Cardiothoracic Learning Package (Liverpool)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download PDF File
Folia Morphol. Vol. 78, No. 2, pp. 283–289 DOI: 10.5603/FM.a2018.0077 O R I G I N A L A R T I C L E Copyright © 2019 Via Medica ISSN 0015–5659 journals.viamedica.pl Observations of foetal heart veins draining directly into the left and right atria J.H. Kim1, O.H. Chai1, C.H. Song1, Z.W. Jin2, G. Murakami3, H. Abe4 1Department of Anatomy and Institute of Medical Sciences, Chonbuk National University Medical School, Jeonju, Korea 2Department of Anatomy, Wuxi Medical School, Jiangnan University, Wuxi, China 3Division of Internal Medicine, Jikou-kai Clinic of Home Visits, Sapporo, Japan 4Department of Anatomy, Akita University School of Medicine, Akita, Japan [Received: 19 June 2018; Accepted: 8 August 2018] Evaluation of semiserial sections of 14 normal hearts from human foetuses of gestational age 25–33 weeks showed that all of these hearts contained thin veins draining directly into the atria (maximum, 10 veins per heart). Of the 75 veins in these 14 hearts, 55 emptied into the right atrium and 20 into the left atrium. These veins were not accompanied by nerves, in contrast to tributaries of the great cardiac vein, and were negative for both smooth muscle actin (SMA) and CD34. However, the epithelium and venous wall of the anterior cardiac vein, the thickest of the direct draining veins, were strongly positive for SMA and CD34, respectively. In general, developing fibres in the vascular wall were positive for CD34, while the endothelium of the arteries and veins was strongly positive for the present DAKO antibody of SMA. -

The Variability of the Small Cardiac Vein in the Adult Human Heart
Folia Morphol. Vol. 63, No. 2, pp. 159–162 Copyright © 2004 Via Medica O R I G I N A L A R T I C L E ISSN 0015–5659 www.fm.viamedica.pl The variability of the small cardiac vein in the adult human heart Monika Cendrowska-Pinkosz Department of Anatomy, University Medical School, Lublin, Poland [Received 5 February 2003; Revised 25 November 2003; Accepted 31 December 2003] Direct analyses were performed on 50 hearts submitted for post mortem exam- ination. The remaining hearts were examined by the corrosion method. The aim of the work was to assess the morphology of the small cardiac vein. The small cardiac vein, which runs along the back surface of the coronary sulcus, would usually drain into the coronary sinus at its right side (86% of cases). Cases of the small cardiac vein draining into the middle cardiac vein were also noticed (12%) or directly into the right atrium (1%). In 1% of the preparations it ran along the right margin in the direction of the apex of the heart. In 30% of the corrosion preparations the small cardiac vein was not accessible with the help of corrosion. In 24% of the dissection preparations it was not possible to reach the small cardiac vein with the help of dissection. A statisti- cally significant relationship was observed between the frequency of the pres- ence or absence of the small cardiac vein and the sex of the donor (p > 0.001). In the group examined the percentage of men who did not have the small cardiac vein was 6 times higher than among the woman. -

A Case of the Bilateral Superior Venae Cavae with Some Other Anomalous Veins
Okaiimas Fol. anat. jap., 48: 413-426, 1972 A Case of the Bilateral Superior Venae Cavae With Some Other Anomalous Veins By Yasumichi Fujimoto, Hitoshi Okuda and Mihoko Yamamoto Department of Anatomy, Osaka Dental University, Osaka (Director : Prof. Y. Ohta) With 8 Figures in 2 Plates and 2 Tables -Received for Publication, July 24, 1971- A case of the so-called bilateral superior venae cavae after the persistence of the left superior vena cava has appeared relatively frequent. The present authors would like to make a report on such a persistence of the left superior vena cava, which was found in a routine dissection cadaver of their school. This case is accompanied by other anomalies on the venous system ; a complete pair of the azygos veins, the double subclavian veins of the right side and the ring-formation in the left external iliac vein. Findings Cadaver : Mediiim nourished male (Japanese), about 157 cm in stature. No other anomaly in the heart as well as in the great arteries is recognized. The extracted heart is about 350 gm in weight and about 380 ml in volume. A. Bilateral superior venae cavae 1) Right superior vena cava (figs. 1, 2, 4) It measures about 23 mm in width at origin, about 25 mm at the pericardiac end, and about 31 mm at the opening to the right atrium ; about 55 mm in length up to the pericardium and about 80 mm to the opening. The vein is formed in the usual way by the union of the right This report was announced at the forty-sixth meeting of Kinki-district of the Japanese Association of Anatomists, February, 1971,Kyoto. -

