magnetic Resonance Findings in the Carpus and Proximal Metacarpal Region of Non-Lame Horses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Articulationes Membri Thoracici • 1. Articulatio
ARTICULATIONES MEMBRI THORACICI • 1. ARTICULATIO HUMERI-art. simplex, art. spheroidea (but functions as a hinge joint) movement: eq, Ru only flexion, extension is possible, in ca: rotation, abduction, adduction also between scapula (cavitas glenoidalis) and humerus (caput) Capsula articularis Recessus: cranial and caudal recesses Labrum glenoidale Ligg. glenohumeralia (eq, ca)- tickened part of the capsule (capsular ligament) in the med. and lat. walls in ca, and cranially in eq Lig. coracohumerale (eq, Ru)- capsular ligament between scapula (tub. supraglenoidale) and humerus (tub. majus, minus) No collateral ligaments! Instead of them: laterally m. infraspinatus (1), medially m. subscapularis (5) ca: part of the joint capsule surrounds the tendon of m. biceps brachii (9) and forms vagina synovialis intertubercularis eq, bo: bursa intertubercularis (=bursa bicipitalis) under the tendor of the m. biceps brachii (may communicate with the joint cavity of the shoulder joint in horse) • 2.ARTICULATIO CUBITI-art. composita, ginglymus (hinge joint) movement: extension and flexion between humerus (condyle), radius (caput), ulna (insisura trochlearis) Articulatio humeroulnaris Articulatio humeroradialis Capsula articularis Recessus: recessus cranialis, large recessus caudalis Lig. collaterale cubiti mediale- from epicondylus med. to radius (in ca also to ulna) Lig. collaterale cubiti laterale- from epicondylus lat. to radius (in ca, Ru also to ulna) Lig. olecrani (ca)- capsular ligament from fossa olecrani of humerus to olecranon •3. ARTICULATIO RADIOULNARIS PROXIMALIS- art. simplex, art. trochoidea movement: ca: rotational movements are possible (pronatio, supinatio) eq, Ru: no movement! between radius (circumferentia articularis radii) and ulna (incisura radialis ulnae) Lig. anulare radii (ca)- encircles the head of the radius, running under the collateral ligaments Membrana interossea antebrachii (ca) (in eq, Ru it is ossified) • 4. -

Orthopaedics Instructions: to Best Navigate the List, First Download This PDF File to Your Computer
Orthopaedics Instructions: To best navigate the list, first download this PDF file to your computer. Then navigate the document using the bookmarks feature in the left column. The bookmarks expand and collapse. Finally, ensure that you look at the top of each category and work down to review notes or specific instructions. Bookmarks: Bookmarks: notes or specific with expandable instructions and collapsible topics As you start using the codes, it is recommended that you also check in Index and Tabular lists to ensure there is not a code with more specificity or a different code that may be more appropriate for your patient. Copyright APTA 2016, ALL RIGHTS RESERVED. Last Updated: 09/14/16 Contact: [email protected] Orthopaedics Disorder by site: Ankle Achilles tendinopathy ** Achilles tendinopathy is not listed in ICD10 M76.6 Achilles tendinitis Achilles bursitis M76.61 Achilles tendinitis, right leg M76.62 Achilles tendinitis, left leg ** Tendinosis is not listed in ICD10 M76.89 Other specified enthesopathies of lower limb, excluding foot M76.891 Other specified enthesopathies of right lower limb, excluding foot M76.892 Other specified enthesopathies of left lower limb, excluding foot Posterior tibialis dysfunction **Posterior Tibial Tendon Dysfunction (PTTD) is not listed in ICD10 M76.82 Posterior tibial tendinitis M76.821 Posterior tibial tendinitis, right leg M76.822 Posterior tibial tendinitis, left leg M76.89 Other specified enthesopathies of lower limb, excluding foot M76.891 Other specified enthesopathies of right lower limb, -