G06, G12, G13 (1000263, 1000268, 1000269) 2 Latin
…going one step further G06 1000263 G13 1000269 G12 1000268 G06, G12, G13 (1000263, 1000268, 1000269) 2 Latin G12, G13: A Apex cordis B Septum interventriculare, pars muscularis I Atrium dextrum Ia Auricula dextra II Atrium sinistrum IIb Auricula sinistra III Ventriculus dexter IV Ventriculus sinister 1 V. cava superior 1a V. brachiocephalica sinistra 2 V. cava inferior 3 Valva atrioventricularis dextra (Valva tricuspidalis) 3a Mm. papillares 3b Valva trunci pulmonalis 4 Truncus pulmonalis 4a A. pulmonalis sinistra 4b A. pulmonalis dextra 5 Vv. pulmonales 6 Valva atrioventricularis sinistra (Valva mitralis) 6c Mm. papillares 6d Valva aortae 7 Pars ascendens aortae ® 7a Arcus aortae 7b Truncus brachiocephalicus 7c A. carotis communis sinistra 7d A. subclavia sinistra 8 A. coronaria dextra 8a R. interventricularis posterior a. coronariae dextrae 8b R. posterolateralis dexter a. coronariae dextrae 9a R. interventricularis anterior a. coronariae sinistrae 9b R. circumflexus a. coronariae sinistrae 9c R. lateralis a. coronariae sinistrae 10 Sinus coronarius 10a V. cardiaca magna 10b V. cardiaca parva 10c V. cardiaca media (V. interventricularis posterior) 10d Vv. ventriculi sinisteri posteriores 11 Sulcus coronarius 12 Sulcus interventricularis anterior 13 Sulcus interventricularis posterior G13: 14 Trachea 15 Oesophagus 3 Heart, 2-times life size English G12, G13: A Apex of heart B Muscular part of interventricular septum I Right atrium Ia Right auricle II Left atrium IIb Left auricle III Right ventricle IV Left ventricle 1 Superior vena -

Superior Vena Cava Pulmonary Trunk Aorta Parietal Pleura (Cut) Left Lung
Superior Aorta vena cava Parietal pleura (cut) Pulmonary Left lung trunk Pericardium (cut) Apex of heart Diaphragm (a) © 2018 Pearson Education, Inc. 1 Midsternal line 2nd rib Sternum Diaphragm Point of maximal intensity (PMI) (b) © 2018 Pearson Education, Inc. 2 Mediastinum Heart Right lung (c) Posterior © 2018 Pearson Education, Inc. 3 Pulmonary Fibrous trunk pericardium Parietal layer of serous pericardium Pericardium Pericardial cavity Visceral layer of serous pericardium Epicardium Myocardium Heart wall Endocardium Heart chamber © 2018 Pearson Education, Inc. 4 Superior vena cava Aorta Left pulmonary artery Right pulmonary artery Left atrium Right atrium Left pulmonary veins Right pulmonary veins Pulmonary semilunar valve Left atrioventricular valve Fossa ovalis (bicuspid valve) Aortic semilunar valve Right atrioventricular valve (tricuspid valve) Left ventricle Right ventricle Chordae tendineae Interventricular septum Inferior vena cava Myocardium Visceral pericardium (epicardium) (b) Frontal section showing interior chambers and valves © 2018 Pearson Education, Inc. 5 Left ventricle Right ventricle Muscular interventricular septum © 2018 Pearson Education, Inc. 6 Capillary beds of lungs where gas exchange occurs Pulmonary Circuit Pulmonary arteries Pulmonary veins Venae Aorta and cavae branches Left atrium Left Right ventricle atrium Heart Right ventricle Systemic Circuit Capillary beds of all body tissues where gas exchange occurs KEY: Oxygen-rich, CO2-poor blood Oxygen-poor, CO2-rich blood © 2018 Pearson Education, Inc. 7 (a) Operation of the AV valves 1 Blood returning 4 Ventricles contract, to the atria puts forcing blood against pressure against AV valve cusps. AV valves; the AV valves are forced open. 5 AV valves close. 2 As the ventricles 6 Chordae tendineae fill, AV valve cusps tighten, preventing hang limply into valve cusps from ventricles. -

CARDIOLOGY PHYSIOLOGY Part 1 Describe the Adult Coronary Circulation the Left Main and Right Coronary Arteries Originate At
CARDIOLOGY PHYSIOLOGY Part 1 Describe the adult coronary circulation The left main and right coronary arteries originate at the base of the aorta, from the coronary ostia, which is located behind the aortic leaflets. These two arteries lie on the surface of the heart whereas the smaller arteries penetrate the epicardium and supply blood to the myocardium. The left main coronary artery arises from the posterior aortic sinus above the left coronary cusp of the aortic valve and has two main branches, the circumflex and the left anterior descending artery. The circumflex artery lies in the left atrioventricular groove and supplies most of the left atrium and the posterior and lateral parts of the left ventricle. It, also with the left anterior descending artery, supplies the anterolateral papillary muscle. The circumflex artery has several branches including; atrial branches and obtuse marginal branches 1, 2 and 3. In 10% of people the circumflex supplies the posterior descending artery, this is termed ‘left dominant circulation’. Also, in 40% of the population, the circumflex supplies the sinoatrial node. The left anterior descending artery, which is also known as the anterior interventricular branch, follows the anterior interventricular sulcus down to the apex of the heart where it often anastomoses with the terminal branches of the posterior descending artery. It supplies the anterolateral portions of the heart, the anterior 2/3 of the interventricular septum. Important branches include the diagonal branches, which run laterally to supply the anterolateral wall of the LV, and the septal branches which supplies the anterior 2/3 of the interventricular septum. -

Thorax-Heart-Blood-Supply-Innervation.Pdf
Right coronary artery • Originates from the right aortic sinus of the ascending aorta. Branches: • Atrial branches sinu-atrial nodal branch, • Ventricular branches • Right marginal branch arises at the inferior margin of the heart and continues along this border toward the apex of the heart; • Posterior interventricular branch- lies in the posterior interventricular sulcus. The right coronary artery supplies • right atrium and right ventricle, • sinu-atrial and atrioventricular nodes, • the interatrial septum, • a part of the left atrium, • the posteroinferior one-third of the interventricular septum, • a part of the posterior part of the left ventricle. Left coronary artery • from the left aortic sinus of the ascending aorta. The artery divides into its two terminal branches: • Anterior interventricular branch (left anterior descending artery- LAD), descends obliquely toward the apex of the heart in the anterior interventricular sulcus, one or two large diagonal branches may arise and descend diagonally across the anterior surface of the left ventricle; • Circumflex branch, which courses in the coronary sulcus and onto the diaphragmatic surface of the heart and usually ends before reaching the posterior interventricular sulcus-a large branch, the left marginal artery, usually arises from it and continues across the rounded obtuse margin of the heart. Coronary distribution Coronary anastomosis Applied Anatomy • Myocardial infarction Occlusion of a major coronary artery leads to an inadequate oxygenation of an area of myocardium and cell death. The severity depends on: size and location of the artery Complete or partial blockage (angina) • Coronary angioplasty • Coronary artery bypass grafting Cardiac veins The coronary sinus receives four major tributaries: • Great cardiac vein begins at the apex of the heart. -