Skeleton of Hand Skeleton of the Hand with Bone Numbering Skeleton Of
Info 6001 Sliding joints at the shoulder allow all natural movements. 6008 Skeleton of hand True to life casting of a skeleton of the human hand. All hand bones are individual- ly mobile-mounted on wire. Ref.no. 6001 With stand Ref.no. 6001S (see image below) 6016 6021 Skeleton of the hand with bone numbering Model as 6001, but with additional numbe- Skeleton of arm with shoulder Skeleton of arm with shoulder ring of the individual hand bones. girdle girdle and muscle marking Ref.no. 6002 (not pictured) True to life casting of a skeleton of the True to life casting of a skeleton of the human arm. The rolling movements of the human arm. The rolling movements of the bones of the lower arm (pronation and bones of the lower arm (pronation and supination) and movements of the hand supination) and movements of the hand Hand with lower arm joint can be demonstrated. The hand is joint can be demonstrated. The hand is True to life casting of a skeleton of the mobilemounted on wire. mobile-mounted on wire. Including marking human hand. All hand bones are individual- Ref.no. 6016 of muscle origins and insertion points. ly mobile-mounted on wire. With radius and Ref.no. 6021 ulna. The rolling movements of the bones Skeleton of arm of the lower arm (pronation and supinati- Model as 6016, but without shoulder girdle. on) and movements of the hand joint can Ref.no. 6012 Skeleton of arm with muscle be demonstrated. marking Ref.no. 6008 Model as 6021, but without shoulder girdle Ref.no. -

(Bucked Shins) in the Flat Racing Horse: Prevalence, Diagnosis, Pathogenesis, and Associated Factors
Journal of Dairy, Veterinary & Animal Research Mini Review Open Access A review of dorsal metacarpal disease (bucked shins) in the flat racing horse: prevalence, diagnosis, pathogenesis, and associated factors Abstract Volume 5 Issue 6 - 2017 Dorsal metacarpal disease (DMD) is the most common cause of lostdays to training S Couch,1 BD Nielsen2 and racing in Thoroughbred racehorses. Colloquially termed ‘bucked’ or ‘sore’ shins, 1Royal (Dick) School of Veterinary Studies, University of this initially painful condition commonly occurs in the first season of training and can Edinburgh, United Kingdom raise welfare concerns. Clinical signs include pain with digital palpation and swelling 2Department of Animal Science, Michigan State University, USA on the dorsal, and sometimes dorso-medial, aspect of the third metacarpal (McIII). Periostitis and excessive growth of periosteal bone can be present as a response to Correspondence: Brian D Nielsen, Michigan State University, high strain cyclic fatigue. Whilst DMD can resolve with rest or reduced exercise, it Department of Animal Science, 474 S. Shaw Lane, East Lansing, can leave bone susceptible to future catastrophic fracture at the same site, particularly MI 48824 1225, USA, Tel 517 432 1378, Fax 517 353 1699, saucer fractures of the lamellar bone of the diaphysis. Some trainers continue to work Email [email protected] an animal through DMD, with the view that it will only happen once, but it can re- occur. Additionally, the animal is in discomfort and has a weakened skeletal system. Received: September 13, 2017 | Published: September 25, In vivo studies of the effects of cyclic strain on the skeletal system of Thoroughbreds 2017 are notoriously difficult, due to the many variables involved and in vitro studies cannot mimic true training and racing conditions. -

Clinical Medical Policy
CLINICAL MEDICAL POLICY Noninvasive Electrical Bone Growth Stimulators Policy Name: (osteogenesis stimulators) Policy Number: MP-070-MD-PA Responsible Department(s): Medical Management Provider Notice Date: 12/15/2018 Issue Date: 01/15/2019 Effective Date: 01/15/2019 Annual Approval Date: 10/17/2019 Revision Date: N/A Products: Gateway Health℠ Medicaid Application: All participating hospitals and providers Page Number(s): 1 of 78 DISCLAIMER Gateway Health℠ (Gateway) medical policy is intended to serve only as a general reference resource regarding coverage for the services described. This policy does not constitute medical advice and is not intended to govern or otherwise influence medical decisions. POLICY STATEMENT Gateway Health℠ may provide coverage under the medical-surgical and DME benefits of the Company’s Medicaid products for medically necessary noninvasive electrical bone growth stimulators as treatment of nonunion long bone fractures or congenital pseudarthrosis. This policy is designed to address medical necessity guidelines that are appropriate for the majority of individuals with a particular disease, illness or condition. Each person’s unique clinical circumstances warrant individual consideration, based upon review of applicable medical records. (Current applicable Pennsylvania HealthChoices Agreement Section V. Program Requirements, B. Prior Authorization of Services, 1. General Prior Authorization Requirements.) Policy No. MP-070-MD-PA Page 1 of 78 DEFINITIONS Prior Authorization Review Panel - A panel of representatives from within the PA Department of Human Services who have been assigned organizational responsibility for the review, approval and denial of all PH-MCO Prior Authorization policies and procedures. Non-invasive (Osteogenic) Electrical Bone Growth Stimulator – A device that uses pulsed- electromagnetic fields, capacitative coupling or combined magnetic fields to generate a weak electric current through the target site. -