Cardiovascular System Cardiovascular System the Heart
2/20/2016 Cardiovascular System • Blood • Heart The Cardiovascular System • Blood vessels Part 1 Cardiovascular System The Heart • Functions • Four separate chambers in humans –Transport gases, wastes, food, hormones, blood cells – Also other mammals, birds • Systems affected • Double pump two closed circuits – Respiratory • 5 L/minute –Urinary –Digestive –Musculoskeletal –Immune system Capillary beds of lungs where The Heart gas exchange occurs Pulmonary Circuit • Symmetrical in design, but not in position Pulmonary veins Pulmonary arteries Aorta and branches – 2/3 of mass to the left of midline Venae cavae Left atrium – 1/3 to right Right atrium Left ventricle Heart Right ventricle Systemic Circuit Oxygen-rich, Capillary beds of all CO 2-poor blood body tissues where Oxygen-poor, gas exchange occurs CO 2-rich blood Figure 18.5 1 2/20/2016 Located within mediastinum Midsternal line Superior Aorta vena cava Parietal 2nd rib pleura (cut) Pulmonary Left lung Sternum trunk Pericardium Diaphragm Point of (cut) maximal Apex of intensity Diaphragm heart (PMI) (a) (c) Figure 18.1a Figure 18.1c Pericardium Pericardium – –Membrane surrounding and protecting the heart Double walled organ • Confines while still allowing free movement • Fibrous pericardium • Serous pericardium Pericardium Pericardium –Double walled organ –Double walled organ • Fibrous pericardium • Fibrous pericardium –Fibrous connective tissue • Serous pericardium –Prevents overstretching, protection, anchorage –Serous epithelium • Serous pericardium –Double layer » Parietal layer -

Heart and Respiratory System Study Guide
Comenius University in Bratislava Jessenius Faculty of Medicine in Martin Department of Anatomy HEART AND RESPIRATORY SYSTEM STUDY GUIDE Desanka Výbohová Gabriela Hešková Yvetta Mellová Martin 2019 1 Authors: Doc. MUDr. Desanka Výbohová, PhD. MUDr. Gabriela Hešková, PhD. Doc. MUDr. Yvetta Mellová, CSc. Authors themselves are responsible for the content and English of the chapters. Reviewers: Prof. MUDr. Marian Adamkov, DrSc. MUDr. Zuzana Lazarová, PhD. ISBN 978-80-8187-065-1 EAN 9788081870651 2 TABLE OF CONTENT Preface.................................................................................................................................6 HEART................................................................................................................................ 7 Position of the heart...............................................................................................................7 Relations of the heart...........................................................................................................10 External features of the heart...............................................................................................13 Pericardium..........................................................................................................................18 Cardiac wall.........................................................................................................................22 Cardiac skeleton...................................................................................................................23 -
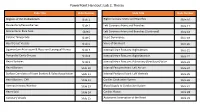
Powerpoint Handout: Lab 2, Thorax
PowerPoint Handout: Lab 2, Thorax Slide Title Slide Number Slide Title Slide Number Regions of the Mediastinum Slide 2 Right Coronary Artery and Branches Slide 16 Pericardium/Pericardial Sac Slide 3 Left Coronary Artery and Branches Slide 17 Pericardium: Bare Area Slide4 Left Coronary Artery and Branches (Continued) Slide 18 Cardiac Tamponade Slide 5 Heart Dominance Slide 19 Heart Great Vessels Slide 6 Veins of the Heart Slide 20 Ligamentum Arteriosum & Recurrent Laryngeal Nerves Slide 7 Internal Heart Features: Right Atrium Slide 21 Pericardial Cavity Sinuses Slide 8 Internal Heart Features: Right Ventricle Slide 22 Heart Surfaces Slide 9 Internal Heart Features: Pulmonary (Semilunar) Valve Slide 23 Heart Borders Slide 10 Internal Features Heart: Left Atrium Slide 24 Surface Correlates of Heart Borders & Valve Auscultation Slide 11 Internal Features Heart: Left Ventricle Slide 25 Heart Borders: CXR Slide 12 Cardiac Conduction System Slide 26 Aortopulmonary Window Slide 13 Blood Supply to Conduction System Slide 27 Heart Sulci Slide 14 Cardiac Plexus Slide 28 Coronary Vessels Slide 15 Autonomic Innervation of the Heart Slide 29 Regions of the Mediastinum The transverse thoracic plane passing through the sternal angle (commonly intersecting the T4/T5 intervertebral disc) divides the mediastinum into two subdivisions. • The superior mediastinum spans the space between superior thoracic aperture and transverse thoracic plane. • The inferior mediastinum spans the space between the transverse thoracic Structures Within Each region of the Mediastinum plane and the diaphragm. It can be further divided into the following regions. Superior Mediastinum • The anterior mediastinum is the smallest subdivision of the • Aortic arch and its branches mediastinum. -
![The Heart & Pericardium 2 [PDF]](https://docslib.b-cdn.net/cover/1484/the-heart-pericardium-2-pdf-8031484.webp)
The Heart & Pericardium 2 [PDF]
The Heart & Pericardium Dr. Rakesh Kumar Verma Assistant Professor Department of Anatomy KGMU UP Lucknow DR.RAKESH VERMA,AP,ANATOMY. KGMU,UP Lko Fibrous skeleton • Dense fibrous connective A tissue forms a structural foundation around AV & arterial orifices. • It is site of attachment to atria & ventricles. L R • Musculature of atria & ventricles does not cross this fibrous ring. • It is also an electrical insulator between atria and ventricles except via AV Bundle/Bundle P of His. DR.RAKESH VERMA,AP,ANATOMY. KGMU,UP Lko Conduction system – Specialized cardiac muscle fibers – Self-excitable – Repeatedly generate action potentials that trigger heart contractions – Act as pacemaker & Form conduction system – Consist of SA , AV Node,Bundle of His & Purkinje fibers DR.RAKESH VERMA,AP,ANATOMY. KGMU,UP Lko Conduction System • SA node acts as natural pacemaker – Faster than other auto rhythmic fibers – Initiates 100 times per second • Nerve impulses from autonomic nervous system (ANS) and hormones modify timing and strength of each heartbeat DR.RAKESH VERMA,AP,ANATOMY. KGMU,UP Lko Conduction system 1. Begins in sinoatrial (SA) node in right atrial wall • Propagates through atria via gap junctions • Atria contact 2. Reaches atrioventricular (AV) node in interatrial septum 3. Enters atrioventricular (AV) bundle (Bundle of His) • Only site where action potentials can conduct from atria to ventricles due to fibrous skeleton 4. Enters right and left bundle branches which extends through interventricular septum toward apex 5. Finally, large diameter Purkinje fibers conduct action potential to remainder of ventricular myocardium DR.RAKESH VERMA,AP,ANATOMY. KGMU,UP Lko Frontal plane Left atrium RightRight atriumatrium 1 SINOATRIAL (SA) NODE 2 ATRIOVENTRICULAR (AV) NODE 3 ATRIOVENTRICULAR (AV) BUNDLE (BUNDLE OF HIS) Left ventricle 4 RIGHT AND LEFT BUNDLE BRANCHES RightRight ventricleventricle 5 PURKINJE FIBERS DR.RAKESH VERMA,AP,ANATOMY. -