Fractures of Hamate: a Clinical Overview
MUSCULOSKELETAL SURGERY (2019) 103:15–21 https://doi.org/10.1007/s12306-018-0543-y REVIEW Fractures of hamate: a clinical overview G. Mouzopoulos1 · C. Vlachos1 · L. Karantzalis1 · K. Vlachos1 Received: 28 June 2017 / Accepted: 20 May 2018 / Published online: 29 May 2018 © Istituto Ortopedico Rizzoli 2018 Abstract Hamate fractures are exceedingly rare clinical entities. However, the diagnosis and treatment of these injuries are often delayed and can severely handicap the performance of afected laborers or athletes. This review focuses on fractures of the hamate and provides an update on the current consensus as to mechanism, diagnosis, management, and complications after such injuries. Keywords Hamate · Hook · Fracture Epidemiology the hook of the hamate [2]. If the grip is relaxed or control is lost, the fracture occurs at the end of a poor swing, as Fractures of the hamate usually occur through the hook centrifugal force is transmitted through the handle of the or body of the bone [1]. Type I fractures involve the hook racquet against the hook [7]. In golfers or baseball players, of the hamate and further are subdivided into three sub- a dubbed shot or a checked swing will fracture the hamulus types involving: base, waist, and avulsion (tip). Fractures because the butt of the club or bat will strike the hook. It has located at the base and proximal third (76%) of the hook also been described in polo and ice hockey [8]. are presented more frequently than fractures located at the Fall on an outstretched hand causing sudden forcible mid-third (13%) or the distal third (11%). -

Fractures of the Neck of the Fifth Metacarpal Bone. Medium-Term Results in 28 Cases Treated by Percutaneous Transverse Pinning I
Injury, Int. J. Care Injured 43 (2012) 242–245 Contents lists available at SciVerse ScienceDirect Injury jo urnal homepage: www.elsevier.com/locate/injury Fractures of the neck of the fifth metacarpal bone. Medium-term results in 28 cases treated by percutaneous transverse pinning V. Potenza *, R. Caterini, F. De Maio, S. Bisicchia, P. Farsetti Department of Orthopaedic Surgery, University of Rome ‘Tor Vergata’, Rome, Italy A R T I C L E I N F O A B S T R A C T Article history: The purpose of this study was to report the medium-term results in 28 patients affected by closed Accepted 27 October 2011 displaced fractures of the neck of the fifth metacarpal bone (boxer’s fracture) with an associated severe swelling of the hand, who were treated with percutaneous transverse K-wire pinning, to verify the Keywords: effectiveness of this surgical treatment. We opted for this treatment in all cases in which malrotation of Boxer’s fracture the fifth finger and volar angulation of the metacarpal head greater than 308 were associated with a Transverse pinning severe swelling of the hand. All the patients were reviewed clinically and radiologically at an average of Metacarpal neck fracture 25 months after surgery. At the final follow-up, no patient reported residual pain. All patients had full extension of the fifth finger, except two in whom we observed a limitation of the extension of the fifth metacarpophalangeal (MP) joint of about 108, without significant impairment of hand function. All patients had at least 908 flexion of the fifth MP joint and full range of motion of the interphalangeal (IP) joints. -

Functional Anatomy of the Equine Musculoskeletal System
1 CHAPTER Functional Anatomy of the Equine Musculoskeletal System ANNA DEE FAILS ANATOMIC NOMENCLATURE AND USAGE Foot Veterinary medical anatomists have been using the The foot consists of the hoof and all it encloses: the Nomina Anatomica Veterinaria, created by the Inter connective tissue corium (dermis), digital cushion, distal national Committee on Veterinary Gross Anatomical phalanx (coffin bone), most of the cartilages of the distal Nomenclature since 1968 to standardize the names of phalanx, distal interphalangeal (coffin) joint, distal part anatomical structures.46 This chapter endeavors to use the of the middle phalanx (short pastern bone), distal sesa most current, correct terms as outlined in that publication. moid (navicular) bone, podotrochlear bursa (navicular Nonetheless, equine practitioners need to be equally fluent bursa), several ligaments, tendons of insertion of the in older terminology, which is likely to be in wide usage common digital extensor and deep digital flexor mus among horse owners and equine professionals. This chap cles, blood vessels, and nerves. Skin between the heels is ter will provide useful and common synonyms for many also part of the foot. structures, along with their more technically correct terms. Figure 1.1 provides the directional terms for veteri HOOF WALL, SOLE, AND FROG nary anatomy that will be used in this chapter. With the exception of the ocular and oral cavity structures, the The hoof is continuous with the epidermis at the cor terms anterior, posterior, superior, and inferior are not onet, and the underlying corium of the hoof is likewise applicable to quadrupeds. continuous with the dermis of the skin. -
PN4 (SL) Carpal Tunnel Syndrome and Ulnar Nerve Entrapment.Pdf
CARPAL TUNNEL SYNDROME AND CUBITAL TUNNEL SYNDROME Shelly Lwu Dr. Midha Oct. 24, 2008 Chronic Nerve Compression ¨ Injury to blood-nerve barrier → subperineurial edema ¨ Thickening of external & internal epineurium ¨ Renaut’s bodies seen in areas of compression following traction or repetitive motion ¨ Large myelinated fibers demonstrate segmental demyelination & unmyelinated fibers progressively degenerate ¨ With long-standing compression, wallerian degeneration may occur ¨ Clinically, patients at this point experience muscle atrophy & severe loss of sensation Chronic Nerve Compression Carpal Tunnel Syndrome Epidemiology ¨ Most common entrapment neuropathy ¨ Incidence: 125:100,000 ¨ Affects1% in general population ¤ Usually people who use their hands extensively in their jobs or daily activities – repetitive movements ¨ F:M 2.5:1 ¨ >50% between ages 40 & 60 ¨ Dominant hand most often affected ¤ Bilateral in10% of patients Clinical Presentation: History ¨ Insidious onset ¨ Numbness, tingling, or aching in radial half of hand & lateral 3 ½ digits ¤ Entire hand may be involved ¨ Waking in the middle of the night w/ paresthesias & numbness – patient must shake or rub hand to obtain relief – characteristic ¤ ? Hypotonia results in venous stasis ¨ Clumsiness or weakness of the involved hand ¨ Symptoms usually aggravated by activity / repeated wrist flexion ¨ May occasionally present w/ forearm, arm, & shoulder pain radiating from wrist Clinical Presentation: Physical Exam ¨ Advanced disease: ¤ Decreased sensation to pain or light touch in radial -

An Anomalous Bilateral Muscle in Guyon's Canal Found During
Folia Morphol. Vol. 69, No. 1, pp. 65–67 Copyright © 2010 Via Medica C A S E R E P O R T ISSN 0015–5659 www.fm.viamedica.pl An anomalous bilateral muscle in Guyon’s canal found during cadaver study P. Depukat, E. Mizia, J. Walocha Chair of Anatomy, Faculty of Medicine, Jagiellonian University, Cracow, Poland [Received 23 November 2009; Accepted 9 December 2009] During anatomical dissection, an unusual bilateral muscle in the region of Guy- on’s canal was found in a 29-year-old human male cadaver. It originated from the pisiform bone and inserted to the flexor retinaculum. The muscle passed between the superficial and deep branch of the ulnar nerve. The ulnar artery passed anteriorly to the muscle. This work reports this finding and tries to cat- egorise it in one of the groups following the literature. (Folia Morphol 2010; 69, 1: 65–67) Key words: accessory muscle, wrist, variations INTRODUCTION lum. In both wrists it was 18.2 mm long and 5.2 mm The occurrence of anomalous hand muscles in wide. The muscle passed between the superficial and the region of the wrist is a rather common event. deep branch of the ulnar nerve. The ulnar nerve di- Usually authors classify them as accessory abductor vided 7.2 mm proximally to the proximal end of the digiti minimi (ADM), flexor digiti minimi brevis pisiform bone. The ulnar artery passed superficially (FDMB), or palmaris longus [1–12]. This work reports to the muscle while the deep branch of the ulnar a rarely seen type of accessory muscle. -