Morphological Study of Middle Cardiac Vein in Human Hearts of North Western up and Its Application for Interventional Procedure
Indian Journal of Clinical Anatomy and Physiology 2020;7(2):130–133 Content available at: iponlinejournal.com Indian Journal of Clinical Anatomy and Physiology Journal homepage: www.innovativepublication.com Original Research Article Morphological study of middle cardiac vein in human hearts of north western UP and its application for interventional procedure Jolly Agarwal1,*, Anurag Agarwal2, D N Sinha3, Virendra Kumar4 1Dept. of Anatomy, Government Doon Medical College, Dehradun, Uttarakhand, India 2Dept. of TB & Chest, Government Doon Medical College, Dehradun, Uttarakhand, India 3Dept. of Anatomy, Government Medical College & Hospital, Haldwani, Uttarakhand, India 4Dept. of Anatomy, Government Medical College, Shahjahanpur, Uttar Pradesh, India ARTICLEINFO ABSTRACT Article history: Background: The aim of present study was to study morphology of middle cardiac vein in human hearts. Received 13-05-2020 Materials and Methods: The study was conducted on middle cardiac vein of thirty human hearts with due Accepted 16-05-2020 clearance from ethical committee. Available online 27-06-2020 Results: The mean diameter of middle cardiac vein was 2.57 1.16 mm and the mean length was 74.69 21.10 mm. There was also statistically significant relationship between length of middle cardiac vein and weight of cadaver. In some hearts middle cardiac vein and small cardiac vein together form common trunk Keywords: and then drain into coronary sinus. Cardiac Conclusion: Middle cardiac vein can be used for radio frequency ablation of a posteroseptal pathway. It Vein can also be used for newer interventional technique such as selective catheterization. It may be one of the Middle choices of implantation of pacing leads.