Developing Learning Models to Teach Equine Anatomy and Biomechanics
The University of Maine DigitalCommons@UMaine Honors College Spring 5-2017 Developing Learning Models to Teach Equine Anatomy and Biomechanics Zandalee E. Toothaker University of Maine Follow this and additional works at: https://digitalcommons.library.umaine.edu/honors Part of the Animal Sciences Commons, and the Veterinary Anatomy Commons Recommended Citation Toothaker, Zandalee E., "Developing Learning Models to Teach Equine Anatomy and Biomechanics" (2017). Honors College. 453. https://digitalcommons.library.umaine.edu/honors/453 This Honors Thesis is brought to you for free and open access by DigitalCommons@UMaine. It has been accepted for inclusion in Honors College by an authorized administrator of DigitalCommons@UMaine. For more information, please contact [email protected]. DEVELOPING LEARNING MODELS TO TEACH EQUINE ANATOMY AND BIOMECHANICS By Zandalee E. Toothaker A Thesis Submitted in Partial Fulfillment of the Requirements for a Degree with Honors (Animal and Veterinary Science) The Honors College University of Maine May 2017 Advisory Committee: Dr. Robert C. Causey, Associate Professor of Animal and Veterinary Sciences, Advisor Dr. David Gross, Adjunct Associate Professor in Honors (English) Dr. Sarah Harlan-Haughey, Assistant Professor of English and Honors Dr. Rita L. Seger, Researcher of Animal and Veterinary Sciences Dr. James Weber, Associate Professor and Animal and Veterinary Sciences © 2017 Zandalee Toothaker All Rights Reserved ABSTRACT Animal owners and professionals benefit from an understanding of an animal’s anatomy and biomechanics. This is especially true of the horse. A better understanding of the horse’s anatomy and weight bearing capabilities will allow people to treat and prevent injuries in equine athletes and work horses. -
ICD-10 Codes for Trigger Point Injections
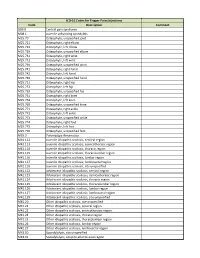
ICD-10 Codes for Trigger Point Injections Code Description Comment G89.0 Central pain syndrome M08.1 Juvenile ankylosing spondylitis M25.70 Osteophyte, unspecified joint M25.721 Osteophyte, right elbow M25.722 Osteophyte, left elbow M25.729 Osteophyte, unspecified elbow M25.731 Osteophyte, right wrist M25.732 Osteophyte, left wrist M25.739 Osteophyte, unspecified wrist M25.741 Osteophyte, right hand M25.742 Osteophyte, left hand M25.749 Osteophyte, unspecified hand M25.751 Osteophyte, right hip M25.752 Osteophyte, left hip M25.759 Osteophyte, unspecified hip M25.761 Osteophyte, right knee M25.762 Osteophyte, left knee M25.769 Osteophyte, unspecified knee M25.771 Osteophyte, right ankle M25.772 Osteophyte, left ankle M25.773 Osteophyte, unspecified ankle M25.774 Osteophyte, right foot M25.775 Osteophyte, left foot M25.776 Osteophyte, unspecified foot M35.3 Polymyalgia rheumatica M41.112 Juvenile idiopathic scoliosis, cervical region M41.113 Juvenile idiopathic scoliosis, cervicothoracic region M41.114 Juvenile idiopathic scoliosis, thoracic region M41.115 Juvenile idiopathic scoliosis, thoracolumbar region M41.116 Juvenile idiopathic scoliosis, lumbar region M41.117 Juvenile idiopathic scoliosis, lumbosacral region M41.119 Juvenile idiopathic scoliosis, site unspecified M41.122 Adolescent idiopathic scoliosis, cervical region M41.123 Adolescent idiopathic scoliosis, cervicothoracic region M41.124 Adolescent idiopathic scoliosis, thoracic region M41.125 Adolescent idiopathic scoliosis, thoracolumbar region M41.126 Adolescent idiopathic